1. Centers for Disease Control and Prevention (CDC). Social Determinants of Health at CDC. Website. https://www.cdc.gov/socialdeterminants/about.html. Published March 10, 2021. Accessed August 28, 2021.
2. Agency for Toxic Substances and Disease Registry (ATSDR). CDC/ATSDR’s Social Vulnerability Index. Website. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Updated April 28, 2021. Accessed September 6, 2021.
3. Kim HK, Ahn J, Atkinson L, Kahlor LA. Effects of Covid-19 misinformation on information seeking, avoidance, and Processing: A multicountry comparative study. Sci Commun. 2020; 42(5): 586-615. doi: 10.1177/1075547020959670
4. Centers for Disease Control and Prevention (CDC). Understanding Risk. Website. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/assessing-risk-factors.html. Published August 5, 2021. Accessed September 4, 2021.
5. Centers for Disease Control and Prevention (CDC). Advancing Health Equity in Chronic Disease Prevention and Management. Website. http://www.cdc.gov/chronicdisease/healthequity/index.htm. Updated March 11, 2020. Accessed August 21, 2021.
6. Papageorge NW, Zahn MV, Belot M, et al. Socio-demographic factors associated with self-protecting behavior during the Covid-19 pandemic. J Popul Econ. 2021; 34(2): 691-738. doi: 10.1007/s00148-020-00818-x
7. Geçer E, Yıldırım M, Akgül Ö. Sources of information in times of health crisis: Evidence from Turkey during COVID-19. J Public Health (Berl.). 2020; 30: 1113-1119. doi: 10.1007/s10389-020-01393-x
8. Obiała J, Obiała K, Mańczak M, Owoc J, Olszewski R. COVID-19 misinformation: Accuracy of articles about CORONAVIRUS prevention mostly shared on social media. Health Policy Technol. 2021; 10(1): 182-186. doi: 10.1016/j.hlpt.2020.10.007
9. Gerts D, Shelley CD, Parikh N, et al. “Thought I’d Share First”: an analysis of COVID-19 conspiracy theories and misinformation spread on twitter. JMIR Public Health Surveill. 2021; 7(4): e26527. doi: 10.2196/26527
10. Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among healthcare professionals and its influence on healthcare outcomes: A systematic review. Am J Public Health. 2015; 105(12): 2588-2588. doi: 10.2105/ajph.2015.302903a
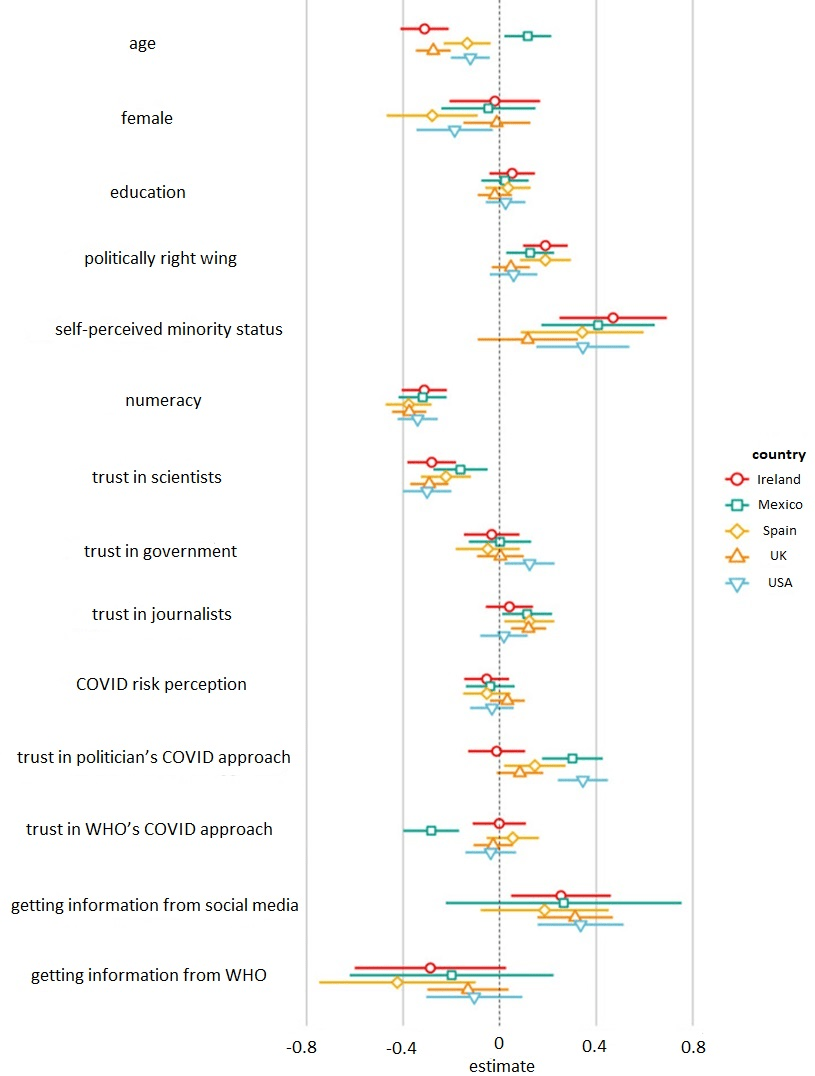
11. Roozenbeek J, Schneider CR, Dryhurst S, et al. Susceptibility to misinformation about COVID-19 around the world. R. Soc. Open Sci. 2020; 7(10): 201199. doi: 10.1098/rsos.201199
12. Viswanath K, Lee EW, Pinnamaneni R. We need the lens of equity in COVID-19 Communication. Health Commun. 2020; 35(14): 1743-1746. doi: 10.1080/10410236.2020.1837445
13. Al-Zaman MS. Social media and COVID-19 misinformation: How ignorant Facebook users are? Heliyon. 2021; 7(5): e07144. doi: 10.1016/j.heliyon.2021.e07144
14. Pennycook G, Rand DG. Lazy, not biased: Susceptibility to partisan fake news is better explained by lack of reasoning than by motivated reasoning. Cognition. 2019; 188: 39-50. doi: 10.1016/j.cognition.2018.06.011
15. Buchanan T. Why do people spread false information online? The effects of message and viewer characteristics on self-reported likelihood of sharing social media disinformation. PLoS One. 2020; 15(10): e0239666. doi: 10.1371/journal.pone.0239666
16. Kumar S, Shah N. False information on web and social media: A survey. arXiv.org. Website. https://arxiv.org/abs/1804.08559. Published April 23, 2018. Accessed September 7, 2021.
17. Choi D, Chun S, Oh H, Han J, Kwon TT. Rumor Propagation is amplified by echo chambers in social media. Sci Rep. 2020; 10(1): 310. doi: 10.1038/s41598-019-57272-3
18. Krause NM, Freiling I, Beets B. Fact-checking as RISK communication: The MULTI-LAYERED risk of misinformation in times of COVID-19. J Risk Res. 2020; 23(7-8): 1052-1059. doi: 10.1080/13669877.2020.1756385
19. Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021; 39(7): 1080-1086. doi: 10.1016/j.vaccine.2021.01.010
20. Qiao S, Li Z, Liang C, Li X, Rudisill CA. Risk perception of COVID-19 and its socioeconomic correlates in the United States: A social media analysis. medRxiv. 2021; 2021.01.27.21250654. doi: 10.1101/2021.01.27.21250654
21. Seo H, Blomberg M, Altschwager D, Vu HT. Vulnerable populations, and misinformation: A mixed-methods approach to underserved older adults’ online information assessment. New Media Soc. 2021; 23(7): 2012-2033. doi: 10.1177/1461444820925041
22. De keersmaecker J, Roets A. ‘Fake news’: Incorrect, but hard to correct. the role of cognitive ability on the impact of false information on social impressions. Intelligence. 2017; 65: 107-110. doi: 10.1016/j.intell.2017.10.005
23. Christy SM, Gwede CK, Sutton SK, et al. Health literacy among medically Underserved: The role of demographic factors, social influence, and religious beliefs. J Health Commun. 2017; 22(11): 923-931. doi: 10.1080/10810730.2017.1377322
24. Enders AM, Uscinski JE, Klofstad C, Stoler J. The different forms of COVID-19 misinformation and their consequences. Har Kennedy Sch Misinformation Rev. 2020; 1(8). doi: 10.37016/mr-2020-48
25. Hildreth JEK, Alcendor DJ. Targeting COVID-19 vaccine hesitancy in minority populations in the US: Implications for herd immunity. Vaccines (Basel). 2021; 9(5): 489. doi: 10.3390/vaccines9050489
26. Kulkarni P, Prabhu S, Kumar S, Ramraj B. COVID-19- Infodemic OVERTAKING Pandemic? Time to DISSEMINATE facts over fear. Indian J Community Health. 2020; 32(2 (Supp): 264-268. doi: 10.47203/ijch.2020.v32i02supp.018
27. Lewandowsky S, Cook J, Ecke et al. Debunking Handbook 2020. NY, USA: New York University Library; 2020. doi: 10.17910/b7.1182
28. An L, Bacon E, Hawley S, et al. Relationship between coronavirus-related eHealth literacy and COVID-19 knowledge, attitudes, and practices among US adults: Web-based survey study. J Med Internet Res. 2021; 23(3): e25042. doi: 10.2196/25042
29. Norman CD, Skinner HA. eHealth literacy: Essential skills for consumer health in a networked world. J Med Internet Res. 2006; 8(2): e9. doi: 10.2196/jmir.8.2.e9
30. Guo Z, Zhao SZ, Guo N, et al. Socioeconomic disparities in eHealth literacy and preventive behaviors during the COVID-19 pandemic in Hong Kong: Cross-sectional study. J Med Internet Res. 2021; 23(4): e24577. doi: 10.2196/24577
31. Tichenor PJ, Donohue GA, Olien CN. Mass media flow and differential growth in knowledge. Public Opin Q. 1970; 34(2): 159-170. doi: 10.1086/267786
32. Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: A systematic review of eHealth literacy in underserved populations in the United States. Inform Health Soc Care. 2015; 41(1): 1-19. doi: 10.3109/17538157.2014.948171
33. Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and DIGITAL inequalities: Reciprocal impacts and mitigation strategies. Comput Human Behav. 2020; 111: 106424. doi: 10.1016/j.chb.2020.106424
34. Lin L, Savoia E, Agboola F, Viswanath K. What have we learned about communication inequalities during the H1N1 pandemic: A systematic review of the literature. BMC Public Health. 2014; 14: 484. doi: 10.1186/1471-2458-14-484
35. Ataguba OA, Ataguba JE. Social determinants of health: The role of effective communication in the COVID-19 pandemic in developing countries. Glob Health Action. 2020; 13(1): 1788263. doi: 10.1080/16549716.2020.1788263
36. Hughes B, Miller-Idriss C, Piltch-Loeb R, et al. Development of a codebook of online anti-vaccination rhetoric to manage COVID-19 vaccine misinformation. Int J Environ Res Public Health. 2021; 18(14): 7556. doi: 10.3390/ijerph18147556
37. Hoffman BL, Colditz JB, Shensa A, et al. #DoctorsSpeakUp: Lessons learned from a pro-vaccine Twitter event. Vaccine. 2021; 39(19): 2684-2691. doi: 10.1016/j.vaccine.2021.03.061
38. Gagneur A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can Commun Dis Rep. 2020; 46(4): 93-97. doi: 10.14745/ccdr.v46i04a06
39. World Health Organization (WHO). Coronavirus disease (COVID-19) advice for the public: Mythbusters. Website. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters. Updated May 5, 2021. Accessed September 7, 2021.
40. MacDonald NE; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015; 33(34): 4161-4164. doi: 10.1016/j.vaccine.2015.04.036