INTRODUCTION
Over the course of the next few months, the readers will be provided with a highly topical three part series of articles on the adverse impacts of alcohol on the human foetus, and thus on the offspring who suffer the consequences of the defects they inherit. The first task is to clarify the confusion surrounding the nomenclature used to describe this area of research. For example, there has been a misapprehension that the term ‘Foetal Alcohol Syndrome’ (FAS) has become antiquated and thus been replaced by the phrase, ‘Foetal Alcohol Spectrum Disorders, (FASD). The term FASD actually represents the overarching framework under which the different kinds of alcohol related abnormalities are categorized. FASD should not be construed or used as a clinical diagnosis, and from this it follows that it would be an inappropriate use of the term to diagnose an individual with FASD.1
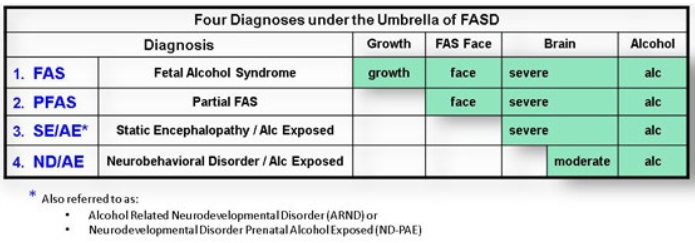
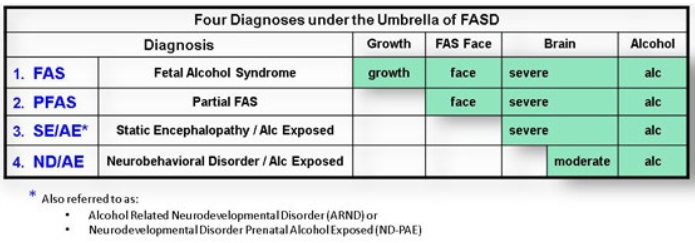
Quoting from a 2016 report by the FAS Diagnostic & Prevention Network, Washington D.C., USA, it is made explicit that: “Four diagnoses fall under the umbrella of FASD: FAS, Partial FAS, Static Encephalopathy/Alcohol Exposed (SE/AE) and Neurobehavioral Disorder/Alcohol Exposed (ND/AE). Each year, as many as 40,000 babies are born with one or more of these four disorders, at a cost of over $4 billion dollars nationwide”.2 To avoid any confusion, it is imperative to note that far from being phased out, the term ‘Foetal Alcohol Syndrome’ (FAS) describes the most severe form of the diagnosis and the widest range of abnormalities associated with what has been elsewhere called, “alcohol pregnancies”.3 One reason for this is that in addition to its shared diagnoses with the other categories listed, FAS also incorporates diagnoses of foetal alcohol growth defects.
Chart 1 is reproduced here from a 2016 report of the FAS Diagnostic & Prevention Network, Department of Health and Education, Washington, D.C., USA, 2016.2
Chart 1: Four Diagnoses that Fall Under the Umbrella of FASD.
Historical Background of Medical Concern with Alcohol Pregnancies
There has long been a suspicion in the literature of antiquity that the consumption of alcohol by pregnant women was likely to cause severe foetal and birth abnormalities. In the Bible, mothers-to-be were strongly counseled to abstain from drinking wine while they were pregnant. In the book of Judges, for example, it is written:
13:3 And the angel of the LORD appeared unto the woman, and said unto her, “Behold now, thou [art] barren, and barest not: but thou shalt conceive, and bear a son.”
13:4 Now therefore beware, I pray thee, and drink not wine nor strong drink, and eat not any unclean [thing].4
Although, there are many examples of antiquity of intuitive belief in the importance of pregnant women refraining from alcohol consumption, the scientific explorations of alcohol pregnancy were not journeyed until much later.
It was in the mid 1900’s that Dr. W.C. Sullivan, who was reputed to have delivered more than one hundred babies, admonished the medical community of the deleterious hazards of alcohol pregnancy. His extensive findings were published, establishing that there was a significantly higher incidence of stillbirth babies, miscarriage, and a statistically significant increase in the incidence of epilepsy amongst their surviving offspring, compared to pregnant women who did not drink whilst pregnant.5,6,7 In 1957, Rouquette on the same page submitted a doctoral dissertation in Medicine at the University of Paris entitled, “Influence of Parental Alcoholic Toxiomania on the Physical and Psychic Development of Young Children”. A decade later, the research of Dr. P. Lemoine, and other team researchers, reinforced and extended the conclusions of Rouquette by demonstrating that alcohol pregnancy clearly increases the rates of still birth, along with two new categories of adverse consequences, namely, growth deficiency, and malformations among the children of alcoholic women.8,9,10
Despite these initial investigations into the problem of teratogenesis (deformation of the foetus), there was little attention paid to finding this topic, until an article on the subject by Dr. K.L. Jones and colleagues was published on June 9th, 1973 in the Lancet, one of the most prestigious medical journals in the world. According to the article, sufficient evidence had accrued to demonstrate unequivocally that alcohol pregnancy produced a recognizable pattern of foetal malformation, which should be identified medically as ‘Foetal Alcohol Syndrome’ (FAS).11,12,13,14 Since the publication of this seminal paper, a vast amount of literature has accumulated to establish scientifically the deleterious effects on the foetus caused by alcohol consumption. By 1981, clinical characteristics of FAS had formally been documented to include the following symptoms:
- Prenatal and postnatal growth deficiency;
- Central nervous dysfunction;
- A particular pattern of distortion in relation to facial characteristics;
- Major organ system malformations: the organ systems affected by FAS include the heart, central nervous system, genitals, skin, liver, kidneys, muscular and skeletal system, and especially the brain14,15,16,17;
- It is the subsequent pattern and irregularities in the child’s growth, coupled with noticeable disruptions of functions of the child’s central nervous system that betrays the presence of FAS. In addition to low birth rate, infants with FAS commonly exhibit a smaller head circumference outside the range of the normal, and display bouts of hyper-excitability often leading to epileptic convulsions. Children with FAS are typically tiny with little fat developed under the skin, diminished muscular development and general muscular weakness. Malformations of the optic disk of the eye are common, with many children suffering a moderate or severe reduction in visual sharpness. Similarly, partial deafness is another symptom.18,19,20,21
Endeavoring to confirm that alcohol is highly toxic and irreparably damaging to the foetus, a research team in 2003 from the Division of Nursing, at the University of Arkansas-Monticello, collected and analyzed every available paper in relation to the actual biological degradation caused by FAS. Their investigation of these studies affirmed that alcohol is definitely a teratogen, and demonstrated that the more alcohol a woman consumes throughout her pregnancy, the higher the risk of the seriousness of the birth defects and abnormalities identified earlier by Dr. Jones.22 However, it is of paramount importance to realize that alcohol binges and intoxication can also impact indirectly on the medical integrity of a woman’s future pregnancy, even before she becomes pregnant. To comprehend why this is so, it is salutary to remember that the ovaries are two diminutive organs located on each side of the woman’s pelvis, and they produce and contain the female gamete cells known as an ova or the oocytes. Because the ovaries are sustained by blood supply, they are not immune to alcohol toxification. Indeed, evidence has now accumulated to show that episodes of binge drinking and intoxication, particularly those episodes that lead to and prolong the presence of alcohol in the bloodstream, have the potential to damage even the unfertilized eggs stored in the ovaries of women.23,24,25,26 This revelation is of extraordinary significance, and could plausibly explain a large portion of the births of children with a range of disabilities. Additional research needs to be conducted to determine the extent to which this phenomenon might adversely be affecting childbirth.
The range of deformations caused by FAS is truly lamentable and could possibly have been prevented or at least ameliorated with appropriate health education programs designed to help both women (and men), to realize and respect the gravity of excessive alcohol consumption both during and outside the context of pregnancy.