INTRODUCTION
Disease prevalence during pregnancy has a particular importance in the study of maternal well-being and neonatal outcomes. Women in their reproductive age and with chronic medical conditions have a greater risk of not only pre-mature death and long-term illnesses but also for pregnancy complications. Therefore, it is not surprising that women with chronic diseases are often anxious about pregnancy.1 Smoking, diabetes and hypertension increase the risk of pre-term delivery,2 whereas, smoking and obesity has led to the risk of infant birth defects.3,4
Chronic diseases and risk factors have been associated with maternal complications such as gestational diabetes, gestational hypertension and pre-eclampsia during pregnancy.5 Such previously existing complications or those developed during the pregnancy tend to get further aggravated by the physiological effects of pregnancy which may indirectly lead to maternal deaths.6 These include anemia, hypertension, diabetes, as well as infectious conditions of HIV and malaria. In developing countries, about 30% of maternal deaths occur due to indirect causes.7 The growing prevalence of lifestyle-related conditions contribute to the increased commonness of obesity. This also contributes to the growing list of health problems as obesity, diabetes mellitus, heart disease and hypertensive disorders.8 Women have also experienced increase in the prevalence of chronic disease related risk factors such as obesity, diabetes, high cholesterol, and asthma during the reproductive ages.9 Therefore, approaching women’s health from a life course perspective offers an opportunity to reduce the pregnancy-related complications and deaths and to eliminate disparities through enhanced health promotion and disease prevention.10
Diabetes has become a global pandemic because of the sedentary lifestyle, urbanization and has lead to increased commonness of obesity.11 In fact, a high prevalence of gestational diabetes mellitus (GDM) of the order of 18% has been reported in India.12 Similarly, hypertension/high blood pressure has been found to be the most common chronic disease during pregnancy. It reduces the supply of oxygen and nutrients to the uterus, potentially slowing the child’s growth and increasing the risk of low-birth weight.13
However, nutritional deficiency like anemia is not only leads to poor outcomes in pregnancy and reduced work productivity among adults, but also contributes to deaths among pregnant women. Levy et al14 in their retrospective study evaluated the pre-term birth and birth weights of the anemic pregnant women which has determined maternal anemia as an independent risk factor for poor birth outcome. However, severe anemia during pregnancy may also have adverse effects on the mother and the fetus.15
With an epidemiological transition started in India, the burden of chronic disease and non-communicable diseases is on the rise.16 It has been predicted that there will be a rise of 67% death among all deaths by chronic diseases in 2020, which was 53% in 2005.17 However, there is a dearth of literature on maternal chronic disease and adverse birth outcome among women from lower socio-economic strata in India. Hence, our study tries to examine the chronic disease prevalence among women and its association with adverse birth outcomes that belong to lower socio-economic strata of the population in Mumbai city.
Study Area
The population of Mumbai has significantly increased over the past few years leading to an alarming population amongst the slum dwellers too. According to census 2011,18 the population of Mumbai was 12 million and the number of people living in slum areas has also grown up by a staggering 3 million. Being a metropolitan city, the situation in Mumbai is different from other cities and a large percentage of population lives in the slum areas. Hence, the main aim of the study is to bring out the prevalence of chronic health complications among women and its adverse impact on birth outcome. Mainly among those from low-income households, living in slum areas, poor and not willing to utilize the health facilities provided by the private health sector. In this context, a tertiary hospital was selected which is situated nearby the slum areas of Mumbai.
MATERIALS AND METHODS
Self-reported reproductive health complications of inpatients were collected through personal interviews in a tertiary hospital of Mumbai. A total of 300 inpatients were selected based on their consent for participation in the interview from 20th January to 31st May 2013. The interview was conducted on women (inpatients) that came for delivery at the selected hospital and are from the lower socio-economic strata of the population. The main focus was to access the prevalence of chronic diseases among women in the surveyed hospital. The patients were enquired whether they suffered from any chronic diseases at any time of their life, especially before or during pregnancy. Specific type of chronic diseases such as, diabetes, hypertension, anaemia, any cardiovascular diseases etc. are included in the questionnaire. Women were also asked about the treatment they received for their chronic illnesses. The self-reported chronic disease status was also cross verified with the hospital case sheets to know the disease status. Among the selected population 151 were having any disease during pregnancy while 149 does not reported of any disease status during pregnancy. Reporting of any chronic disease during and before pregnancy was taken as the dependent variable for the analysis where, ‘having any chronic disease was taken as ‘1’ if ‘yes’ and ‘0’ if otherwise. For further analysis, all the reported diseases were grouped into three different categories, like women having at least one chronic disease, one to two chronic diseases and more than two chronic diseases during pregnancy.
The outcome variables of the study were low birth weight, prematurity, birth defects and other neonatal complications. However, to compare the pre-natal and perinatal outcomes, participants were categorized into groups according to the number of live births and previous pregnancies. So the participants were categorized into two groups; Primiparous and multiparous with chronic disease during pregnancy and primiparous and multiparous without chronic disease. Socio-economic and demographic characteristics of women were considered as independent variables for analysis to see the impact on health of the women and new-born. Both descriptive and analytic statistical methods were used. Frequencies and bi-variate analysis was performed to see the disease prevalence. Whereas, inference statistics was calculated using chi-square tests according to Pearson’s coefficient.
Chi-square test was performed to explore the significance difference between the selected women and new-born health indictors. As Chi-square test is used to see the association between two classifications (classifier variable) of a set of counts or frequencies and compares the observed and expected frequencies in each category. Results are presented in terms of odd ratios and associated p-values. All the analysis was done using SPSS 20.
Ethical Approval
The International Institute for Population Sciences-Students Research Ethics Committee (IIPS-SREC) approved the study, and it was explained to the participants that the information collected was solely for the purpose of research and the confidentiality of their names would be maintained. The participants’ verbal consent was obtained and recorded on paper. .
RESULTS
Demographic Profile of the Respondent
The mean age of the respondent is 25 years (SD±4.06). The highest numbers of respondent (inpatients) were in the age group of 20-24 years (45.7%) whereas only 3.3% of respondent is in age below 20 years. The mean age at marriage of the respondent is about 20 years (SD±2.71). More than half of the total respondents were married before completion of 20 years of age (56.6%). The mean duration of marriage is around 6 years (SD±4.03). Half of the respondents were married for less than 10 years. About 66% of women reported of having their first child at the age group of 20-24 years and the mean age at first birth was 21 years, whereas 32% of the births are of first ordered birth. Forty-nine percent are second ordered and 19% births are third or higher ordered birth. Out of the total births 52% were male and 48% were female child. Some preference was seen among the women as many of them reported that they gave birth of more than two or three children because they wanted a male child (Table 1).
| Table 1: Demographic Characteristics of Participants. |
|
| Background Characteristics |
N
|
%
|
| Age of women (mean 25.25±4.06) |
|
|
| Less than 20 years |
10
|
3.3
|
| 20-24 years |
137
|
45.7
|
| 25-29 years |
100
|
33.3
|
| More than 30 years |
53
|
17.7
|
| Husband’s age (mean 29.61±4.84) |
|
|
| Less than 25 years |
27
|
9.0
|
| 25-30 years |
175
|
58.3
|
| 30-35 years |
64
|
21.4
|
| More than 35 years |
34
|
11.3
|
| Age at marriage (mean 19.50±2.71) |
|
|
| Less than 20 years |
170
|
56.6
|
| 20-25 years |
119
|
39.7
|
| More than 25 years |
11
|
3.7
|
| Marriage Duration (Mean 5.73±4.03) |
|
|
| Less than 5 years |
132
|
44.0
|
| 5-10 years |
135
|
45.0
|
| More than 10 years |
33
|
11.0
|
| Age at first birth (mean 21.48±2.95) |
|
|
| Less than 20 years |
49
|
23.9
|
| 21-24 years |
135
|
65.9
|
| More than 25 years |
29
|
10.2
|
| Birth order |
|
|
| One |
96
|
32.0
|
| Two |
146
|
48.7
|
| Three and more |
58
|
19.3
|
| Sex of the child |
|
|
| Male |
156
|
52.0
|
| Female |
144
|
48.0
|
Prevalence of Chronic Disease among Women
About half of the women reported having a chronic disease during pregnancy. Amongst all the diseases, anaemia (40.7%), respiratory disease (39.0%), hypertension (11%) and diabetes (9%) (Table 2) were found to be the most severe.
| Table 2: Prevalence of Chronic Disease before and during Index Pregnancy. |
|
Type of Chronic diseases
|
Disease prevalence among women |
|
During pregnancy1
|
Anytime before pregnancy2
|
| N |
% |
N |
%
|
| No disease |
149
|
49.7 |
90 |
30.0
|
| Any chronic disease |
151
|
50.3 |
210 |
70.0
|
| Diabetes |
14
|
9.3 |
4 |
1.9
|
| Hypertension |
16
|
10.6 |
77 |
36.7
|
| Severe anemia |
61
|
40.7 |
120 |
57.1
|
| Tuberculosis |
21
|
13.9 |
109 |
51.9
|
| Cardiovascular disease |
3
|
2.0 |
0 |
0.0
|
| Respiratory disease |
59
|
39.0 |
33 |
15.7
|
| Malaria |
5
|
3.3 |
88 |
41.9
|
| Note: 1Reported chronic disease by women were cross-checked with case-sheets
2Self-reported disease prevalence |
Table 3 shows the socio-economic and demographic characteristics and its association with chronic disease prevalence among women. A negligible difference was found in reporting of having any chronic disease during pregnancy by age of the women. However, women in age group above 30 years reported more of having any chronic disease during pregnancy. Reporting of having any chronic disease, was found more among women with her second parity (52.1%). Meanwhile, more than three fifth of women reportedly underwent a C-section (Caesarean section) and about three-fourth had forceps delivery those were having any chronic disease during pregnancy.
| Table 3: Type of Chronic Disease Prevalence among Women during Pregnancy (most Recent Birth) by Socio-Demographic Characteristics. |
|
Characteristics
|
Any chronic disease during pregnancy
|
| Age of women |
|
| Less than 20 years |
50.0
|
| 20-24 years |
47.7
|
| 25-29 years |
52.2
|
| More than 30 years |
54.7
|
| Parity of women |
|
| One |
49.0
|
| Two |
52.1
|
| Three and more |
48.3
|
| Type of delivery |
|
| Normal |
49.8
|
| C-section |
61.5
|
| Forceps |
71.4
|
| Number of ANC visit |
|
| Only once |
43.8
|
| 2-3 times |
43.4
|
| More than 3 times |
53.1
|
| Women’s education |
|
| Primary |
57.1
|
| Secondary |
49.2
|
| Higher |
58.6
|
| Working status |
|
| Working |
30.0
|
| Not working |
51.0
|
| Religion |
|
| Hindu |
48.1
|
| Muslim |
52.9
|
| Treatment received |
|
| Yes |
98.0
|
| Total |
50.3 (151)
|
Women with any chronic disease during pregnancy reported to have had more antenatal check-ups compared to women without any disease. It is about half of the women who received proper antenatal check-ups during pregnancy as they needed more care and treatment with a disease. Similarly, highly educated women reported having more disease prevalence because they were aware of the symptoms of the diseases and its consequences compared to their counterparts. Ninety-eight percent of women received treatment for their chronic diseases during pregnancy and most of them were treated in public hospitals.
Association of Chronic Diseases and Birth Outcome
Result demonstrates that most of the newborns with low birth-weight were delivered by women with who suffered from a chronic disease during pregnancy (33.4%), than women without any disease (26.4%) (c2=0.71; p<0.10). Similarly, smaller size at birth (14.4%) and pre-mature delivery (10.6%) was also found to be high among women with any chronic disease during pregnancy (c2=0.84; p<0.05). However, the result clearly shows that women having any disease during pregnancy have higher chances of delivery in C-section (11.3%) and with the help of forceps (13.2%) compared to women not exposure to any disease during pregnancy, which is 3% and 5% respectively.
But, newborns with birth defects were found to be higher among women without disease during pregnancy. The study results did not show any differentials in reporting of stillbirth among women with any chronic disease during pregnancy or not (Table 4).
| Table 4: Outcome of Pregnancy by Chronic Disease Status of Women during Pregnancy |
|
Birth outcomes
|
Disease prevalence among women during pregnancy |
| With any Chronic disease |
Without any Chronic disease |
c2
|
| Weight at birth |
|
|
|
| Less than 2.5kg |
33.4
|
26.4
|
0.71*
|
| 2.5 kg to 3.5kg |
16.8
|
14.9
|
| More than equal to 3.5 kg |
49.8
|
58.7
|
| Size at birth |
|
|
|
| Smaller than average |
14.4
|
12.2
|
3.48
|
| Average |
84.1
|
87.8
|
| More than average |
1.5
|
0.0
|
| Type of delivery |
|
|
4.86*
|
| Normal |
75.5
|
91.2
|
| C-section |
11.3
|
3.4
|
| Forceps |
13.2
|
5.4
|
| Gestation month at delivery |
|
|
|
| Seventh month |
10.6
|
7.4
|
0.84**
|
| Eight month |
14.3
|
14.1
|
| Nine month |
75.1
|
78.5
|
| Any birth defects |
|
|
|
| Yes |
2.9
|
3.4
|
0.50
|
| No |
97.1
|
96.6
|
| Birth outcome |
|
|
|
| Live birth |
98.7
|
98.6
|
1.33*
|
| Stillbirth/Neonatal death |
1.3
|
1.4
|
| N |
151
|
149
|
|
| Note: p values ***<0.01, **<0.05, *<0.10 |
The gestational month of delivery was also seen less among women who had any chronic disease during her pregnancy (i.e., delivered before completion of nine months). About 11% of the women delivered within seven months of gestational period and with chronic disease during pregnancy (c2=0.84; p<0.05). However, no significant differential was observed in reporting of experiencing stillbirth and neonatal mortality. The study shows that women with any chronic disease during pregnancy had a poor health status of the newborn.
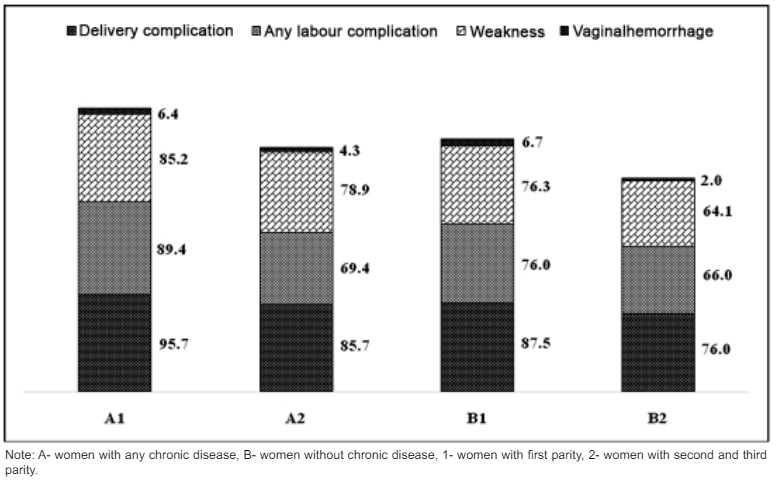
Figure 1 represents some of the specific complications during the time of delivery and after delivery among women who had developed any chronic disease during pregnancy. It also provides information by parity of women such as women having chronic disease or not with first parity and having chronic disease or not with her second and more parity in the studied area. It clearly shows that women having any chronic disease irrespective of first or second and more parity are more prone to having any complication at delivery as compared to women without chronic disease during pregnancy and about 96% with first parity and 88% with second or more parity respectively.
Figure 1: Complications during Delivery and after Delivery Plot Against having Chronic Diseases or not during Pregnancy by Parity of Women.
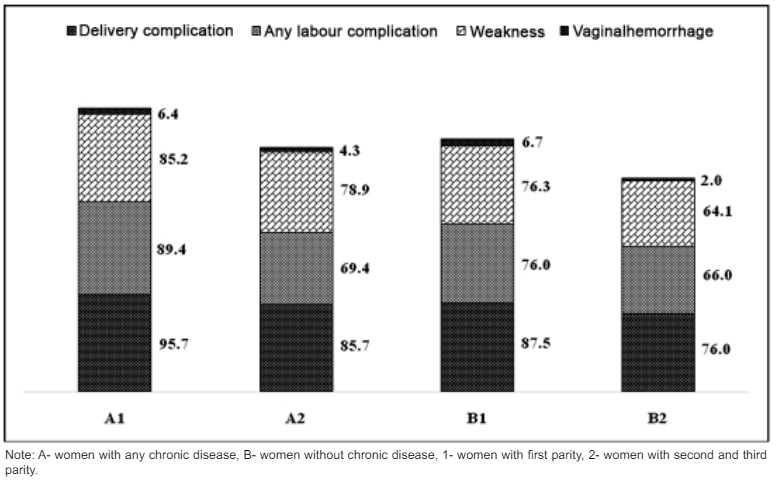
Women with their first parity were observed to have experienced more complications like labor complication and weakness during and after delivery compared to their counterparts. However, chronic disease prevalence was another most important cause of health complications among women as reported by them. It was also observed that, any health complication during pregnancy was highly reported by women those who were not suffering from any chronic disease during pregnancy. Whereas in both the groups, vaginal hemorrhage was found to be higher among women having chronic diseases.
Table 5 represents the groups of chronic disease prevalence before and during pregnancy and its relation to the newborn health complications. Difficulty in breast feeding among newborn was highly reported by women with any chronic disease at any time before and during pregnancy. While it was seen more among those having any chronic disease any time before pregnancy (58.4%) than others. Breathing problem was found to be high (16.9%) among newborns whose mothers developed chronic diseases during pregnancy, while about 4 point less (13%) among those had chronic diseases at any time before pregnancy. Low weight at birth and baby develop yellow staining on palm and soles were also found high among women with disease prevalence during pregnancy compared to their counterpart.
| Table 5: Newborn Health Complication by Chronic Disease Prevalence of Women (before and during Pregnancy). |
|
Newborn health complications
|
Prevalence of any chronic disease among women |
| During pregnancy1 |
Any time before pregnancy2
|
| Low weight |
22.0
|
20.8
|
| Feeding problem/Poor sucking |
56.8
|
58.4
|
| Problem in breathing |
16.9
|
13.0
|
| Dull and inactive |
5.1
|
5.8
|
| Yellow staining on palm and soles on body |
13.6
|
11.1
|
| Cold/cough |
16.9
|
16.3
|
| Ulcers in mouth |
12.7
|
7.8
|
| Any other problem |
55.1
|
58.8
|
| Note: 1Reported chronic disease by women were cross checked with case-sheets
2Self-reported disease prevalence |
DISCUSSION
The main aim of the study is to bring out a brief overview of chronic disease prevalence during pregnancy and its association with the health of women and the health of the new-born. Half of the women were suffering from a type of chronic disease during pregnancy whereas about three-fourth of them reported having any chronic disease at any time in lifetime. Severe anaemia (40.7%) and chronic respiratory illness (39.0%) were the most common diseases found among women. Study by Kersten et al1 has found that every fifth pregnant woman suffers from at least one chronic disease, and higher prevalence rates have reported in the literature. In an American study analyzing 6294 women of childbearing age, 26.6% of the participants had one of the most prevalent chronic diseases. In contrast, 39.1% of all women who were not pregnant reported that they were chronically ill.19 While our study shows that about half of the women reported of developing any chronic disease during her pregnancy.
Severe anemia is not only concentrated among women at pregnancy but also before pregnancy that continues to be a major public health problem. It has been estimated that more than one-third of the world’s women are anemic; the vast majority of this being in developing countries.20,21 It is generally agreed that the prevalence of malaria is higher among pregnant women than other groups, and that can lead to abortion, intrauterine fetal death, pre-mature delivery and even maternal death.22 Whereas, the prevalence of malaria was found to be most common among women, although, not particularly during pregnancy. Study shows that women having more than one or more than two chronic disease at the time of pregnancy has a higher chance of experiencing complications like labour related complications, convulsion (not from fever) during delivery. Where the educational status of women and receiving any antennal check-ups has no positive association with developing any chronic disease during pregnancy as disease prevalence is quite hazardous to the weak immune health.
The study also highlights the women’s chronic ill status and its association with the health of the new-born. A positive correlation was found between the mother’s ill health status and adverse health outcome of new-born.While women with severe anaemia and severe respiratory illness also reported of delivering new-born with poor health status. Similarly, low weight at birth (54.1%), small sized baby (55.0%) and premature baby (66.7%) were delivered by the women who developed any chronic disease during her pregnancy compared to women without disease. So, it can be summarized that there is a positive association between mother’s chronic ill health during pregnancy and adverse health outcome of the new-born. Chronic disease among pregnant women such as severe anemia has a significant influence on adverse pregnancy outcome.1 Similarly, in our study we have found that a newborn with low birth weight, small size at birth and premature birth were delivered by women who developed any chronic disease during pregnancy.
CONCLUSION
This analysis was done on hospital-based study in which the prevalence of all major chronic diseases during and before pregnancy was included as reported by the inpatients. Half of the women suffered from at least one chronic disease during pregnancy. In addition to this, the perinatal outcome appears to be less favourable for newborns of women with chronic diseases.
LIMITATION
The previous chronic history was taken based on the women’s self-reported response. There were no clinical records to verify the privious history.
ACKNOWLEDGEMENT
The authors would like to thank Head of the Department (gynecology) of the surveyed hospital for allowing data collection and would also like to thank the staff and respondents for their cooperation and help during data collection.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interest.