INTRODUCTION
Calciphylaxis is a rare disease occurring in usually obese women around the age of 40 years subject to hemodialysis. It can be prevented by controlling drug intake and biological markers. However, when installed it is irreversible and lethal. We report the case of a very young woman victim of non-observation with very deleterious consequence of calciphylaxis.
OBSERVATION
We report the case of a 26-year-old woman who was admitted to our hospital because of epistaxis and digital necrosis.
The patient was seen at our hospital 4 times since the age of 10. She had been diagnosed with Fanconi syndrome after a renal biopsy was done in 2001 for hypocalcemia, high PTH level and rachistism. Since then she had a hemodialysis 3 times a week. The patient reported many episodes of epistaxis, menorrhagia which were due to low platelets. Many investigations were done and a fibrotic medulla was diagnosed. Meanwhile, she received many platelet and red blood cells transfusions to recover from her severe anemia. Her last admission to this hospital was in February 2011 for severe hemorrhage after which she continued her medical treatment at a peripheral hospital.
Few months before her actual admission, the patient complained of a progressive dyspnea which was getting worse even on rest. She noted a loss of weight of 10 kg in 9 months and a loss of hearing with otorrhagia. She had as well digital necrosis with rapid progression and firm masses on both her right shoulder and right knee.
On presentation, the patient was very weak with inability to walk and active epistaxis. The distal parts of her 3rd and 4th fingers of her left hand as well as her 2nd, 3rd and 4th fingers of her right hand were necrotic and very painful (Figure 1). She had subcutaneous firm lesions with deformations of her upper limbs’ articulations (Figure 2). She had a silver corneal arch with yellow corneal deposits (Figure 1). On auscultation she had normal vesicular murmur and normal cardiac sounds. Her pulses were very weak on both her upper and lower limbs. She had an hepatomegaly and a splenomegaly.
Figure 1: Digital Necrosis on the Left and Silver Corneal Arch on the Right

Figure 2: Subcutaneous Calcified Lesions.

Her usual treatment was Moxonidine, Amlodipine, Ursodeoxycholic acid, Sevelamer, Alfacalcidol, Rabeprazole, Prednisolone, Erythropoetin, Naftidrofuryl, Sulodexide, Aspirine and weekly ferrous IV injections.
At first, we had to manage the epistaxis. The otolaryngology team described an anterior septal necrosis without evidence of telangiectasia and a chronic medial otitis which were the cause of the otorrhagia and epistaxis. A bilateral hemostatic packing with absorbable gelatin foam was done and the bleeding stopped 2 days later. The hypothesis of vasculitis was considered. A total body scan was done without evidence of pulmonary vasculitis or adenopathies. The immune assay was negative as well as the purified protein derivative (PPD) skin test (Table 1). A bone marrow biopsy was done to rule out any malignancy in cause of the low platelets; it came back positive for iron deposits and fibrinous changes.
| Table 1: Laboratory Results. |
|
Variable
|
Reference range, adults |
Jan-15 |
June 2016, before admission |
First admission |
Second admission
|
| Hematocrit (%) |
36-46
|
35.50 |
32.50 |
38.90 |
36.50
|
| Hemoglobin (g/dl) |
12.0-16.0
|
11.90 |
10.30 |
13.20 |
12.00
|
| White-cell count (per mm3) |
4500-11000
|
7000.00 |
8100.00 |
9400.00 |
6700.00
|
| Differential count (%) |
|
|
|
|
|
| Neutrophils |
40-70
|
68.00 |
77.00 |
79.00 |
75.00
|
| Lymphocytes |
22-44
|
19.00 |
16.00 |
15.00 |
17.00
|
| Monocytes |
4.0-11.0
|
12.00 |
6.00 |
5.00
|
|
| Eosinophils |
0-8
|
1.00 |
1.00 |
1.00
|
|
| Basophils |
0-3
|
0.00 |
0.00 |
0.00
|
|
| Platelet count (per mm3) |
150000-400000
|
33000.00 |
25000.00 |
40000.00 |
40000.00
|
| Mean corpuscular volume (um3) |
80-100
|
94 |
97 |
90
|
|
| Erythrocyte count (per mm3) |
4000000-5200000
|
3770000 |
3360000 |
4320000
|
|
| Erythrocyte sedimentation rate (mm/hr) |
0-20
|
|
|
|
|
| Sodium (mmol/liter) |
135-145
|
141 |
138 |
138 |
139
|
| Potassium (mmol/liter) |
3.4-4.8
|
3.61 |
3.62 |
3.5 |
3.6
|
| Chloride (mmol/liter) |
100-108
|
93 |
98 |
97
|
|
| Carbon dioxide (mmol/liter) |
23-31.9
|
27 |
18 |
19 |
16
|
| Glucose (mg/dl) |
70-110
|
|
|
113.5
|
|
| Albumin (g/dl) |
3.3-5.0
|
|
|
31
|
|
| Calcium (mg/dl) |
8.6-10.8
|
|
11.86 |
12 |
11.4
|
| Phosphore (mg/dl) |
2.5-4.5
|
|
5.8 |
5.9 |
5.4
|
| Urea nitrogen (mg/dl) |
8.0-25.0
|
46.4 |
46 |
67 |
30.5
|
| Creatinine (mg/dl) |
0.60-1.50
|
2.49 |
|
6.1 |
3.1
|
| Alkaline phosphatase (U/liter) |
30-100
|
|
246 |
329 |
489
|
| Aspartate aminotransferase (u/liter) |
9.0-32.0
|
26 |
|
31 |
41
|
| alanine aminotransferase (U/liter) |
7.0-30.0
|
34 |
20 |
35 |
48
|
| Lactate dehydrogenase (U/liter) |
110-210
|
|
|
|
|
| C-reactive protein (mg/liter) |
<8
|
73.6 |
|
22.6 |
103
|
| Ferritine (ng/ml) |
12-150
|
|
|
4720
|
|
| Transferrin (mg/dl) |
200-350
|
|
|
176 |
|
| Total serum iron (µg/dL) |
30-170
|
|
|
70.4
|
|
| Transferrin saturation (%) |
20-50
|
|
|
33.2
|
|
| Anti-thrombine III (%) |
|
|
|
95
|
|
| Lupus-like anticoagulant |
|
|
|
(-)
|
|
| Proteine C (%) |
70-130
|
|
|
120
|
|
|
Proteine S (%)
|
55-140 |
|
|
93
|
|
| Prothrombin time (sec) |
11.0-14.0
|
14 |
|
13.9
|
|
| aPTT (sec) |
20-40
|
26 |
|
32 |
|
| Anti-B2 glycoprotein |
|
|
|
(-)
|
|
| Ag HBs |
|
|
|
(-)
|
|
| ANA |
|
|
|
(-)
|
|
| C3 (mg/100ml) |
90-180
|
|
|
122
|
|
| C4 (mg/100ml) |
10.0-40.0
|
|
|
35.4
|
|
| DsDNA |
|
|
|
(-)
|
|
| Ac HBc |
|
|
|
(-)
|
|
| Ac HBs |
|
|
|
(-)
|
|
| Ac HCV |
|
|
|
(-)
|
|
| Ac HIV |
|
|
|
(-)
|
|
| p-ANCA |
|
|
|
(-)
|
|
| c-aNCA |
|
|
|
(-)
|
|
| TSH (mlU/l) |
0.5-5
|
|
|
4.6
|
|
| PTH (pg/ml) |
<46
|
|
|
514 |
333
|
| Vit D(25 OH) (ng/ml) |
5.0-75
|
|
|
5.3
|
|
Concerning the digital necrosis, we first did radiography of the hands which showed calcified vessels and calcified subcutaneous lesions (Figure 3).
Figure 3: Calcified Vessels, Calcified Lesions of the Left Index

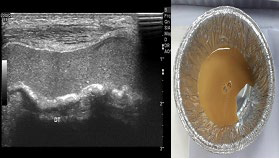
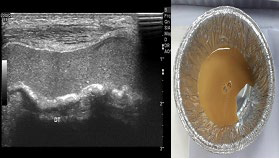
The arterial doppler of both the upper and the lower limbs showed an occlusion of the left radial artery, weak blood flow at the right cubital artery and bilateral distal arteriopathy in the lower limbs. She received daily doses of Prostavasine with small improvement and decrease of the pain. However, 2 days later she complained of pain again with progression of the digital lesions. The hypothesis of calciphylaxis was considered as we had ischemic lesions with arterial occlusion without signs of vasculitis and subcutaneous calcified lesions. Moreover an echography of her right knee was done and showed an intraarticular echogenic calcific sediment linked to another superficial sediment over the distal quadriceps. A fluid puncture was performed and got back sterile (Figure 4).
Figure 4: Knee Echography with the Liquid Removed.
Her lab results were accurate with a secondary hyperparathyroidism with a high phosphocalcic product (5,95 mmol2 / L2 ) (Table 1). The Alfacalcidol was stopped and the Cinacalcet started.
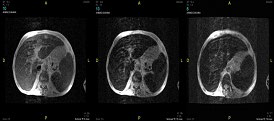
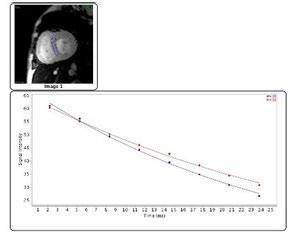
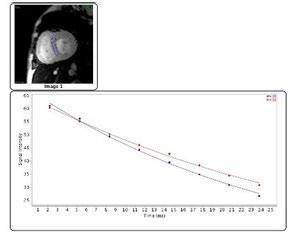
One week after her admission the patient was still unable to walk and was getting weaker. A cardiac ultrasound was then performed. A hypertrophic cardiomyopathy with suspicion of amyloid deposits and a severe diastolic dysfunction were found. An optimal cardiac treatment was impossible due to its side effects which involved more vasoconstriction. A salivary gland biopsy was performed to provide evidence for any amyloid deposits. It came back negative for amyloidosis but with signs of iron deposits. The hypothesis of secondary hemochromatosis was more evident as the results were out. We suggested a cardiac MRI and a hepatic MRI to rule it in; the cardiac MRI was negative for iron deposits but with some imaging limitations (Figure 6) while the hepatic MRI came back positive for iron sediments (Figure 5). We initiated the Deferasirox (Exjade) at that time.
Figure 5: Hepatic MRI T2*.
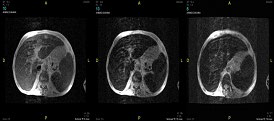
Figure 6: Cardiac MRI- The Mean T2* was 29.9±0.7 ms. It is Superior to the Reference Range of 20 ms set for Machines of 1.5 Tesla.
The patient left home with her new treatments and was denied any blood transfusion. She spent 2 weeks at home and came back with fever and severe weakness. On examination the digital necrosis were surrounded by areas of redness and purulent secretions. The subcutaneous nodules were less firm and some had decreased in size.
An amputation of her fingers previously suggested and rejected by her family was now the only choice. The culture was positive for E.Coli ESBL and E.Cloacae. Moreover her right knee was red, swollen and warm; another puncture was performed but the culture was sterile. She received 2 weeks of Ertapenem. During her hospital stay we decided to remove her parathyroid glands as the phosphocalcic product was still high even though she was taking the Cinacalcet. An incomplete parathyroidectomy was done because of anesthetic complications. The PTH level fell from 333 pg/ml to 121 pg/ml. Our patient left the hospital and came back one month later.
During this admission, the patient reported pain and severe weakness with insomnia and anorexia. She was given fluids and the parathyroidectomy was completed. She was in a severely depressive mood and decided to go back home as she was not getting any better. She died 2 hours after she reached her home.
DISCUSSION
Our patient presented unfortunately both calciphylaxis and secondary hemochromatosis.
In fact, calciphylaxis, also called calcific uraemic arteriolopathy, is a rare disease occurring mainly in hemodialysis patients. It is characterized by medial calcification of the small arteries and ischemia of the subcutaneous tissue, often leading to necrosis of subcutaneous fat and skin. It may not be as rare as it seems to be because we believe that the actual incidence is of 1% per year.1 Consequently the search for risk factors for calciphylaxis is crucial to prevent irreversible lesions. Among the risk factors described in the International Journal of Dermatology in 2007 (Table 2) our patient had too much which confirms the hypothesis of iatrogenicity.
| Table 2: Risk Factors for Calciphylaxis.9 |
|
Medications
|
Patient factors |
Biochemical
|
| Corticosteroids |
Renal failure |
Hypoalbuminemia |
| Vitamin D |
Female |
Hypercalcemia |
| Calcium salts |
Caucasian |
hyperphosphatemia |
| Immunosuppressants |
Local trauma |
High serum alkaline phosphatase |
| Iron salts |
Obesity |
High plasma parathyroid hormone |
| Insulin injections |
Diabetes mellitus |
High serum Ca2+×PO4 product |
| Calcium-based phosphate binders |
Malnutrition hypotension |
Protien C and S deficiency Vitamin D excess |
Moreover, this young patient had for many years ferrous injections plus transfusions which concluded to secondary hemochromatosis. One study in 1986 suggested the possibility of iron overload as a challenger for systemic calciphylaxis.2
Despite intensive combined therapies, the prognosis of both calciphylaxis and secondary hemochromatosis remains poor especially in the presence of necrotic lesions.
Many studies have emphasized the crucial role of a multidisciplinary therapeutic approach focusing on the correction of the underlying abnormalities of the calcium and phosphorus plasma concentrations in prevention for irreversible necrotic lesions. In fact, parathyroidectomy as well as the use of calcimimetics are actually the most recommended therapies for calciphylaxis. Parathyroidectomy must be done when parathyroid hormone (PTH) is higher than 500 pg/ml and when the Ca2+xPO4 product is refractory to drugs. However, in our patient it was of limited efficacy. Other therapies have been suggested including hyperbaric oxygen,3 intravenous sodium thiosulphat,4 steroids5 and bisphosphonates,6 but their efficacy is based on scant evidence. On the other hand, calcimimetics increase the sensitivity of the calcium-sensing receptor to calcium decreasing the parathyroid hormone as a consequence. One study reported a very good response to Cinacalect in a patient with calciphylaxis and contraindication for parathyroidectomy,7 which was not the case in our patient. This observation may be due to the advanced lesions in our patient associated with complete irreversibility.
Secondary hemochromatosis remains difficult to treat as the best treatment is phlebotomy which cannot be done to severe anemic patients who are usually subject to this condition. Iron chelators offer different means of achieving a negative iron balance and tolerable iron concentrations in body tissues. Deferasirox (Exjade) was probably the best choice for our patient because of its excretion in the biliary tract and its oral intake once daily. Moreover, a study published in 2015 reported a significant improvement of iron metabolism in hemodialysis patients with iron overload and an acceptable frequency of adverse effects.8 Our patient had a good tolerance but she was consistently weak and we did not look for biological improvement of the transferrin saturation. We believe that iron deposits were difficult to remove in the context of severe weakness and calciphylaxis.
CONCLUSION
Our case describes the deleterious effects that some of our practice as doctors can induce. Prevention medicine is not only about vaccinations but also about considering side effects of drugs. Calciphylaxis remains an important diagnosis to consider in patients with renal failure, with the aim of prevention and early therapy to reduce the associated morbidity and mortality. The astute physician should focus on the prevention and reduction of predisposing factors in cohorts at risk. Secondary hemochromatosis is an important side effect of multiple transfusions and ferrous injection. Physicians must limit unneeded therapies.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.