INTRODUCTION
Tumoral calcinosis is a rare benign condition characterized by deposition of calcium salt in different peri-articular soft tissue regions, mainly in the juxta-articular areas.1 It affects mostly African people, especially in the second decade, but it can affect any age.2,3,4 The term tumoral calcinosis was first used by Inclan et al in 1943,5 however, the condition itself was described before in 1899 by Duret.6
CASE REPORT
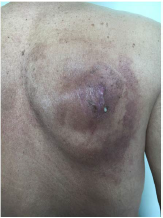
A 58-year-old patient, on chronic hemodialysis, presented with a six-month history of three slightly painful swellings gradually increasing in size located in the shoulder and both the hips. Clinical examination found a mass on the right shoulder (Figure 1) from which there was a flow of thick yellowish-white liquid. It also revealed the presence of three large lumps. The largest one on the right hip (measuring 20 cm in length) extended to the lower third of the thigh and was of firm consistency (Figure 2).
Figure 1. Mass of the Right Shoulder Showing Discharge of Thick Yellowish-White Liquid
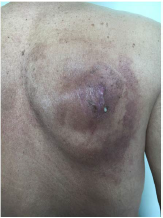
Figure 2. Voluminous Mass, Measuring 20 cm on the Right Tigh and Extending above the Knee, of Firm Consistency

X-ray of the shoulder showed a periarticular calcified mass of multi-locular appearance capping the humoral head without lysing the bone. Magnetic resonance imaging (MRI) revealed the presence of several soft tissue masses on both shoulders and both hips, giving a bees nest-like appearance (Figure 3). Their matrix was osteoid and they were seen to infiltrate adjacent muscle whilst sparing bones and joints. The radiological findings were very suggestive of pseudotumoral calcinosis.
Figure 3. MRI Showing Soft Tissue Masses on both Shoulders, Giving a Beesnestlike Appearance

Laboratory tests showed a high serum calcium concentration, a normal phosphate concentration and elevated serum parathyroid hormone concentration. After the diagnosis of hypercalcemia with tumoral calcification secondary to chronic renal failure was made, the patient was placed on a low calcium diet and intensive hemodialysis sessions. However, the calcifications did not improve and the patient refused surgery.
DISCUSSION
There are three clinical forms of pseudotumoral calcinosis.
- Tumoral calcinosis secondary to chronic renal failure due to a disorder in calcium and/or phosphate metabolism.
- A familial form with a an autosomal recessive transmission, which may be hyper phosphataemic or normo-phosphataemic.
- A form with a sporadic pattern which generally has normal calcium and phosphate levels.7,8
Although, lesions usually appear around large joints, cases involving cervical and lumbar spine, the supraclavicular area and toes have also been reported.9 Large lesions can cause pain, functional impairment and nerve compression.10 Local complications include skin ulceration with a chalky milk-like discharge and chronic infection with resulting secondary amyloidosis. Typically, there is no bone involvement, although periosteal reaction or erosion due to pressure may be found. Tumoral calcinosis has a typical appearance on radiographs: amorphous, cystic, and multilobulated calcification located in periarticular soft tissues. On MRI, tumoral calcinosis is seen as a well-circumscribed multicystic mass.11 The differential diagnosis of tumoral calcinosis includes multiple causes of metabolic and dystrophic calcification including:
- Connective tissue diseases (systemic sclerosis, mixed connective tissue disease, dermatomyositis, systemic lupus erythematosus)
- Neoplastic diseases (synovial sarcoma, osteosarcoma, chondrosarcoma)
- Degenerative diseases (calcific tendonitis, calcific bursitis).12
Surgery is the gold standard treatment. Indications for surgery are pain, recurrent infection, ulceration and functional impairment..13
CONCLUSION
The diagnosis of tumoral calcinosis is based on clinical context, biology and radiology. Management of tumoral calcinosis is difficult. Surgical excision is the best treatment option, but the deposits can recur after surgery. Other options include increasing dialysis dosage phosphate deprivation and vitamin-D analogs but the response may be limited. Renal transplantational ways leads to resolution. However, more studies are necessary in order to clarify the most effective treatment modality for each type of tumoral calcinosis.14
CONSENT
The authors have received written informed consent from the patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.