1. Weckstein LM, Masserman JSH, Gaite TJ. Placenta accrete: A problem of increasing clinical significance. Obstet Gynecol. 1986; 69: 480-482. Web site. https://www.ncbi.nlm.nih.gov/pubmed/3808530. Accessed December 15, 2016
2. Khan M, Sachdeva P, Arora R, Bhasin S. Conservative management of morbidity adherent placenta- A case report and review literature. Placenta. 2013; 34: 963-966. doi: 10.1016/j.placenta.2013.04.016
3. Morison JE. Placenta accrete. A clinicopathologic review of 67 cases. Obstet Gynecol Annu. 1978; 7: 107-123. Web site. https://www.ncbi.nlm.nih.gov/pubmed/662213. Accessed December 15, 2016.
4. Miller D, Cholletr JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accrete. Am J Obtet Gynecol. 1997; 177: 210-214. doi: 10.1016/S0002-9378(97)70463-0
5. Kistner RW, Hertig AT, Reid DE. Simultaneously occurring placenta previa and placenta accrete. Surg Gynecol Obstet. 1952; 94: 141-151. Web site. https://www.ncbi.nlm.nih.gov/pubmed/14901248. Accessed December 15, 2016.
6. Clark SL, Koonings PP, Phelan JP. Placenta previa accrete and prior cesarean section. Obstet Gynecol. 1984; 66: 89-92. Web site. https://www.ncbi.nlm.nih.gov/pubmed/4011075. Accessed December 15, 2016.
7. Rossi AC, Lee RH, Chmait RH. Emergency postpartum hysterectomy for uncontrolled postpartum bleeding: A systematic review. Obstet Gynecol. 2010; 115: 637-644. doi: 10.1097/AOG.0b013e3181cfc007
8. Wright JD, Pri-Paz S, Herzog TJ, et al. Predictors of massive blood loss in women with placenta accrete. Am J Obstet Gynecol. 2011; 205: 38e1-6. doi: 10.1016/j.ajog.2011.01.040
9. Bateman BT, Mhyre JM, Callaghan WM, Kukina EV. Peripartum hysterectomy in the United States: Nationwide 14 year experience. Am J Obstet Gynecol. 2012; 206: 63 e1-8. doi: 10.1016/j.ajog.2011.07.030
10. Eshkoli T, Weintraub Ay, Sergienko R, Sheiner E. Placenta accrete: Risk factors, perinatal outcomes, and consequences for subsequent births. Am J Obstet Gynecol. 2013; 208: 219.e1-e7. doi: 10.1016/j.ajog.2012.12.037
11. Lloyd-Jones R, Winterton WR. Spontaneous rupture of the uterus due to placenta percreta: A case report. J Obstet Gynecol Br Common. 1961; 68: 273-276. Web site. https://www.ncbi.nlm.nih.gov/pubmed/8697340. Accessed December 15, 2016.
12. O’Brien JM, Barton JR, Donaldson ES. The management of placenta percreta: Conservative and operative strategies. Am J Obstet Gynecol. 1996; 175: 1632-1638. doi: 10.1016/S0002-9378(96)70117-5
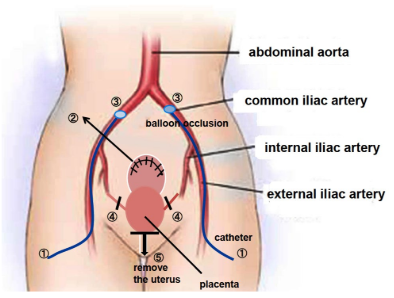
13. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: Balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997; 176: 723-726. Web site. https://www.ncbi.nlm.nih.gov/pubmed/9077641. Accessed December 15, 2016.
14. Ojala K, Perälä J, Kariniemi J, Ranta P, Raudaskoski T, Terkay A. Arterial embolization and prophylactic catheterization for the treatment for severe obstetric hemorrhage. Acta Obstet Gynecol Scand. 2005; 84: 1075-1080. doi: 10.1111/j.0001-6349.2005.00727.x
15. Tan CH, Tay KH, Steah K, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. AJR. 2007; 189: 1158-1163. doi: 10.2214/AJR.07.2417
16. Carnevale FC, Kondo MM, de Oliveira Sousa W Jr, et al. Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accreta. Cardiovasc Intervent Radiol. 2011; 34: 758-764. doi: 10.1007/s00270-011-0166-2
17. Hishikawa K, Koshiyama M, Ueda M, et al. Exchange of intraoperative balloon occlusion of the internal iliac artery for the common iliac artery during cesarean hysterectomy in a patient with placenta percreta. Am J Case Rep. 2013; 14: 409-411. doi: 10.12659/AJCR.889449
18. Jaffe R, DuBeesheter B, Sherer DM, Thompson EA, Woods JR Jr. Failure of methotrexate for the term placenta percreta. Am J Obstet Gynecol. 1994; 171: 558-559.doi: 10.1016/0002-9378(94)90300-X
19. Veenstra M, Spinder T, Dekker GA, van Geijin HP. Post partum intra-abdominal hemorrhage due to placenta percreta. Eur J Onstet Gynecol. 1995; 62: 253-256. doi: 10.1016/0301-2115(95)02183-8
20. Knuttinen MG, Jani A, Gaba RC, Bui JT, Carrillo TC. Balloon occlusion of the hypogastric arteries in the management of placenta accrete: A case report and review of the literature. Semin Intervent Radiol. 2012; 29: 161-168. doi: 10.1055/s-0032-1326924
21. Levine AB, Kuhlman K, Bonn J. Placenta accreta: Comparison of cases managed with and without pelvic artery balloon catheters. J Matern Fetal Med. 1999; 8: 173-176. doi: 10.1002/(SICI)1520-6661(199907/08)8:4<173::AID-MFM7
>3.0.CO;2-V
22. Bodner LJ, Nosher JL, Gribbin C, Siegel RL, Beale S, Scorza W. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol. 2006; 29: 354-361. doi: 10.1007/s00270-005-0023-2
23. Shih JC, Liu KL, Shyu MK. Temporary balloon occlusion of the common iliac artery: New approach to bleeding control during cesarean hysterectomy for placenta percreta. Am J Obstet Gynecol. 2005; 193: 1756-1758. doi: 10.1016/j.ajog.2005.08.033
24. Matsubara S, Nonaka H, Kobayashi M, Kuwata T, Fujii H. Intrauterine balloon occlusion during cesarean hysterectomy for placenta previaaccreta: The internal or common iliac artery? Acta Obstet Gynecol Scand. 2014; 93: 122-123. doi: 10.1111/aogs.12273
25. Clausen C, Stensballe J, Albrechtsen CK, Hansen MA, Lonn L, Langhoff-Roos J. Balloon occlusion of the internal iliac arteries in the multidisciplinary management of placenta percreta. Acta Obstet Gynecol Scand. 2013; 92: 386-391. doi: 10.1111/j.1600-0412.2012.01451.x
26. Nishida Y, Hirakawa T, Utsunomiya Y, Tsusue H, Narahara H. Transfundal uterine incision performed with prophylactic common iliac artery balloon occlusion for patient with placenta previatotalis. Clin Med Insights Case Rep. 2012; 5: 93-97. doi: 10.4137/CCRep.S9777
27. Minas V, Gul N, Shaw E, Mwenenchanya S. Prophylactic balloon occlusion of the common iliac arteries for the management of suspected placenta accreta/percreta: Conclusions from a short case series. Arch Gynecol Obstet. 2015; 291: 461-465. doi: 10.1007/s00404-014-3436-9
28. Chou MM, Kung HF, Hwang JI, Chen WC, Tseng JJ. Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation.Taiwan J Obstet Gynecol. 2015; 54: 493-498. doi: 10.1016/j.tjog.2014.03.013
29. Sewell MF, Rosenblum D, Ehrenberg H. Arterial embolus during common iliac balloon catheterization at cesarean hysterectomy. Obstet Gynecol. 2006; 108: 746-748. doi: 10.1097
/01.AOG.0000201992.80130.2c
30. Matsueda S, Hidaka N, Kondo Y, Fujiwara A, Fukushima K, Kato K. External iliac artery thrombosis after common iliac artery balloon occlusion during cesarean hysterectomy for placenta accreta in cervico-isthmic pregnancy. J Obstet Gynecol Res. 2015; 41: 1826-1830. doi: 10.1111/jog.12777
31. Brigham and Women’s Hospital. Caring for the placenta accreta patient. Web site. http://www.brighamandwomens.org/Departments_and_Services/obgyn/Medical_Professionals/caring-for-placenta-accerta-patient.aspx#pageheadline. Accessed June 30, 2016.
32. de la Cruz CZ, Coulter ML, O’Rourke K, Alio PA, Daley EM, Mahan CS. Women’s experiences, emotional responses, and perceptions of care after emergency peripartum hysterectomy: A qualitative survey of women from 6 months to 3 years postpartum. Birth. 2013; 49: 256-263. doi: 10.1111/birt.12070