CASE REPORT
An otherwise healthy 11-year-old boy underwent an elective circumcision at the age of five for phimosis with a normal healing. The boy began to develop pain associated with erections at the age of nine. He had presented his concern multiple times to his general practitioner, hospital and urologists for 2 long years. Despite his condition being correctly diagnosed, he was managed conservatively due to lack of a well-established intervention.
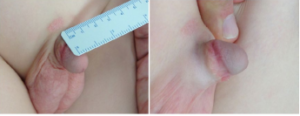
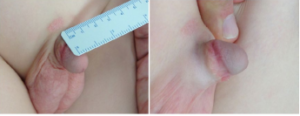
On examination, the flaccid length of his penis was 2 cm with the skin while under tension. The boy reported that his penis did not increase in length with an erection and this was associated with exquisite pain. The cause of the pain was attributable to the skin of the penis, for not being able to accommodate the penis during the erectile state (Figure 1).
Figure 1: Pre-operative Images of the Partially Buried Penis.
A decision was made to release the skin of the penis, and cover the defect with a split skin graft from the inguinal region. This site was chosen for a donor site as it is hairless, and soft and closely resembling the skin of the penis.
The operation was performed with parent’s consent of the patient and broad-spectrum antibiotics were administered on induction. During the procedure, the skin overlying the shaft was released distally at the site of previous incision from the circumcision, resulting in a 3 cm skin deficit. A carefully measured section of split skin was harvested with an scalpel blade of size 21 from the inguinal region, we didn’t use the dermatome due to the difficulty to make the area flat to use this device. The graft was macerated and grafted onto the penis shaft. The graft was sutured with interrupted 4.0 Biosyn sutures and 4.0 Vicryl Rapide quilting sutures. The graft was dressed under pressure with Bactigras gauze. The skin donor site was closed primarily (Figure 2).
Figure 2: Intra-operative Pictures Demonstrating Releasing of the Skin, the Resulting Skin Deficit and the Harvesting of Skin from the Anterior Abdominal Wall.

The patient was admitted for 48 hours under observation and analgesia. The dressings were left intact for 48 hours and when the dressing was taken down the graft was healthy and viable. At the time of discharge the graft and donor site were healing well. Community nurses managed daily dressings for a further three weeks. Analgesic requirement was minimal and managed in the community (Figure 3).
Figure 3: Day 2 Post-Operation

On follow-up at 3 weeks, the graft looked healthy, with no areas of breakdown or necrosis. The donor site was also healing well. On follow-up at 6 weeks the graft had taken well, but there was evidence of keloid scarring at the suture lines of the proximal and distal sections of the skin graft, as well as keloid scarring of the donor site. There was no history to suggest a propensity to form keloid scar. The patient then started on daily applications of hydrocortisone cream to the graft site as well as the donor site (Figure 4).
Figure 4: 6 Weeks Post-Grafting.

After following the above mentioned procedures for 6 months, the graft had taken well, the symptomatic painful erections had resolved and the patient was pleased with the result and the overall cosmesis. The keloid scarring responded well to the steroid cream and did not interfere with the erectile function of the penis (Figure 5).
Figure 5: 6 Months Post-Procedure Showing Healed Skin Graft.

We continued follow-up of this patient for 2 years and the patient did not develop any contracture and the graft grew with the penile growth without producing any deformity. As the patient reaches puberty and the penis has a tendency to growth in size, the patient needs to be reviewed to check if the graft produces any contracture.
DISCUSSION
Male circumcision is a common surgical procedure having been performed on 30% of the worldwide population.1,2 It is subject to continue debate with varying public attitudes with some evidence supporting circumcision for hygiene purposes and prophylaxis of penile cancer. As with all surgical procedures, there is a complication rate and depending on the skill and training of the individual performing the circumcision, this can be as high as 15% with the median complication rate being 1.6%.3
While a common procedure, if done incorrectly, it can have long-term, and debilitating complications, affecting sexual function, as well as significantly impacting the mental and emotional state of the individual.
Excessive excision of skin during circumcision results in a buried penis, leaving insufficient skin to accommodate the full length of the penis particularly during an erection. This can result in pain associated with erections, decreased penis length, impaired sexual function and poor aesthetic appearance. There is little data available on the rate of this complication, but the rate of complication is likely very under-reported and under-treated. This case report describes the use of split skin graft to correct a complication of excessive skin excision during circumcision.
There have been numerous techniques described to correct this complication including; healing by secondary intention, dorsal Z-plasty for small skin deficits, and skin re-surfacing.4 Techniques that have been described to correct this defect are complex and have high rates of failure, complicated and poor cosmetic results. The challenges with providing skin coverage for the penis shaft differ from other parts of the body in that the penis requires the ability to accommodate the elongation and engorgement during erection, as well as cosmesis, and preservation of sensation.
To correct a skin defect from a buried penis, the use of autologous free skin grafts from a hairless and subtle donor site have the benefit of being able to correct a greater defect than Z-plasty or scrotal skin advancement, while preserve the surrounding anatomy and give a greater cosmetic outcome. The use of split skin graft for skin resurfacing of the penis is not a frequently described method in the literature with only two cases reported in the last five years.5,6 However, as demonstrated by this case, it is a simple yet effective technique that can be utilised to correct a large skin defect as well as to maintain the function of the skin excised during the circumcision.
The donor site we recommend is the skin above the level of the inguinal region, easy to harvest and good quality skin due to his elasticity, softness and hairless, making this region ideal to replace the skin in the penile shaft with good cosmetic and functional effect. This region can provide grafts big enough to cover the whole shaft of the penis without leaving big and anaesthetic scars in the harvesting area. The use of split skin graft decreases and diminishes the scaring and retraction of the graft compared with the full thickness.
This technique can be used in paediatric and adult patients that need a big size graft. We have been using this method in a Burmese patient with an indurated shaft of the penis due to injection of Benzene that covers the full length of the penis. A split skin graft from the groin was used to cover the full length of the penis, from base to glans with a good cosmetic and functional result and with a small lineal scar in the donor site.
CONCLUSION
Radical skin excision during routine circumcision is an under reported complication, one that can have profound effects on the individual including pain, self esteem and sexual function, and mostly left untreated, with a great impact in the individual. This complication can be avoided by taking extra precautions during circumcision. We can see in this case, free split skin grafting is an alternative method for correcting large skin deficit of the penis following excessive skin excision of circumcision, and is suitable for use in children and adults.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
Consent has been taken from the patient for purpose of using patient photographs for publication in print or on the internet.