Organ supply is the greatest limitation to organ transplantation nowadays. Among the factors that can affect organ supply favourably, donor management has received the least attention. To meet the increased need for transplantable organs, medical staff should develop ways for optimal recognition of maintenance of donors. With an increased awareness of the problems and needs of the donor and the application of a rational physiological approach, the supply of functional organs for transplantation can be boosted. The importance of establishing an acceptable method of rapidly and accurately determining brain death (BD) in potential donors cannot be overemphasized. The organ transplantation community has invoked the Uniform Determination of Death Act to informally establish the “Dead Donor Rule” which states that one can only retrieve vital organs after the declaration of death.1
DEFINITION AND CRITERIA FOR BRAIN DEATH
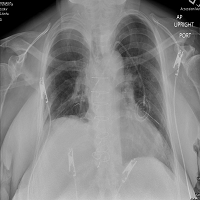
The clinical evaluation comprise documenting the complete absence of function of the entire brain and brainstem. This includes complete loss of consciousness, no spontaneous movements, no reaction to stimuli, no function or reflexes of the cranial nerves, and no spontaneous breathing during apnea testing.1
The prerequisites that should have been sought for before evaluating the patient for BD include being on a ventilator in a coma and displaying a clear cause of serious brain damage such as traumatic brain injury. Subarachnoid hemorrhage, cerebral abscess or neoplasm, meningitis and cerebral hypoxia from all causes can also lead to BD. Reversible causes such that hypothermia and intoxication should be ruled out.
Five brain stem reflexes should be absent to diagnose brain stem death: pupillary light response; corneal reflex to touch; vestibulo-ocular reflex using the cold caloric test; the gag reflex; and the apnoea test. Transcranial Doppler (TCD) sonography demonstrates the cessation of brain perfusion. These adjunctive studies may also comprise serial electroencephalography (EEG) and radionuclide scan to evaluate cerebral blood flow.
In 1981, the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research declared principles for the identification of BD. The ‘Uniform Determination of Death Act’ was developed, outlining neurological criteria for the diagnosis of BD in patients whose cardiopulmonary function is being artificially maintained.2,3
Harvard criteria for BD are summarized in Table 1. These items are to be sought for before establishing the diagnosis. Of note, the US Centers for Medicare and Medicaid Services mandates a referral of any patient with an acute brain injury with “imminent death,” which can be interpreted as a Glasgow Coma Score of <4 or 5.4
| Table 1: Harvard Criteria for Brain Death. |
| 1. Absence of spontaneous muscular movements or spontaneous respiration or response to stimuli. An apnoea test as indicated by the absence of spontaneous breathing while the respirator is off for 3 minutes may also serve as an adjunct to the diagnosis of BD.
2. Absence of reflexes. The pupils are fixed and dilated and do not respond to light. Ocular movement (to head turning and irrigation of the ears with ice water) and blinking are absent. Corneal and pharyngeal reflexes are absent. The stretch tendon reflexes cannot be elicited.
3. Flat or isoelectric electroencephalogram. |
EVALUATION AND MANAGEMENT OF THE POTENTIAL DONOR
In the last decade, euthanasia and organ recovery has been performed on patients in whom the decision to withdraw support has been made.5 Any patient who has been brain dead or who is planned to be deprived of life support measures should be seen as a candidate for organ donation. Most clinicians and ethicists believe in the appropriateness of the Dead Donor Rule (DDR), which states that vital organs should only be recovered from people who have died.1 Healthcare personnel need to be proficient on a clear protocol for communicating with the families of such patients. Once the patient receives the diagnosis of BD and while the patient remains on a ventilator, the patient’s family should be clearly informed that the patient has died. At that time, organ donation may be discussed.
After announcing BD and receiving informed consent from first-degree relatives, the management of the patient should focus on preservation of the function of donor organs.6 This is generally carried out in the intensive care unit (ICU), but it should begin in the ED. The needs specific to the organs to be transplanted should be taken into account when outlining the treatment strategy.
Because of the dearth of research in this field, the pluses and minuses of strategies for preserving organ function and improving recipient outcomes are uncertain.7 Maintaining haemodynamic stability in the donor optimizes organ function and improves the chances of successful results in transplant recipients.
The goal of emergency management strategies consists of normalization of physiological status in the organ donor to preserve organ function for transplantation.8 Clinicians need to provide vasoactive medications, lung-protective mechanical ventilation, hormone supplementation, nutrition, electrolyte and glucose control, systemic anticoagulation along with haemodynamic monitoring and bronchoscopy.7,8
In cases in which haemorrhage is controlled, if any, and adequate circulating volume has been established, inotropic treatment may be required. The initial rate of infusion is 2-4 L crystalloid with the endpoint of a systolic blood pressure (SBP) of 100 mmHg and above.6 The general objective ‘Rule of 100’ has been formulated by Gelb and Robertson9 and was detailed in Table 2.
| Table 2: The ‘Rule of 100’. |
| Maintain: Systolic blood pressure (SBP) greater than 100 mmHg
Urine output greater than 100 ml/h PaO2 greater than 100 mmHg
Haemoglobin concentration greater than 100 g/l
PaO2 , Arterial oxygen tension. |
In patients whose SBP levels are stil below 100 mmHg in spite of a central venous pressure level above 10 cm H2 O, sympathomimetic agents such as dopamine should be administered. Dopamine is recommended to start at a rate below 10 mg/kg per minute. An aggressive, proactive approach to the medical management of the potential donor is recommended in order to limit the number of medical failures and maximize the number of organs donated.
In conclusion, treating patients with BD is a real challenge for caregivers, including the staff in the ED. Cardiovascular and respiratory disorders and metabolic and electrolyte changes prompt close monitoring and expedient management. Drug and fluid resuscitation in the patient have firm limits and guidelines that are of great importance to retrieval and transplant teams, and most of all, the recipient of the optimally perfused organ.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.