INTRODUCTION
Mobile health (mH) communications smartphones and other devices (SP/D) used for data transport, computing and integration are a force in business, entertainment and health communities. mH and social media are growing exponentially via the X, Millennial/Y and Z generations.1 They are delivering healthcare anytime/anywhere and surpassing geographical, cost, temporal and organizational barriers.2 This movement is consistent with not only patient-centered care, but participatory medicine, in which patients are responsible drivers of their health with physicians3 according to the Institute of Medicine.4,5
mH, telemedicine and other services are considered part of a telehealth or e-health (eH) spectrum of care, including e-behavioral health (eBH).6,7 Traditional telehealthcare services have been provided synchronously by video conferencing7 or asynchronously.8 mH and its corresponding mobility components are central to healthcare monitoring and alerting systems, clinical and administrative data collection, record maintenance, delivery programs, medical information awareness, detection and prevention systems, drug-counterfeiting and theft.9 mH hasbeendefined as “unwired e-med”, mobile communication and network technologies and now mobile or wireless communication technologies for health and healthcare.10,11,12 A worldwide review of the literature on eH through 2010 found four primary areas of service delivery: information provision; screening, assessment, and monitoring; intervention; and social support (Table 1).13
| Table 1. The E-BH Spectrum of Technology Use in Healthcare for Patients and Clinicians |
| Level |
Source/ Entry |
Initiator Goals/Aims |
Questions And Perspectives |
Liabilities |
Suggestions For Programs |
| 1 |
Website information |
Health information: gain perspective, obtain standard and updated info |
Do I need more information? How should I approach the problem? What is out there?
Better if referred by clinician who has checked it out
|
Quality of information and lack of regulation |
Provide training on how to evaluate sites and to identify good ones; how to screen for patients’ use |
| 2 |
On-line formal educational materials |
Person/patient: education
Caregiver: education, supports, and advice
Clinician: continuing medical education (CME)
|
I learn easier this way?
I need “sound” info to make decisions for loved ones
CME implies good quality; peers’ opinion helpful
|
Some prefer in-person interaction (e.g., Q&A)
May not fit learning style
|
Provide advice on good options, how to evaluate the materials and help patients do likewise. |
| 3 |
Support/chat groups or “communities |
Spontaneous, anonymity, gain answers/tips and greater perspective
Socialization and networking |
What should/can I do?
What are others doing locally, regionally or globally?
Can I connect easier with others? |
Peer compatibility?
Information quality?
Who is talking on the other end? |
Provide curricula in general and how to use at specific clinical sites (e.g., inpatient unit, outpatient care) |
| 4 |
Self-directed assessment and decision-making options |
Person/patient: tips to reflect, make changes and get help
Caregiver: tips to reflect, tools to assess loved ones, and next steps
Clinician: give patients assignments/resources; obtain tips on clinical care |
What are my needs and resources? What is my next step in seeking help?
Can my love ones/patients get help/support outside the office with help (i.e., with a nurse, mid-level or care coordinator)? |
Not all problems can be self-assessed
Some illnesses affect insight and reflection
Quality is an issue; get a reference |
Provide training on how to help patients consider options, take steps and share information with clinician; start self- and life-long learning options |
| 5 |
Social media (SM)/ networking |
Person/patient/caregiver: easy, convenient, and spontaneous
Clinician: rarely use; could screen if/what patients are doing, why and impact
All: if purposeful and focused on one dimension, it could add to relationship |
Can impact therapeutic alliance positively/negatively
Public information may be visible; it cannot be collected for analysis, though
Discuss, weigh pros/cons, address privacy, when to use/not use (e.g., SI) and tracking (if any)
Not billable care |
Not HIPAA compliant?
Undisclosed and/or impulsive use may indicate problems and boundary issues?
Personal/ professional role diffusion? |
Provide skills, knowledge and approaches in curriculum and with case conferences
Focus on developing professional role in transition from past personal experience(s) |
| 6 |
Assisted self-care assessment and decision-making; de-identified |
Person/patient/caregiver: feel ownership of care and better partnership is with clinician
Clinician: distributes my time with help from others and empowers patients |
Empowering, in general?
Increased self-efficacy/ confidence?
Feel part of a team?
Do I have time to discuss issues with patient?
Is there time to train team and share decision-making? |
Occasional “bad” decision or poor outcome, partly due to lack of context?
Doing more without time/quality is a risk? |
Provide training on how to screen what patients are doing and when to seek help, and when to make decisions together. |
| 7 |
Asynchronous video or one-time synchronous consultation |
Person/patient/caregiver: obtain good quality tips for primary provider to use
Clinician: distributes time well with help from others and empowers patients |
Feels good about getting “better” care; glad primary provider gets an opinion
Primary provider learns and develops relationship with psychiatrist? |
Can primary provider use tips? They will work for which patients?
Learning curve takes some time? |
Build into the regular care continuum, like an option on a stepped continuum |
| 8 |
Asynchronous, between-session patient-clinician contact (e.g., mobile app or e-mail/text) |
Person/patient/caregiver has minor question, forgot a question, or needs a detail
Clinician: good for quick advice and simple details
All: send/assign apps, questionnaires, reports (e.g., individualized educational plans); use screening/ follow-up surveys to track |
Convenient to reach the clinician or team member?
Easier for teen patients, who prefer texting over calling?
Build into the EHR?
Is the contact tracked, private, documented and billable? |
Some patients and/or clinicians do not use?
Things taken out of context; errors?
HIPAA compliant?
Some see as a nuisance (i.e., extra time) |
Provide training across the curriculum; boost at core training sites; enhance with subspecialty (e.g., child)
Faculty development suggested for patient and trainee e-mail/text |
| 9 |
Continuous mobile health/ e-monitoring to database/ EHR |
Person/patient/caregiver likes access
Clinician: longitudinal monitoring, frequent contacts
All: set expectations and boundaries |
Patient feels glad to be tracked, part of treatment and ‘connected’ to clinician
Integrated decision-making takes preparation and extra time? |
Best in systematic care models with team-based approach? |
Team training, coordination, communication and documentation is important |
| 10 |
Synchronous or in-person ongoing care |
Person/patient: it works and is much more convenient
Clinician: if patients like it, it is a good option |
Allows synchronous decision-making (patient-clinician); links providers (e.g., primary care psychiatry) |
It always has to be scheduled (and paid for); not spontaneous |
Provide curriculum, and other experiences |
Two areas that are growing exponentially are SP/D and mobile apps, social health networking – partly to help users change behaviors (e.g., nutrition/diet, stress reduction).14,15 Mobile apps offer: 1) portability for access anytime, anywhere, regardless of patient geography and transportation barriers; 2) an inexpensive option versus traditional desktop computers; and 3) additional features (e.g., context-aware interventions and sensors)1,16 with real-time feedback. Overall, a review of behavior change revealed 19 studies had a 65% or greater retention rate and 6 studies reported changes in planning and self-monitoring.17,18
A review of cognition and mH focused on three facets of cognition that are clearly implicated in public discourse regarding the impacts of mobile technology – attention, memory, and delay of gratification (reward processing).19 Regular engagement with these devices can lead to diminished attentional capacity – producing shorter attention spans and “scatter-brained” tendencies among those who are most invested with the devices – and worrying some that children and adolescents’ attention spans are shorter.20,21
This paper will help the reader by…
1) Defining and describing mH’sapproach, core concepts, components (e.g., SP/D), operations and processes within an e-health spectrum of service delivery,
2) Providing an overview of some cognitive functions relevant to new technologies and SPs/Ds, and
3) Describing a range of app options (and a few in detail) and outlining competencies for mH, SPs/Ds and apps.
METHODS
The review of the literature was conducted as per previously described methods1,6 using title word searches within the MEDLINE, PubMed, PsychInfo, Embase, Science Citation Index, Social Sciences Citation Index, Telemedicine Information Exchange databases, Centre for Reviews and Dissemination and The Cochrane Library Controlled Trial Registry databases for the period of May 2003 to May 2018. Primary words: apps, behavior, cognition, cognitive, devices, function, mobile, patient, practice, quality, satisfaction, service, smartphones, and technology. Secondary words: care, centered, education, mental, e-behavioral, e-mental, health, telehealth, telemedicine, telemental, and telebehavioral.
The evidence-based literature review followed the Agency for Healthcare Quality and Research (AHQR) and Cochrane Database of Systematic Reviews, which use a panel of multidisciplinary experts to rate two factors: 1) the quality of evidence (e.g., Levels I (best) to IV (least)); and 2) consensus, expert opinion. Level I (i.e., a high quality randomized trial or prospective study; testing of previously developed diagnostic criteria on consecutive patients; sensible costs and alternatives; values obtained from many studies with multi-way sensitivity analyses; and systematic reviews and Level II (i.e., lesser quality RCT; prospective comparative study; retrospective study; untreated controls from an RCT; lesser quality prospective study) was focused on randomized controlled (RCTs) with interventions using mH, SP/Ds and apps. These key words were cross-searched with the cognitive primary terms.
MOBILE HEALTH’S APPROACH, CORE CONCEPTS AND COMPONENTS
Internet and Mobile Health Trends for Self-Directed Habit, Lifestyle or Illness Changes
Internet and mH tools typically target good habits/health promotion, disease prevention and informal management of symptoms or problems.1 Techniques might include use of a diary, questionnaire or survey to provoke reflection or “stepping back” to re-evaluate one’s assumptions in a conclusion. Exercise and substance (i.e., alcohol) logs are popular, mood assessments (Moody Me https://itunes.apple.com/us/app/moody-me-mood-diary-tracker/id411567371?mt=8), and those that map behavior patterns across time, including triggers, diet, sleep and other related factors.
Among the fastest growing areas are related to nutrition/diet (i.e., apps to count calories and keep a food diary like iFood and Calorie Counter) and sports statistics (such as distance, speed and calories consumed).14 Despite the popularity of physical activity apps available on the commercial market, there were substantial shortcomings in the areas of data safety and likelihood of effectiveness.22 A review of medication adherence apps in the Apple App Store and the Google Play Store (N=5,881) found of those accessible without payment (N=420), only 3 with an evidence base and there were 3 broad categories of adherence strategies (i.e., reminder, behavioral, and educational).23 A total of 250 apps utilized a single method, 149 apps used two methods, and only 22 apps utilized all 3 methods. In particular, young people may benefit from structured health information, web-based screening and assessment, and online treatment options to reduce medication non-adherence.24 Mental health promotion in children and adolescents is increasing, too (e.g., Kindertelefoon (www.kindertelefoon.nl).6
mH Approaches and Themes
mH is able to incorporate qualities often associated with conventional health communication methods, such as personalization, tailoring, interactivity, and message repetition at a relatively low cost.25 An estimated 69% of the U.S. adult population track at least 1 health indicator, such as activity, weight, or symptoms26 at home or within primary care.27 Text messaging (short message service, SMS; containing 160 characters) varies in frequency (daily, weekly), interactivity (one-way vs. two-way), personalization and tailoring (all of the above).28,29 Text messages from web-based platforms allow for pre-scheduling of sending, automation, and better monitoring.
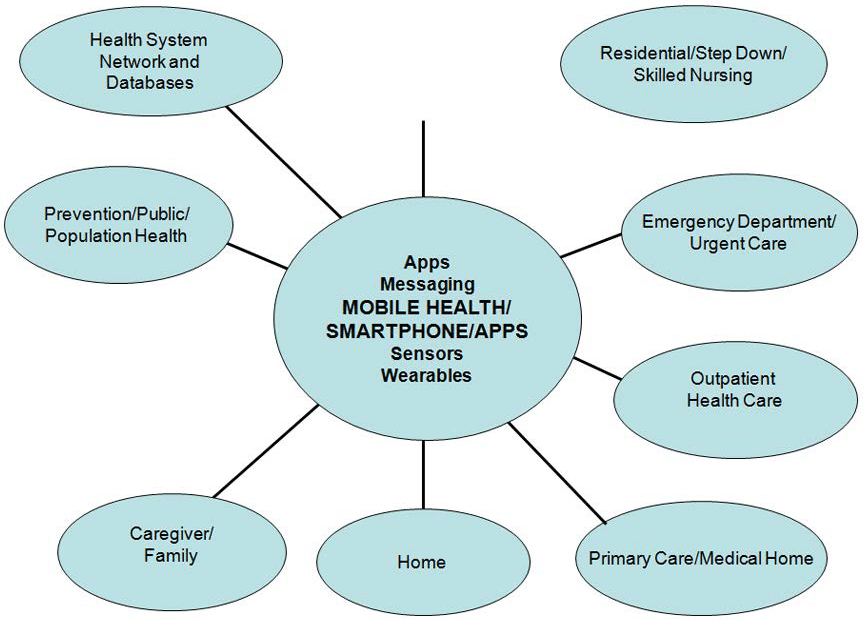
The SP/D is the core device linking people, communities and systems (Figure 1). They have the core functions of a modern computer paired with apps to facilitate day-to-day functions for health and disease management. Integrative components of a generic mobile health system potentially link: 1) a national health network; 2) hospital and other acute care centers; 3) home-based care; and 4) mobile health devices.30 The main functions SP/Ds and apps are: voice/video calling to remotely communicate; SMS; multimedia message services (MMS) with video clips/sound files to deliver education; inbuilt sensors (e.g., touch, motion and GPS) for clinical assessment, lifestyle and social activities; and device connectivity for practical and less error-prone data entry.1 The content of messages is of particular importance. Some characteristics such as personalization, caring sentiments, and polite text are associated with more successful preventative messages.31
Figure 1. Integration of Information in the Technology Age through The Mobile/Smart Phone and Other Technologies.
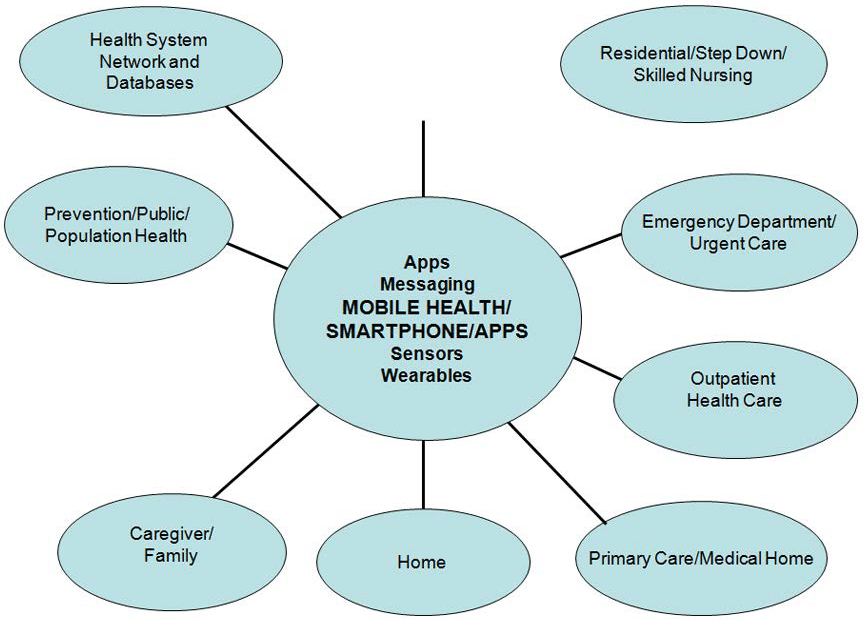
SP/Ds serve as organizing hubs that link patients’ health data to other health services; the bi-directional flow enables routine care or education from clinicians to patients in their own environment. Wireless monitoring devices gather data from sensors, input that data into a mobile medical app on the SP/D, and then relay the information to a centralized national health network. Theoretically, the data would be organized and processed through clinical decision support medical apps in a healthcare information system for review and response by clinicians (e.g., feedback, reminders of healthy behaviors, scheduled appointments, medications) 24-hours a day and 7-days per week.
Ecological momentary assessment (EMA) is a method for capturing more accurate accounts of a person’s or patient’s emotions, functioning and activity32,33,34,35 by sampling of naturalistic behaviors and experiences. Examples of EMA commonly used are daily diary methods, signal-dependent reporting, and event-dependent reporting; these reduce recall bias. Signal-dependent reporting involves the client reporting on symptoms at random intervals during the day in response to an alarm. Event-dependent reporting has the client report on symptoms after predetermined interpersonal or challenging events during the day. Of the three, signal-and event-dependent reports are more accurate and yet, they demand a level of engagement and motivation that may exceed the capacity of some participants.36 EMA data analysis use mood/affect changes to predict risk of suicidal ideation37 and provide a portal into teenagers’ psychological symptoms.38
COGNITIVE FUNCTION RELEVANT TO NEW TECHNOLOGIES AND THE SP/D
Overview
Our ability to contemplate the future through cortical function39 and we have higher levels of happiness and lower levels of stress than at other times. How we learn is dependent on our personal experience and professional training, and reflection with evaluation of our strengths and weaknesses is a key part of development. Learners progress to critical thinking via a series of developmental steps, from gathering information in rote, analyzing, and reconstructing data in a laborious manner; later algorithms are used to guide decision-making and mental shortcuts (or heuristics). Skills needed to solve a problem is developed by education, mentoring and practice.40,41
The problems in researching the use of SP/Ds include trouble employing true experimental methods with random assignment, literature based on topical and cross-sectional investigation of momentary rather than long-term impact for SP/D users, disparities in technology users’ backgrounds, biased (self) reporting of behaviors and a limited “half life” of research questionnaires.19 The SP/D era is also very short, so there is little broadly generalizable longitudinal evidence.
The Range From Healthy to Unhealthy Behaviors
Social media and networking options like Twitter® and Facebook® are common among the Digital Native (Z), Millennial (Y) and X Generations. Today’s youth engage with media through television, computer/video games, text/e-mail, mobile apps and video sharing platforms. On a typical day, American teenagers (13 to18 year-olds) average about nine hours of entertainment media use, excluding time spent at school or for homework; tweens (8 to 12 year-olds) use an average of about six hours of entertainment media daily.
While many aspects of this new media landscape can be positive, others are problematic. Positive aspects of technology for youth include speaking more freely, learning/knowledge gains, communication/engagement with others and creative exploration. Youth also use technology for depression, obesity and/or suicidal thinking,42,43 but the evidence base is limited.44 Concerns about media use – especially excess use of television and computer games – have arisen due to potential changes in mood, sedentary lifestyles, withdrawal from other activities and impaired sleep patterns.45 Problematic social media behaviors may range from disinhibition and the posting of ill-advised photos, to more extreme examples like online bullying, sexting, frank exploitation and other addictive behaviors.46,47,48,49,50 There are also negative effects on physical and mental health, neurological development and personal relationships, not to mention safety on roads and sidewalks.51,52 Finally, borrowing from business, the “opportunity costs” need to be assessed, as time spent on one thing limits the opportunity to spend it on another (better?) thing.53
Attention
There are different times of inattention and/or interruptions. Some occur when the user’s own thoughts drift toward a SP/D-related activity for immediate gratification. Users often then engage in a chain of subsequent task-unrelated acts on the SP/D. Importantly, SP/Ds are capable of interfering with focused attention even when the user attempts to ignore them (e.g., e-mail alert). Such notifications (i.e., the sound or feeling the vibration) significantly decrease performance on a concurrent attention-based task, even when the participant did not take the time to view the notification.54
Further evidence suggests that even the mere awareness of the physical presence of a SP/D may impact cognitive performance. Thornton et al55 conducted a study in which participants were asked to complete two neuropsychological tasks designed to measure executive function and attention – a digit cancelation task and a trail-making task. At the start of the experiment, the experimenter “accidentally” left a SP/D on the participant’s desk. Participants in the SP/D condition performed significantly worse on the more difficult parts of the digit cancelation and trail-making task. The researchers replicated these findings in a follow-up study for which half of the participants were asked to place their own SP/D on their desks. Texting during driving most likely parallels distractions in past simulation studies.56
Addictive Process
We are governed by the subcortex in many ways including addictions. The connection between an individual’s degree of “addiction” to a SP/D and the ability to achieve “flow” has been studied.57 A flow state relates to sustained attention in that it is “a state of concentration so focused that it amounts to absolute absorption in an activity”.58 Long-term, those who scored highest on the SP/D addiction scale scored significantly lower on the self-regulated learning and flow scales; they also do poorly with self-regulated learning.
Multi-Tasking
Media multitasking involves the simultaneous use of more than one media technology – and studies are assessing basic cognitive skills and the tendency to engage in simultaneous media-related habits. Computer-based behavioral tasks have been used to measure participants’ attentional functioning.59 The data revealed that those who reported engaging in more media multitasking were also less able to filter environmental distractions. Media multi-taskers exhibited higher switch-costs in a task-switching paradigm, indicating that they were less able to suppress the activation of task set representations that were no longer relevant to performance.60
Memory and Knowledge
There is less research investigating the relationships between SP/D habits related to memory and knowledge. SP/Ds provide constant access to an endless and ever-improving database of collective knowledge.61 The “Google Effect”, and later referred to by other researchers as “digital amnesia” demonstrates that the expectation of having later access to information can make us less inclined to encode and store that information in long-term memory. Humans are “cognitive misers”41 who rely on simple heuristics and mental shortcuts. Studies of heavy users of SP/Ds show less analytical “cognitive styles” and poorer performance on knowledge measures.62
Another potential impact of digital media on memories showed that taking photographs diminishes memory for observed objects.63 Recent trends in social media and networking use have prioritized ephemeral photo-sharing (e.g., Snapchat, Instagram).64 These allow users to send/post pictures, videos or messages that can only be viewed a limited number of times or for a finite period. Little is yet known about the specific effects of this, but it may act on memory in a way that is akin to the soon-to-be-erased files.
Delay of Gratification and Reward:
In addition to their effects on memory and attention, SP/Ds and related media are often implicated as the cause of a perceived cultural shift toward a necessity for immediate gratification.65 Studies are tentative/in process related to media multi-tasking and uses and gratifications theory.66 Subjects rate specific “motivation” (i.e., emotional, cognitive, social, or habitual) that drive them to engage in each media interactions, but often those needs are not met, which infers other factors may have been more influential.67
Other Cognitive Functions
Studies are exploring the relationship between technology habits and general academic performance. Studies on this front generally support the conclusion that poor academic performance (e.g., grade point average) can be predicted by higher levels of SP/D use, instant messaging, social networking, media multitasking, and general electronic media usage.19 Some of this may depend on the a person’s cognitive skill set, ability to exert self-regulatory control over behavior, interruptions and resultant stress and working memory capacity as a predictor of the speed of task resumption following an interruption.68 Other things like diet, exercise, sleep and mood may also indirectly affect measurement of these issues.
SMARTPHONE/DEVICE APPS IN MENTAL HEALTH AND CLINICAL SKILLS/COMPETENCIES
Broad areas of research are clinician-to-clinician, clinician-to-patient and patient as mobile compared to stationery. Clinicians need a framework6 and skills/competencies1 to meet needs of consumers, patients, caregivers and other providers related to technology. mH and other technologies alter care in terms of communication, boundaries and privacy/confidentiality. Overall, clinicians are encouraged to screen what technology is being used, how and when. Second, there are questions about how mH care fits with traditional care and affects the therapeutic relationship.69 Third, people and patients need education on using the “right” technology at the “right” time (e.g., not using an app or text to express suicidal ideation). Fourth, the advantages of empowerment, in-time learning and increased self-efficacy need to outweigh liabilities. Finally, clinicians (and patients) need research, select and evaluate technology as part of a treatment plans.
Participants in care need to evaluate how good the technology is (e.g., psych/mental health apps for SP/Ds).70 A review of 5465 abstracts on mental health apps (i.e., depression, anxiety, substance use, sleep disturbances, suicidal behavior, self-harm, psychotic disorders, eating disorders, stress, and gambling) delivered on mobile devices with a pre- to posttest design or compared with a control group.71 Only 8 papers describing 5 apps met the criteria (e.g., depression, anxiety and substance abuse) and 4 apps provided support from a mental health professional.
Mobile BH (mBH) or m Mental Health (mMH)
With regard to mBH, a review of 677 mobile phone and web-based text messaging papers in BH found 36 data-based ones, revealing that text messaging was used in a wide range of mental health situations, notably substance abuse (31%), schizophrenia (22%) and affective disorders (17%).72 Studies have described four ways in which text messages are used from the clinician to the patient: 1) reminders (14%); 2) information (17%); 3) supportive messages (42%); and 4) prompts for self-monitoring procedures (42%); combination use was common, too.72,73 Apps are also used for other functions, including: 5) communicating with other patients, caregivers, social supports or providers; 6) augmenting psychotherapy; 7) (smart) monitoring, that is, to using tools to predict relapse behavior or worsening affective symptoms, through sensors and data activity; 8) practicing self-assessment and care through reflection about their symptoms; and 9) facilitating interactive learning.69,73,74
Various mobile apps, especially those focusing on self-help in dealing with anxiety disorders, wellness and stress reduction,are not designed to act as a substitute for treatment. But they have been adjusted so specific patient groups (e.g., “Fear Fighter”, computer guided self-exposure approach to treat phobia/panic disorder; e.g., PTSD Coach from the National Center for Telehealth and Technology to learn about and manage trauma).6 Exposure therapy is effective for phobia/panic, but some patients prefer technology and qualified therapists are scarce; this increases healthcare efficiency. Soldiers prefer to complete psychometric measures (e.g., Patient Health Questionnaire or PHQ-9) and other military population measures by iPhone rather than paper or computer due to its interface, portability, and convenience.75
A systematic review of the effectiveness of online services in facilitating MH help-seeking in young people aged 14-25, emphasizing rigorous designs (N=18) showed high satisfaction and higher use by females.76 Many patients migrate to sites like PatientsLikeMe (http://www.patientslikeme.com/), a consumer driven site where individuals connect with others in the community who are experiencing similar medical issues. Young people with developmental challenges may have few traditional care options and feel more comfortable anonymously or at a distance, to share experiences and try to learn new behaviors.77 Comfortable with internet-based chats and groups, they may even express ideas of self-harm, negative affective states, or pessimistic cognitions of other peers.78 This is concerning, though, if these things are not shared with parents and/or professionals.
Common prejudice is that psychotic patients are not eligible for mH options due to poor concentration, lack of energy and paranoia. Non-attendance to treatment is common79 due to stigma and poor insight, but direct or remote education, motivation and support may increase attendance via treatment readiness and greater recognition of treatment benefits.80 Seriously mentally ill patients have also successfully used the Internet to learn about illness and medication (e.g., side effects and the hope of finding better medication)81,82 via EMA options.83 Research shows better concordance between clinician-rated affective symptoms and SP/D-captured mood ratings (compared to paper-and-pencil ratings by patients). Presentation of summary feedback in graphical form helps users learn about temporal sequencing of behaviors.84
Competencies, Education and Training
The international organization for migration (IOM’s) core competencies for the health professions include the ability to provide patient-centered care, work in interdisciplinary teams, employ evidence-based practice, apply quality improvement and use information technology.5 Learner-centered skills more than knowledge require that teaching and assessment methods align.85 The most common US framework used being the Accreditation Council for Graduate Medical Education (ACGME), which uses domains of patient care, medical knowledge, practice based learning and improvement, systems based practice, professionalism, and interpersonal skills and communication.86 Another useful framework is the evidence-based CanMEDS, which frames knowledge, skills and abilities into seven roles that all physicians play: medical expert, communicator, collaborator, manager, health advocate, scholar and professional.87
TP competencies have been published using the ACGME domains and with a teaching, supervisory and evaluation plan88; medication competencies have also been added.89 Novice/advanced beginner, competent/proficient (and expert levels were suggested. Subsequently, an interprofessional, evidence-based framework for measurable TBH competencies organizes seven Competency Domains: 1) Clinical Evaluation & Care; 2) Virtual Environment & Telepresence; 3) Technology; 4) Legal & Regulatory Issues; 5) Evidence-Based & Ethical Practice; 6) Mobile Health and Apps and 7) Telepractice Development.90 The competency literature has also recently grown with specific additions to social media competencies91 and mH and app competencies.92
mH poses challenges for competencies compared to in-person and telepsychiatric care, mainly as it is synchronous and anytime/anywhere – conceivably organized in a 24-hours per day and 7-days per week framework.92 Since many professionals often use the same SP/D for professional and personal life – mH is therefore “live”. mH care may also be “outside” the clinical visit, but it may affect the therapeutic frame and create additional boundary issues and be disruptive.1 If it is conducted over public, private and health system sites/apps, data integration and security may be difficult. Not all patients may be suitable for mH, which is very different than for in-person and telepsychiatric care. Finally, ethical issues are involved as SP/Ds collect sensitive information (e.g., personal information, geo-location, physiological activity, self-reports of mood and cravings and the consumption of drugs).93
An example mH, SP/D and Apps Competency for Patient Care Evaluation and Treatment would include history taking, engagement and interpersonal skills, assessment, education and management and treatment planning.88,92 It also includes administration, documentation and medico-legal issues such as privacy, confidentiality, safety, data protection/integrity and security. Clinicians reflect with patients on the pros/cons of the use of mH, SP/D and apps as part of treatment document this in the consent form or progress notes. This may include, but not be limited to, the competent/proficient clinician selecting the SP/D option based on patient preference, skill and need (i.e., purpose). S/he may also find it helpful to know if the patient uses SP/D and apps for personal life, healthcare and/or BH care, and seeing if the patient is aware of risks (e.g., privacy, self-disclosure, potential for cyberbullying) (Table 2).
| Table 2. Tips on Evaluating Outcomes Related to New Technology Options (e.g., SP/D, APPS). |
| Fundamental issues and components of evaluating care |
| 1 |
Keep it simple by picking 1-2 foci to evaluate (e.g., depression as a diagnosis; the impact of one technology like mobile apps). |
| 2 |
Use a known standard of evaluation (i.e., Patient Health Questionnaire-9; PHQ-9 for depression; adapt a telepsychiatric satisfaction instrument for a mobile app)? |
| 3 |
Customize patient outcome targets (e.g., social engagement if that had lessened due to depression; how the mobile health helped), |
| 4 |
Measure satisfaction with an existing 5– to 10–item survey for regular care and one technology options (e.g., a chat room or a diary for depression), |
| 5 |
Contextualize the evaluation with a specific population or clinical setting
a. Age or population (e.g., for patients over 60; outpatient; use of substance by screening with the Alcohol Use Disorders Identification Test (AUDIT))
b. Disorder-specific (e.g., plan for tracking suicidal ideation for a depressed patient, in general, or if a teenager due to high risk),
|
| 6 |
Employ a log/diary by the patient and the clinician about
a. The experience, overall,
b. How and what technology was used and the relative frequency, too (e.g., texting 3 times/week).
|
| 7 |
Can the technology help us use resources better, as interdisciplinary teams’ members (e.g., care coordinators) help us in providing a range of services in stepped care? |
| 8 |
What additional resources (i.e., time, $, staff/manager/medical director/administrative director, trainings) are necessary to use new technologies? |
| Questions, reflections and considerations for patients |
| 9 |
What am I seeking when I choose to view a website, visit a chat room, get an informal suggestion or work with a clinician directly? |
| 10 |
What are my means: time, $, and other resources? |
| 11 |
What is my learning style: alone vs. group of learners, reading versus doing something, prefer a little versus a lot of instruction? |
| 12 |
Am I self-assessing, part of a support group or engaging in ‘real’ treatment – in which I work with a clinician? |
| 13 |
How do I pick the “best” technology option? |
| Clinical care issues for the provider related to patient care |
| 14 |
Do the new technologies and associated behaviors affect the therapeutic relationship, clinical approach and treatment plan? |
| 15 |
What are the technology pros and cons? |
| 16 |
Did the patient and I talk about the options, work together to select the plan, and how should be continue to discuss this? |
Evidence-based Practice and Research
Parameters and methods fall into three basic frameworks that naturally overlap with one another: 1) research measures, in the form of feasibility, validity, reliability, satisfaction, costs and outcomes; 2) clinical care measures (e.g., mood questionnaires; habit diaries; utilization of health services); and 3) customized measures for technologies.1,53 Suggestions are to:
- Pick 1-2 things to measure rather than trying to measure everything; for an app for substance issues, monitor how frequently is the app used, frequency of near misses of or actual use of substances.
- Pick an outcome that has high heuristic value (e.g., substance relapse; averted suicide; frequency of increased visits cued by using an app).
- Adopt standardized measures already used in the literature; they typically have undergone multiple iterations, levels of review and psychometric testing.
- Use a readily available, easy to use self-report instrument or program.
- Collect data prospectively rather than retrospectively, with some exceptions.
- If possible, pick a regular evaluation interval (e.g., beginning and then 3-, 6- and 12-months).
- Identify who has the responsibility to prevent, identify, and correct the issues: patients, providers, or programs?
DISCUSSION
Technology is frequently used, is readily accessible and satisfies persons, patients and caregivers94 and is transforming the way health information is accessed, delivered and managed. The healthcare industry is able to distribute and deliverservices, partly due to cloud computing via fourth-generation (4G) mobile communications systems is the main responsible for enabling these advents.95 When people and patients – or trainees and clinicians/supervisors – use technology, personal experience may only partially translate to professional skill, hence the need for competencies. All participants, too, must reflect on when, why and how to use technology, in terms of getting things done versus engaging with others. Furthermore, they have to consider the cognitive pros and cons (e.g., attentional problems that make multi-tasking not really true multi-tasking).
Clinicians have to adapt clinical care using these new technology options in order to provide the best care – this means new advisory roles to explore patients’ experiences, preferences and skills in using them with regular in-person care.1,53 Standards for professionalism, privacy/confidentiality, tracking of data, evaluation and general practice management are affected by most of these technologies – not just by social media, texting and e-mail. Evidence-based research for a common vocabulary and set of quality standards for health apps would benefit both end users, industry participants and governments.1 Relatively few studies assess outcomes, compare in-person and eMH care, and or compare technology-based care options to one another; hybrid models of care have emerged, but have not been studied.
A dilemma exists, currently, in which neither public nor private, top-down nor bottom-up, and country-specific nor international approaches related to apps is providing a framework to develop, evaluate and regulate to mH care – the result is a chaotic mix of apps of varying degrees of usefulness, quality, effectiveness and danger. Ideally, such a consortium would be open to all who are involved in healthcare, including consumers, clinicians, academia, business, technology, education, and professional and advocacy organizations.96 Creation and adoption of review standards by an international, interdisciplinary consortium could reduce many of the barriers currently keeping mH technologies from becoming routine in providing healthcare worldwide.
Limitations to this review of mH, SP/Ds and apps are many. The scope and methods of the review was limited. Second, the metrics of a more detailed approach to design, implementation and evaluation need to be spelled out, preferably with users’ competencies measured. Third, for both cross-sectional and longitudinal trajectories, with qualitative and quantitative evaluation of participants is suggested to iteratively improve the process. Research is needed on organization change with technology and how a paradigm shift like mH re-contextualizes digital healthcare. Finally, a broader consensus across organizations (e.g., American Medical Association, American Telemedicine Association) is needed.
CONCLUSIONS
mH, telemedicine and other services are considered part of a telehealth or e-health spectrum of care. Technology usually offers portability for access anytime/anywhere, are relatively inexpensive and have additional features (e.g., context-aware interventions and sensors with real-time feedback). The evidence-based literature shows that many people have an openness to technology as a way to engage others, change behaviors and obtain clinical services. Skills/competencies for mobile health, SP/Ds and app have similarities and differences from in-person and telepsychiatric care. Cognitive function related to SP/Ds and app use may be affected by these technologies – particularly attention, memory and delay of gratification. More research is needed with respect to health services delivery models, effectiveness, competency outcomes and how a paradigm shift like mobile health re-contextualizes digital healthcare.
DISCLOSURE(S)/CONFLICTS OF INTEREST(S)
None.
ACKNOWLEDGMENTS
American Telemedicine Association, Telemental Health Special Interest Group Coalition for Technology in Behavioral Science.