INTRODUCTION
Granulosa cell tumors belonged to the sex cord-stromal tumors of the gonads and granulosa cell tumors commonly arose from ovaries. GrCT are rare and can be classified into adult and juvenile types. Juvenile type of GrCT mostly concerned infants and followed a benign course.1 However, adult type GrCT may be potentially malignant and more aggressive progression. Less than 50 cases of adult granulosa cell tumor (aGrCT) have been reported.2,3 In this paper, we presented a case of an elderly male diagnosed of aGrCT.
CASE REPORT
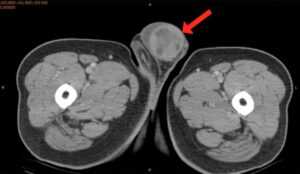
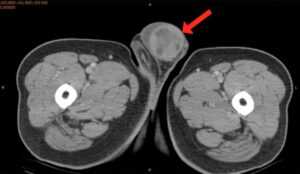
An 82-year-old male visited our hospital due to enlarging left testis for 3 months. He denied scrotal pain/tenderness/heaviness, abnormal urethral discharge or fever episode within the past 3 months. Physical examination showed prominent enlargement, firm and hardness of left testis. No inguinal lymphadenopathy was palpable. Sonography revealed diffuse heterogeneous density of left testis. LDH, AFP and B-HCG were all within the normal range. Abdominal to pelvic computer tomography scan (CT) showed space-occupying lesion in left testis with surrounding fluid accumulation (Figure 1) but no evidence of lymph node enlargement or distal metastasis. He denied any family history of testis cancer. There was also no gynecomastia symptoms or signs. Under the impression of testicular cancer, he received radical orchiectomy on September 13, 2013. The final stage of testis cancer is pT1N0M0. The operation went smooth and he was discharged the following day. His recovery was uneventful and no recurrence signs/symptoms were noted in subsequent follow-up.
Figure 1: Pelvic CT. Space-occupying lesion in the left testis with surrounding fluid accumulation (red arrow).
PATHOLOGIC FINDINGS
Macroscopically, the testicle measured 7.0×4.7×4.0 cm. The spermatic cord measured 12 cm in length and 1.4 cm in diameter. Tumor was largely replaced by tumor lesion. The tumor is encapsulated and yellowish and homogenous in appearance, measuring in 4.5×3.5×0.9 in size (Figure 2). Some microcysts but not hemorrhagic or necrotic changes are seen on cut surface. The spermatic cord is unremarkable. The surgical margin is free from the tumor.
Figure 2: Gross cut surface. The tumor occupied the seminiferous tubules and focally extended into the rete testis tubules.

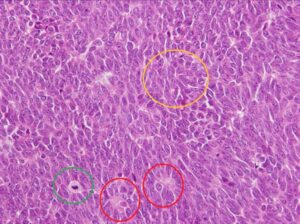
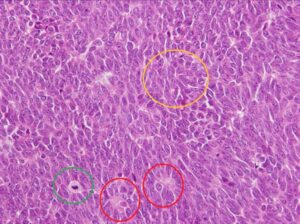
Microscopically, the tumor lesion located in the right seminiferous tubules and separated by fibrous tissue of tunica albuginea (Figure 3). It shows a solid tumor composed of compacted cells with uniform nuclei common with irregular nuclear membrane, nuclear groove, ample amphophilic cytoplasm and indistinctive border (Figure 4). Some tumor cells grew in sheetlike, cell cord, trabecular and follicular patterns. Some amorphous substance seems like the Call-Exner bodies (Figure 4) and variable thickness of the fibrous septae are also seen. No tumor necrosis or hemorrhagic change is found. The mitotic figure is variable in areas sometimes up to 7/10 HPF. The tumor is mainly located at the seminiferous tubules and focally extended into the rete testis tubules. The epididymis and the vas deferens are not tumor involved but compression and atrophic change is noted. The spermatic cord is unremarkable. The surgical margin of spermatic cord and the tunica albuginea are also unremarkable.
Figure 3: Tumor lesion X4. The tumor lesion located in the right seminiferous tubules and separated by fibrous tissue of tunica albuginea.

Figure 4: Tumor lesion X40. The uniform spindle to ovoid tumor cells with mildly pleomorphic nuclei sometimes with nuclear grooves (yellow circle), one or two nucleoli, present mitotic figures (green circle) and Call-Exner bodies (red circle) between the tumor cells.
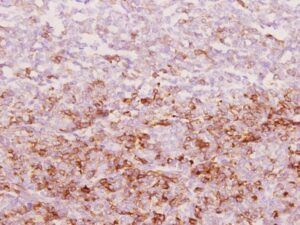
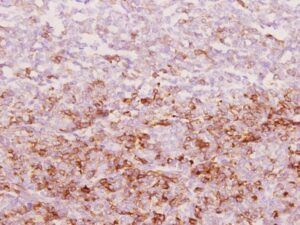
The immunohistochemical stain of the neoplastic cells show positive for valentine (Figure 5), inhibin-alpha (Figure 6), and Bcl-2, focal positive for CD56 and negative for CK, calretinin, CLA, S-100, CD99, chromogranin, synaptophysin and Smooth Muscle Actin. A lesion of adult type granulosa cell tumor is considered. The tumor size is less than 7 cm, no hemorrhage and necrosis, but the mitotic figure is up to 7 /hpf (than 4 / hpf), so increase in risk potential for malignancy is noted.
Figure 5: X40 immunohistochemical stain of the tumor showed positive for Vimentin.

Figure 6: X20 immunohistochemical stain of the tumor showed positive for inhibin-α.
DISCUSSION
aGrCT is the minority group of reported GrCT cases as described by Miliaras et al1. aGrCT patients usually present with slow growth, painless scrotal swelling or mass. The average time of enlargement was 5.4 years. In particular, about 20% of male cases would present gynecomastia.4 The prevalence age ranges from 16 to 77 years and is often above 50 years old. It is hard to make a diagnosis simply from the outer appearance and laboratory workup. The diagnosis would depend on histology and immunohistochemistry. According to Miliaras et al1 aGrCT may have a more aggressive course and it can cause distal metastasis even after many years. However, there are no well-established concept about poor prognosis of aGrCT because of its rarity. Hanson and Ambaye have suggested that tumor size larger than 5 cm is a feature associated with malignancy in the testes.5 Jimenez-Quintero et al considered size >7 cm, vascular or lymphatic invasion, and hemorrhage or necrosis somewhat predictive of spread.6
Thus, follow-up for patients receiving radical orchiectomy should be extended. As far as we know, the most common distal metastasis site of testicular germ cell tumor is the retroperitoneal lymph node. Retroperitoneal lymph node dissection (RPLND) is also a treatment option for patients with lymph node metastasis in testicular germ cell tumor. Although the therapeutic role of RPLND is unclear, it is still an option after radical orchiectomy in aGrCT patients with malignant features, as described by Ashraf et al5 Except surgical management, Jimenez-Quintero et al6 suggested that etoposide based chemotherapy with adjuvant radiotherapy may be a curative option for metastatic disease. To date, in the absence of guidelines regarding aGrCT, it is difficult for urologists to implement a follow-up program.
In conclusion, this patient is relative old age (in the past literature, the oldest person is 83 year-old) and short duration of clinical signs. Because of older person may lose the ability of self-care and daily activity, many patients was found of metastatic disease while diagnosed. Fortunately, in our case, he received surgical treatment within 3 months and no metastasis lesions was found via abdominal CT. There were also no suggestive poor prognostic factors like larger tumor size, tumor necrosis or hemorrhage. After 2 years follow-up, there was no signs of recurrence. Long-term follow-up is recommended, since recurrence of the disease may appear late in the clinical course.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
CONSENT
Authors obtain written informed consent from the patient for submission of this manuscript for publication.