1. World Health Organization (WHO). Obesity preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). 2000. Website. https://www. who.int/nutrition/publications/obesity/WHO_TRS_894/en/. Accessed April 10, 2020.
2. World Health Organization (WHO). Ten threats to global health in 2019. Website. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. Accessed April 10, 2020.
3. NG M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: Asystematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 30: 766-781. doi: 10.1016/S0140-6736(14)60460-8
4. Weihrauch-Blüher S, Schwarz P, Klusmann J-H. Childhood obesity: increased risk for cardiometabolic disease and cancer in adulthood. Metabolism. 2019; 92: 147-152. doi: 10.1016/j.metabol.2018.12.001
5. O’Rahilly S, Farooqi IS. Human obesity: A heritable neurobehavioral disorder that is highly sensitive to environmental conditions. Diabetes. 2008; 57: 2905-2910. doi: 10.2337/db08-0210
6. Pinto RM, Steinmetz LS, Barbosa JMG, Mendes AFCS, Curado MP, da Cruz AD. The role of genetics in the pathophysiology of obesity: A systematic review. Obes Res Open J. 2019; 6(1):11-17.
7. Larqué E, Labayen I, Flodmark C-E, Lissau I, Czernin S, Moreno LA, et al. From conception to infancy — early risk factors for childhood obesity. Nat Rev Endocrinol. 2019; 15: 456-478. doi: 10.1038/s41574-019-0219-1
8. Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: An endocrine society scientific statement. Endocr Rev. 2017; 38 (4): 267-296. doi: 10.1210/er.2017-00111
9. Oussaadaa SM, van Galena KA, Cooimanb MI, Kleinendorstc L, Hazebroekb EJ, van Haelst MM, et al. The pathogenesis of obesity. Metabolism. 2019; 92: 26-36. doi: 10.1016/j.metabol.2018.12.012
10. Gordon EL, Ariel-Donges AH, Bauman V, Lisa J Merlo. What Is the Evidence for “Food Addiction?” A Systematic Review. Nutrients. 2018; 10(4): 477. doi: 10.3390/nu10040477
11. King BM. The modern obesity Epidemic, ancestral huntergatherers, and the sensory/reward control of food intake. Am Psychol. 2013; 68(20): 88-96. doi: 10.1037/a0030684
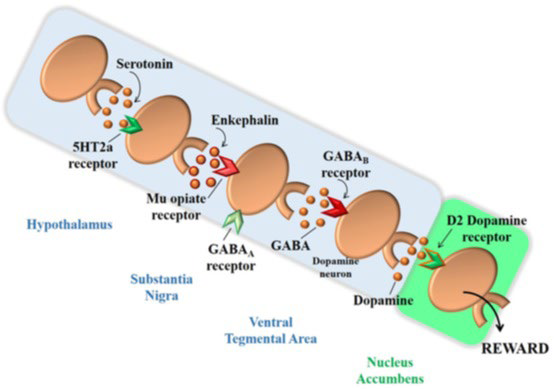
12. Pinto RM, Cominetti C, da Cruz AD. Basic and genetic aspects of food intake control and obesity: Role of dopamine receptor D2 TAQIA polymorphism. Obes Res Open J. 2016; 2(4): 119-127. doi: 10.17140/OROJ2-119
13. Böttcher Y, Körner A, Kovacs P, Kiess W. Obesity genes: Implication in childhood obesity. Pediatrics and Child Health. 2011; 22(1): 31-36. doi: 10.1016/j.paed.2011.08.009
14. Ford CP. The role of D2-autoreceptors in regulating dopamine neuron activity and transmission. Neuroscience. 2014; 282(12): 13-22. doi: 10.1016/j.neuroscience.2014.01.025
15. Blum K, Chen ALC, Giordano J, Borsten J, Chen TJH, Hauser M, et al. The addictive brain: All roads lead to dopamine. J Psychoactive Drugs. 2012; 44(2): 134-143. doi: 10.1080/02791072.2012.685407
16. Stice E, Yokum S, Bohon C, Marti N, Smolen A. Reward circuitry responsivity to food predicts future increases in body mass: moderating effects of DRD2 and DRD4. Neuroimage. 2010; 50: 1618-1625. doi: 10.1016/j.neuroimage.2010.01.081
17. Davis C, Levitan RD, Yilmaz Z, Kaplan AS, Carter JC, Kennedy JL. Binge eating disorder and the dopamine D2 receptor: Genotypes and sub-phenotypes. Prog Neuropsychopharmacol Biol Psychiatry. 2012; 38: 328-335. doi: 10.1016/j.pnpbp.2012.05.002
18. Davis C, Levitan RD, Kaplan AS, Carter J, Reid C, Curtis C, et al. Reward sensitivity and the D2 dopamine receptor gene: A casecontrol study of binge eating disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2008; 32(3): 620-628. doi: 10.1016/j.pnpbp.2007.09.024
19. Kvaløy K, Holmen J, Hveem K, Holmen TL. Genetic effects on longitudinal changes from healthy to adverse weight and metabolic status—The HUNT Study. PLoS One. 2015; 10(10): e0139632. doi: 10.1371/journal.pone.0139632
20. Gluskin B, Mickey BJ. Genetic variation and dopamine D2 receptor availability: A systematic review and meta-analysis of human in vivo molecular imaging studies. Transl Psychiatry. 20016; 6(3): e747. doi: 10.1038/tp.2016.22
21. Epstein LH, Temple JL, Neaderhiser BJ, Salis RJ, Erbe RW, Leddy JJ. Food reinforcement, the dopamine D2 receptor genotype, and energy intake in obese and nonobese humans. Behav Neurosci. 2007; 121: 877-886. doi: 10.1037/0735-7044.121.5.877
22. Clifton IJ, McDonough MA, Ehrismann D, Kershaw NJ, Granatino N, Schofield CJ. Structural studies on 2-oxoglutarate oxygenases and related double-stranded beta-helix fold proteins. J Inorg Biochem. 2006; 100: 644-669. doi: 10.1016/j.jinorgbio.2006.01.024
23. Speakman JR, Rance KA, Johnstone AM. Polymorphisms of the FTO gene are associated with variation in energy intake, but not energy expenditure. Obesity (Silver Spring). 2008; 16: 1961-1965. doi: 10.1038/oby.2008.318
24. Haupt A, Thamer C, Staiger H, Tschritter O, Kirchhoff K, Machicao F, Häring H-U, et al. Variation in the FTO gene influences food intake but not energy expenditure. Exp. Clin. Endocrinol. Diabetes. 2009; 117: 194-197. doi: 10.1055/s-0028-1087176
25. Tanofsky-Kraff M, Han JC, Anandalingam K, Shomaker LB, Columbo KM, Wolkoff LE, et al. The FTO gene rs9939609 obesity-risk allele and loss of control overeating. Am J Clin Nutr. 2009; 90: 1483-14889. doi: 10.3945/ajcn.2009.28439
26. Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. Int J Obes. 2009; 33: 42-45. doi: 10.1038/ijo.2008.174
27. Doaei S, Jarrahi SAM, Moghadam AS, Akbari ME, Kooshesh SJ, Badeli M, et al. The effect of rs9930506 FTO gene polymorphism on obesity risk: a meta-analysis. Biomol Concepts. 2019; 10: 237-242. doi: 10.1515/bmc-2019-0025
28. Jacobsson JA, Schiöt HB, Fredriksson R. The impact of intronic single nucleotide polymorphisms and ethnic diversity for studies on the obesity gene FTO. Obes Ver. 2012; 13: 1096-1109. doi: 10.1111/j.1467-789X.2012.01025.x
29. Cha SW, Choi SM, Kim KS, Park BL, Kim JR, Kim JY, et al. Replication of genetic effects of FTO polymorphisms on BMI in a Korean population. Obesity (Silver Spring). 2008; 16: 2187-2189. doi: 10.1038/oby.2008.314
30. Hong KW, Oh B. Recapitulation of genome-wide association studies on body mass index in the Korean population. Int J Obes. 2012; 36: 1127-1130. doi: 10.1038/ijo.2011.202
31. Villalobos-Comparán M, Flores-Dorantes MT, VillarrealMolina MT, Rodríguez-Cruz M, García-Ulloa AC, Robles L, et al. The FTO gene is associated with adulthood obesity in the Mexican population. Obesity (Silver Spring). 2008; 16: 2296-2301. doi: 10.1038/oby.2008.367
32. Wing MR, Ziegler J, Langefeld CD, Ng MCY, Haffner SM, Norris JM, et al. Analysis of FTO gene variants with measures of obesity and glucose homeostasis in the IRAS Family Study. Hum Genet. 2009; 125: 615-626. doi: 10.1007/s00439-009-0656-3
33. Dong C, Beecham A, Slifer S, Wang L, McClendon MS, Blanton SH, et al. Genome-wide linkage and peak-wide association study of obesity-related quantitative traits in Caribbean Hispanics. Hum Genet. 2011; 129: 209-219. doi: 10.1007/s00439-010-0916-2
34. Sun X, Luquet S, Small DM. DRD2: Bridging the genome and ingestive behavior. Trends Cogn Sci. 2017; 21 (5): 372-384. doi: 10.1016/j.tics.2017.03.004
35. Sevgi M, Rigoux L, Kühn AB, Mauer J, Schilbach L, Hess ME, et al. An obesity-predisposing variant of the FTO gene regulates D2R-dependent reward learning. J Neurosci. 2015; 35 (36): 12584- 12592. doi: 10.1523/JNEUROSCI.1589-15.2015
36. World Health Organization (WHO). Physical Status: the use and interpretation of antropometr, report of a WHO expert committee. 1995. Website. https://apps.who.int/iris/handle/10665/37003. Accessed April 10, 2021.
37. Bresolin NL. Hipertensão arterial na infância e adolescência: Manual de Orientação do Departamento Científico de Nefrologia [In: Portuguese]. Rio de Janeiro: Sociedade Brasileira de Pediatria. 2019.
38. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017; 140 (3): e20171904. doi: 10.1542/peds.2017-1904
39. Freedman DS, Serdula MK, Srinivasan SR, Berenson GS. Relation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: The bogalusa heart study. Am J Clin Nutr. 1999; 69: 308-317. doi: 10.1093/ajcn/69.2.308
40. Sociedade Brasileira de Pediatria (SBP). Guia pratico de avaliação: Novas orientações sobre o jejum para determinação laboratorial do perfil lipídico [In: Portuguese]. Sociedade Brasileira de Pediatria. 2017
41. American Diabetes Association. Children and adolescentes: standards of medical care in diabetes. Diabetes Care. 2018; 41(Suppl 1): S126-S136. doi: 10.2337/dc18-S012
42. Araz NC, Nacak M, Balci SO, Benlier N, Araz M, Pehlivan S, et al. Childhood obesity and the role of dopamine D2 receptor and cannabinoid receptor-1 gene polymorphisms. Genet Test Mol Biomarkers. 2012; 16(12): 1408-1412. doi: 10.1089/gtmb.2012.0244
43. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28: 412-419. doi: 10.1007/BF00280883
44. de Almeida CAN, Pinho AP, Ricco RG, Pepato, Iguatemy Lourenço Brunetti. Determination of glycemia and insulinemia and the homeostasis model assessment (HOMA) in schoolchildren and adolescents with normal body mass index. J Pediatr (Rio J). 2008; 84(2): 136-140. doi: 10.2223/JPED.1767
45. Ford ES, Li C. Defining the metabolic syndrome in children and adolescents: will the real definition please stand up? J Pediatr. 2008; 152(2): 160-164. doi: 10.1016/j.jpeds.2007.07.056
46. Zimmet P, Mm Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents – an IDF consensus report. Pediatr Diabetes. 2007; 8(5): 299- 306. doi: 10.1111/j.1399-5448.2007.00271.x
47. Magge SN, Goodman E, Armstrong SC, COMMITTEE ON NUTRITION; SECTION ON ENDOCRINOLOGY; SECTION ON OBESITY. The metabolic syndrome in children and adolescents: Shifting the focus to cardiometabolic risk factor clustering. Pediatrics. 2017; 140(2): e20171603. doi: 10.1542/peds.2017- 1603
48. Behravan J, Hemayatkar M, Toufani H, Abdollahian E. Linkage and association of DRD2 gene TaqI polymorphism with schizophrenia in an Iranian population. Arch Iran Med. 2008; 11(3): 252- 256.
49. Bouchard C. The genetics of human obesity. In: Handbook of Obesity. Nova York, USA: Marcel Dekker; 1998.
50. Rankinen T, Pérusse L, Weisnagel SJ, Snyder EE, Chagnon YC, Bouchard C. The human obesity gene map: The 2001 update. Obes Res. 2002; 10(10): 196-243. doi: 10.1038/oby.2002.30
51. Hainer V, Zamrazilová H, Spálová J, Hainerová I, Kunesová M, Aldhoon B, et al. Role of hereditary factors in weight loss and its maintenance. Physiol Res. 2008; 57(s. 1): S1-S15. doi: 10.33549/physiolres.931485
52. Borgeson M. The aetiology of obesity in children . A study of 101 twin pairs. Acta Paediatr. Scand. 1976; 65(3): 279-287. doi: 10.1111/j.1651-2227.1976.tb04887.x
53. Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa Nacional de Saúde 2013 Ciclos de vida Brasil e Grandes Regiões. 2015.
54. Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001; 161 (13): 1581-1586. doi: 10.1001/archinte.161.13.1581
55. Jaeger C, Brendel MD, Hering BJ, Eckhard M, Bretzel RG. Progressive islet graft failure occurs significantly earlier in autoantibody-positive than in autoantibody-negative IDDM recipients of intrahepatic islet allografts. Diabetes. 1997; 46(11): 1907-1910. doi: 10.2337/diab.46.11.1907
56. Kavaler S, Morinaga H, Jih A, Fan WQ, Hedlund M, Varki A, et al. Pancreatic beta-cell failure in obese mice with human-like CMPNeu5Ac hydroxylase deficiency. FASEB J. 2011; 25(6): 1887-1893. doi: 10.1096/fj.10-175281
57. Brown MS, Goldstein JL. Selective versus total insulin resistance: A pathogenic paradox. Cell Metab. 2008; 7(2): 95-96. doi: 10.1016/j.cmet.2007.12.009
58. Han T, Cheng Y, Tian S, Wang L, Liang X, Duan W, et al. Changes in triglycerides and high-density lipoprotein cholesterol may precede peripheral insulin resistance, with 2-h insulin partially mediating this unidirectional relationship: A prospective cohort study. Cardiovasc Diabetol. 2016; 15: 154. doi: 10.1186/s12933-016- 0469-3
59. da Silva CF, Zandoná MR, Vitolo MR, Bó Campagnolo PD, Rotta LN, Almeida S, et al. Association between a frequent variant of the FTO gene and anthropometric phenotypes in Brazilian children. BMC Med Genet. 2013; 14: 34. doi: 10.1186/1471-2350-14-34
60. Lourenço BH, Qi L, Willett WC, Cardoso MA, ACTION Study Team. FTO genotype, vitamin D status, and weight gain during childhood. Diabetes. 2014; 63: 808-814. doi: 10.2337/db13-1290
61. Reuter CP, Burgos MS, Bernhard JC, Tornquist D, Klinger EI, Borges TS, et al. Association between overweight and obesity in schoolchildren with rs9939609 polymorphism (FTO) and family history for obesity. J Pediatr. 2016; 92(5): 493-498. doi: 10.1016/j. jped.2015.11.005
62. do Nascimento GA, Teixeira MD, Furtado-Alle L, Leite N, de Souza RLR, Saliba LF, et al. FTO rs9939609 A allele influences anthropometric outcome in response to dietary intervention, but not in response to physical exercise program. Eur J Nutr. 2019; 58(1): 325-334. doi: 10.1007/s00394-017-1596-7
63. Todendi PF, de Moura Valim AR, Klinger E, Reuter CP, Molina S, Martínez JA, et al. The role of the genetic variants IRX3 rs3751723 and FTO rs9939609 in the obesity phenotypes of children and adolescents. Obes Res Clin Pract. 2019; 13: 137-142. doi: 10.1016/j.orcp.2019.01.005
64. de Araújo Pereira P, Alvim-Soares AM Jr, Sandrim VC, Lanna CMM, Souza-Costa DC, de Almeida Belo V, et al. Lack of association between genetic polymorphism of FTO, AKT1 and AKTIP in childhood overweight and obesity. J Pediatr (Rio J). 2016; 92 (5): 521-527. doi: 10.1016/j.jped.2015.12.007
65. Rodrigues LDS, Santos AMD, Lima MIS, Simões VMF, Pereira SR. Association between the FTO gene polymorphism and obesity in Brazilian adolescents from the Northeast region. J Pediatr (Rio J). 2020; 96(5): 630-637. doi: 10.1016/j.jped.2019.05.006
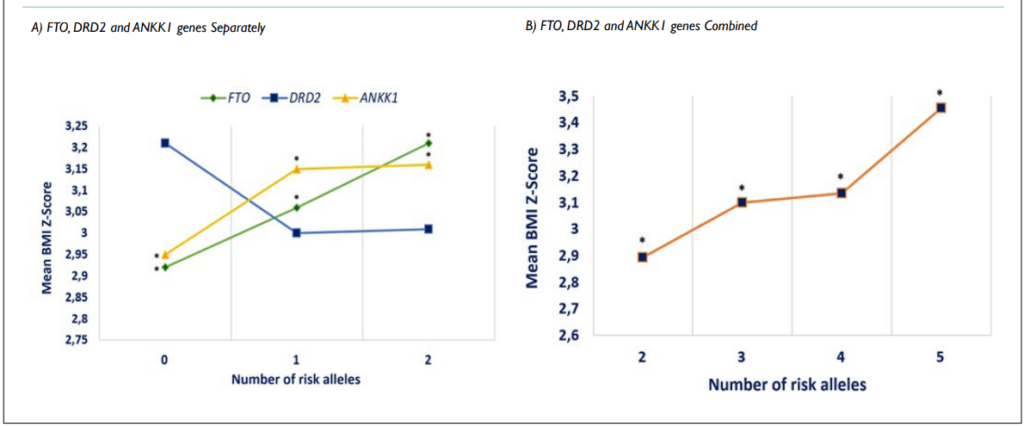
66. Heni M, Kullmann S, Ahlqvist E, Wagner R, Machicao F, Staiger H, et al. Interaction between the obesity-risk gene FTO and the dopamine D2 receptor gene ANKK1/TaqIA on insulin sensitivity. Diabetologia. 2016; 59: 2622-2631. doi: 10.1007/s00125-016-4095-0
67. Stock A-K, Arning L, Epplen JT, Beste C. DRD1 and DRD2 genotypes modulate processing modes of goal activation processes during action cascading. J Neurosci. 2014; 34(15): 5335-5341. doi: 10.1523/JNEUROSCI.5140-13.2014
68. Beste C, Stock A-K, Epplen JT, Arning L. Dissociable electrophysiological subprocesses during response inhibition are differentially modulated by dopamine D1 and D2 receptors. Eur Neuropsychopharmacol. 2016; 26(6): 1029-1036. doi: 10.1016/j.euroneuro.2016.03.002
69. Colzatoa LS, Steenbergena L, Sellaroa R, Stockb A-K, Arningc L, Beste C. Effects of l-Tyrosine on working memory and inhibitory control are determined by DRD2 genotypes: A randomized controlled trial. Cortex. 2016; 82: 217-224. doi: 10.1016/j.cortex.2016.06.010
70. Torre OHD, Paes LA, Henriques TB, de Mello MP, Celeri EHRV, Dalgalarrondo P, et al. Dopamine D2 receptor gene polymorphisms and externalizing behaviors in children and adolescents. BMC Med Genet. 2018; 19(1): 65. doi: 10.1186/s12881-018-0586-9
71. Zink N, Bensmann W, Arning L, Colzato LS, Stock A-K, Beste C. The role of DRD1 and DRD2 receptors for response selection under varying complexity levels: Implications for meta control processes. Int J Neuropsychopharmacol. 2019; 22(12): 747-753. doi: 10.1093/ijnp/pyz024
72. Mohammadi H, Joghataei MT, Rahimi Z, Faghihi F, Farhangdoost H. Relationship between serum homovanillic acid, DRD2 C957T (rs6277), and hDAT A559V (rs28364997) polymorphisms and developmental stuttering. J Commun Disord. 2018; 76: 37-46. doi: 10.1016/j.jcomdis.2018.08.003
73. Ramos-Lopez O, Panduro A, Rivera-Iñiguez I, Roman S. Dopamine D2 receptor polymorphism (C957T) is associated with sugar consumption and triglyceride levels in West Mexicans. Physiol Behav. 2018; 194: 532-537. doi: 10.1016/j.physbeh.2018.07.004
74. Eny KM, Corey PN, El-Sohemy A. Dopamine D2 receptor genotype (C957T) and habitual consumption of sugars in a freeliving population of men and women. J Nutrigenet Nutrigenomics. 2009; 2(4): 235-242. doi: 10.1159/000276991
75. 1000 Genomes Project Consortium; Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, et al. A global reference for human genetic variation. Nature. 2015; 526(7571): 68-74. doi: 10.1038/nature15393
76. Pinto RM, e Silva DM, Queiroz FJ, Godoy FR, Teodoro LS, Lacerda I, et al. Reward deficiency syndrome in children: obesity and metabolic disorders are associated with the SNP TaqIA C32806T of the DRD2 gene. Obes Res Open J. 2015; 2(2): 64-72. doi: 10.17140/OROJ-2-111
77. Yeh J, Trang A, Henning SM, Wilhalme H, Carpenter C, Heber D, et al. Food cravings, food addiction, and a dopamine-resistant (DRD2 A1) receptor polymorphism in Asian American College Students. Asia Pac J Clin Nutr. 2016; 25(2): 424-429. doi: 10.6133/apjcn.102015.05
78. Obregón AM, Valladares M, Goldfield G. Association of the Dopamine D2 receptor rs1800497 polymorphism with eating Behavior in Chilean children. Nutrition. 2017; 35: 139-145. doi: 10.1016/j.nut.2016.11.005
79. Cardel MI, Lemas DJ, Lee AM, Miller DR, Huo T, Klimentidis YC, et al. Taq1a polymorphism (rs1800497) is associated with obesity-related outcomes and dietary intake in a multiethnic sample of children. Pediatr Obes. 2019; 14(2): 12470. doi: 10.1111/ijpo.12470
80. Pijl H, Ohashi S, Matsuda M, Miyazaki Y, Mahankali A, Kumar V, et al. Bromocriptine a novel approach to the treatment of type 2 diabetes. Diabetes Care. 2000; 23(8): 1154-1161. doi: 10.2337/diacare.23.8.1154
81. de Leeuw van Weenen JE, Parlevliet ET, Maechler P, Havekes LM, Romijn JA, Ouwens DM, et al. The dopamine receptor D2 agonist bromocriptine inhibits glucose-stimulated insulin secretion by direct activation of α2-adrenergic receptors in beta cells. Biochem Pharmacol. 2010; 78: 1827-1836. doi: 10.1016/j.bcp.2010.01.029
82. Rubí B, Ljubicic S, Pournourmohammadi S, Carobbio S, Armanet M, Bartley C, et al. Dopamine D2-like receptors are expressed in pancreatic beta cells and mediate inhibition of insulin secretion. J Biol Chem. 2005; 280(44): 36824-36832. doi: 10.1074/jbc. M505560200
83. García-Tornadú I, Ornstein AM, Chamson-Reig A, Wheeler MB, Hill DJ, Arany E, et al. Disruption of the dopamine D2 receptor impairs insulin secretion and causes glucose intolerance. Endocrinology. 2010; 151(4): 1441-1450. doi: 10.1210/en.2009-0996
84. Epstein LH, Dearing KK, Erbe RW. Parent–child concordance of Taq1 A1 allele predicts similarity of parent–child weight loss in behavioral family-based treatment programs. Appetite. 2010; 55(2): 363-366. doi: 10.1016/j.appet.2010.06.006
85. Ergun MA, Karaoguz MY, Koc A, Camurdan O, Bideci A, Yazici AC, et al. The apolipoprotein E gene and Taq1A polymorphisms in childhood obesity. Genet Test Mol Biomarkers. 2010; 14(3): 343-345. doi: 10.1089/gtmb.2010.0002
86. van Strien T, Snoek HM, van der Zwaluw CS, Engels RCME. Parental control and the dopamine D2 receptor gene (DRD2) interaction on emotional eating in adolescence. Appetite. 2010; 54: 255-261. doi: 10.1016/j.appet.2009.11.006
87. Duran-Gonzalez J, Ortiz I, Gonzales E, Ruiz N, Ortiz M, Gonzalez A, et al. Association study of candidate gene polymorphisms and obesity in a young Mexican-american population from South Texas. Arch Med Research. 2011; 42: 523-531. doi: 10.1016/j.arcmed.2011.10.010
88. Roth CL, Hinney A, Schur EA, Elfers CT, Reinehr T. Association analyses for dopamine receptor gene polymorphisms and weight status in a longitudinal analysis in obese children before and after lifestyle intervention. BMC Pediatrics. 2013; 13: 197. doi: 10.1186/1471-2431-13-197