INTRODUCTION
Intolerance to foods has been known since ancient times, although it was regarded as minor health problem.1 Concerns about food allergies emerged and escalated in the last few decades as a result of life-threatening anaphylactic reactions produced by food allergens. For instance, the prevalence of food allergy in US children has increased by 20% over the last decade, and similar trends have been reported in other countries.2 According to statistics from the World Allergy Organization (WAO)3 and allergy associations, 8% of children and 3% of adults are affected by food allergies and intolerance. Allergists alert that this rate might be in fact much higher.4 According to Asthma and Allergy Foundation of America (AAFA),5 allergy is the 5th leading chronic disease in US among all ages, and the third most common chronic disease among children under 18 years old. As a chronic disease, it starts from infancy and often lasts for a lifetime.6 Although, many people outgrow their allergy, it drastically changes the quality of life of the patient and his/her family, and generates different costs, including social and psychological ones. Thus, since the 1990s, food allergy is considered a major public health issue.7
Almost all sources state that the most effective management food intolerance, including allergy, is elimination or avoidance of harmful ingredients.8 According to the American Food Allergy & Anaphylaxis Network (FAAN), no medication could prevent food allergies.9 Medications can be applied to merely control symptoms, which can range from mild (rashes, hives, itching, swelling, etc.) to severe (dyspnea, wheezing, loss of consciousness, etc.). Besides, despite numerous research projects devoted to food allergy, carried out in multinational consortia (e.g. INFORMALL, EUROPREVALL), knowledge on mechanisms of food allergy and intolerance is still incomplete, especially with regard to haptens (small compounds typically of simple chemical structure) that are present in all foodstuffs either as natural components, contaminants, or additives given purposefully during food processing.
As it was pointed out by Nolan (2004) early diagnoses with timely and individualized management are key elements to fight the rapidly growing rate of allergy and may prevent complications and progression to a chronic disease.4
The goal of the present paper is to review existing knowledge on current food allergy management strategies and to suggest an outline for integrated management framework of food allergy and intolerance. It will consist of Standard Operating Procedure addressed to health professionals, food production sector and educators, and Dietary Behaviour Principles addressed to different groups of consumers, e.g. breastfeeding mothers. We would like to emphasize the importance to base the management strategies on evidence-based and up-to-date knowledge on food allergies, and we will indicate the areas which still need much more scientific evidence.
STATE-OF-THE-ART IN FOOD ALLERGY – KNOWLEDGE GAPS AND AREAS FOR FURTHER RESEARCH
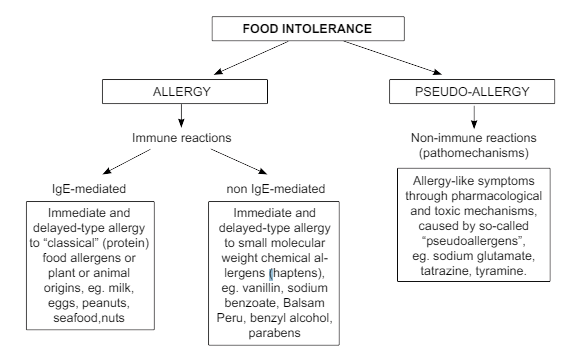
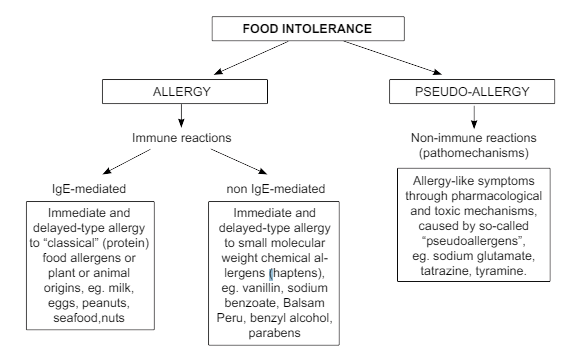
At the beginning, it is necessary to distinguish between food intolerance and allergy. Food intolerance can be divided as allergy and pseudo-allergy (Figure 1). The term “food allergy” is used when an immunological mechanism has been defined or is suspected in case of food intolerance. Immune reactions to food are traditionally divided into IgE-mediated and non-IgE-mediated. IgE-mediated (type I or immediate) allergic reactions are to “classical” protein allergens (e.g. milk or egg proteins) while non-IgE-mediated may be due to the cell-mediated, delayed (type IV) allergic reactions to small molecular weight compounds (haptens) of synthetic or natural origin. Both allergy types are known causes of eczema, referred to as atopic eczema and allergic contact dermatitis, respectively. Another diseases caused by delayed type-allergy to haptens include allergic contact stomatitis,10 allergic contact conjunctivitis,11 allergic vaginitis.12 Relapses of allergic contact dermatitis caused by oral ingestion of haptens are referred to as systemic reactivation of allergic contact dermatitis – an entity that shares clinical characteristics with atopic eczema (chronic or recurrent course, flexural predilection of eczema, etc.) and is very difficult to tell apart from the latter.13 Furthermore, delayed type allergy was proposed as explanation for some cases of urticaria,14 asthma,15 and allergic rhinitis.16
Figure 1: Food allergy within the spectrum of food intolerance. Source: Own research.
“Classical” protein allergens, like eggs, milk, peanuts, legumes, etc. have been intensively studied with respect of food allergy and eczema. Nevertheless, only 10-50% of the cases could be explained by actual allergy to these compounds. Thus, focusing exclusively on these food allergens has proven insufficient in controlling the whole spectrum of food allergy and to be effective in management strategies. The role of delayed-type allergy to food haptens has not been yet systematically studied, however convincing scientific evidence supports assumption that they may explain cases that cannot be explained by the IgE-mediated allergy to food proteins. Therefore, next to paying due attention to “classical” food allergens (proteins), the research is needed on the food haptens, which have not yet been studied systematically in relation to food allergy. Recent clinical and experimental evidence seem to support the existence of relationship between food haptens and delayed type food allergy.17 This group of food chemicals typically causes symptoms that may appear from one to several days after the ingestion. Artificial food agents are present in a vast majority of contemporary food products. However, current risk management strategies offer no respective recommendations to food industry, health professionals and policy makers, who only know how to manage classical food allergens. Haptens may be present in food both as natural components (e.g. nickel, cobalt, vanillin) or contaminants (pesticides, animal drugs, industrial chemicals) and those purposefully added during food processing (preservatives, emulsifiers, colorants flavour enhancers, antioxidants). Finally most of oral drugs are also haptens,18 contrast to allergens, haptens are too small to be recognized by the immune system via antibodies or lymphocyte receptors, however; they form strong chemical bonds with endogenous proteins distorting their spatial conformation to such extent that these are no longer tolerated and induce immune reactions.
A number of recent reports (European Academy of Allergy and Clinical Immunology – EAACI and GA2LEN, several scientists confirmed that although patients suffering from food allergy and/or intolerance often associate relapses of their disease with ingestion of particular foods, only minority of these cases is caused by “classical” protein allergens (e.g. milk, eggs or peanuts).19,20,21,22 In majority of adolescents and adults allergies to “classical” food allergens, such as hen’s eggs and cow’s milk are considerably less common and play a marginal role. As a result, “elimination diets” aimed at curing food allergy or intolerance by excluding various “allergenic food” remain ineffective in most cases and too often cause unjustified dietary regimens.23,24 Better insight into the role of food haptens as a possible cause of dermatitis and food allergy was listed among relevant future research priorities by experts of the European Academy of Allergy and Clinical Immunology.25
Large and medium-scale international research projects funded within the EU Framework Programs (eg. ALLERGEST, BIOAIR, EUROPREVALL, FAREDAT, GA2LEN, FORALLVENT, INFABIO, INFORMALL, PARSIFAL, PDCAAE, PROTAL) addressed various aspects of food allergies diagnostics, tests, cost, assessment, thresholds, prevention related to various elements of life (chronic respiratory conditions in children related to traffic air pollution, effect of gastrointestinal digestion on the allergenicity of foods, clinical course and biomarkers in severe chronic airway disease, effect of diet and lifestyle on risk of gastrointestinal infection and allergy in early life, determinants of childhood asthma and allergies across Europe etc.). Regardless the huge contribution and benefits from these studies to the present knowledge and management strategies, problems of high numbers of patients with food allergy still remain unsolved and current policies seem not capable of offering them sufficient support/help in the context of effective health policies.
CURRENT ISSUES IN ALLERGY MANAGEMENT STRATEGIES
There are four approaches to management of food allergy: avoidance, education, pharmacotherapy and immunotherapy. Total avoidance of an allergen, and being prepared with appropriate treatment of acute allergic reaction, are the main principles of successful food allergy management. Programs of dietary allergen avoidance have shown a positive effect in preventing or delaying the atopic disease, yet their effect is mostly limited to infants at high risk of developing allergy. Dietary prevention of allergy in infants and small children was studied by i.a. Muraro et al and Sicherer et al.26,27,28,29 The results show i.e. that in case of high-risk children, breastfeeding combined with avoidance of solid food and cow’s milk for at least 4-6 months is the most effective preventive food regimen. On the other hand, in elder children elimination diets should be introduced with caution, due to the risk of malnutrition. Thus, patients, their families and healthcare workers need guidelines and suggestions for avoiding allergenic foods in meal planning, preparation and selection of nutritionally adequate replacement food.30 Parents’ knowledge is also insufficient. It has been shown that only one eight of the infants whose parents reported adverse food reactions were found to have an actual allergy or intolerance, which implies a need to raise awareness of the need for accurate diagnosis to prevent children being on unnecessarily restricted diets.31
Moreover, certain foods are difficult to avoid due to e.g. hidden ingredients, and there are social risks of dietary avoidance,32 and psychological distress,33 which also should be addressed in management. Young et al34 pointed out that numerous studies, examining food allergy and anaphylaxis care in schools and childcare settings, have identified two main deficiencies, such as inadequate food allergy management plans and deficiencies in recognizing reactions and treating reactions with epinephrine. There is also much to be done to improve current food allergy and intolerance management practices in healthcare sector. For example, most allergies are managed within primary care, yet it has been proven that very few GP’s and practice nurses get any formal training in allergy.35 There are also concerns that diagnosis and management of food allergies vary from one clinical practice to another.36 Besides, little or no emphasis has been given on the distinction between “food allergy” and “food intolerance” and consequently, there are no allergy/intolerance specific risk management strategies.
One of the latest book about food allergy comprised information about pharmacotherapy and educational programmes. Authors stated that currently it is no well-established-modifying treatment for food allergy and that the best method is avoidance of allergen(s). In case of acute food-induced allergic reactions exist recommendations for the pharmacological management.37 Educational programmes in food allergy are not so often presented by scientists, perhaps because it is need of knowledge about foods as well as about nutrition. Technological processes during food products preparation often change allergenic properties. Educational programmes should comprised knowledge of disease, food properties, food technology, interactions between food and drugs used in allergy therapies, as well as psychology, how to change nutritional behaviour of patient.38,39
The two position papers have been published on allergen immunotherapy in Journal of Allergy and Clinical Immunology in 2015 and 2016. They present actual international consensus on procedures inducing tolerance to specific allergens through repetitive administration of them, e.g. food allergens. The key message is that “…For food allergy, EAACI (European Academy of Allergy and Clinical Immunology) systematic review of the literature highlighted a large heterogeneity in the protocols used by different research groups in terms of preparation of food allergens, updosing, maintenance dose, and OFC (Oral Food Challenge – a highly diagnostic provocation test used for the diagnosis of food allergy) procedure; therefore there is no single established protocol that has been shown to be both effective and safe in large multicentre studies. Currently, there is agreement that although immunotherapy to foods is an important area of research, it is not yet ready for clinical practice….”.40,41
SUGGESTIONS FOR INTEGRATED MANAGEMENT OF FOOD ALLERGIES
There is a need to develop an innovative approach for evidence-based risk assessment and management in the field of food allergy, taking into account both “classical” (protein) allergens and small-molecular haptens occurring in food naturally, contaminants and food additives, from the farm through the food industry to the end consumer and further to the society (“from farm to fork”). This approach should take form of sets of documents addressing evidence-based solutions for the existing problems of food allergy management – available both in electronic and printed form as Standard Operating Procedures (SOPs) and Dietary Behaviour Principles (DBPs).
Standard Operating Procedures (SOPs)
Standard Operating Procedures with relevant recommendations should be developed and distributed among three main groups (sectors) of the relevant stakeholders: healthcare sector, food industry sector, and educational sector. The basic scope of each SOP should contain the following:
– Scope and applicability (purpose, limitations),
– Summary of methods and description of target groups,
– Definitions,
– Health and safety warnings,
– Cautions and mitigation plan,
– Interferences with final product,
– Personnel qualifications and responsibilities,
– Equipment and supplies,
– Procedures identifying all pertinent steps needed to accomplish the procedures, including checklists,
– Data and records management (i.e. calculations, forms to be used, reports to be written, data and record storage information, personal data protection),
– Specific recommendations, complementary to Procedures or referring to issues that are not covered by the Procedures,
– Guidelines for implementation – additional information on how to implement procedures and recommendations, taking into account regulatory issues,
– Quality assurance (control) – specifications for self-verification of the quality and consistency of work, with the inclusion of specific criteria for each stakeholder group,
– References – other external documents and procedures that interfere with the SOP and recommendations (attached any document, including those which are not readily available).
The SOPs and relevant recommendations should be specific for each group of professionals, and include accordingly:
Health sector
Recommendations for medical doctors (allergists, general practitioners, gynecologists, pediatricians), including new methods of diagnosis of food allergy, updated list of allergens, and complementary practices in cooperation with other health professionals, in order to provide a complex care over allergic patients,
– SOPs for biochemical laboratories in hospitals, assuring Good Laboratory Practice (GLP) with biological samples from allergic patients, taking into account specific conditions of food allergy,
– SOPs and recommendations for dieticians and pharmacists regarding cooperation with medical doctors and providing advice in food and drug preparation and intake,
– SOPs and recommendations for nurses and midwives regarding cooperation with medical doctors and Good Communication Practice with allergic patients,
– SOPs for sanitary authorities regarding controls in hospitals, clinics, and other institutions.
Food industry
– SOPs and recommendations for agri-food producers, containing Good Agricultural Practices (GAP) to reduce risk of unintentional contamination of food with potentially allergenic agents,
– SOPs and recommendations for food technologists, including Good Manufacture Practices (GMP) i.e. to use allergy-friendly food ingredients, and to avoid cross-contamination which may occur during processing. It will contribute to make allergy declaration for new updated labelling and consumer information by providing an updated list of sensitizing food agents, which can be “classical” protein allergens and non-proteinaceous, small molecular weight sensitizers (haptens),
– SOPs for sanitary authorities regarding the control whether food production and processing practices at different stages of the food chain fulfil allergy-safety requirements, to provide an allergy-friendly food to the consumer.
Educational sector
– SOPs for kitchen staff at kindergartens, schools, etc., for allergy-safe meal preparation and distribution to children and adolescents,
– Recommendations for teachers regarding proper attitude to allergic child, providing healthy lifestyle education and communication with children and their parents,
– Recommendations for school medical staff (doctors/nurse/hygienist) as regards preparation of school/childcare setting environment to be friendly for children with food allergies, as well as providing relevant care for such children during school hours, in cooperation with kitchen staff, teachers and parents.
Dietary Behaviour Principles (DBPs)
The objective of the evidence-based Dietary Behaviour Principles (DBPs) is to help allergic consumers and their families to understand their current dietary practices and how these practices influence the risk of food allergy, as well as to encourage them to develop eating habits that will prevent unnecessary exposure to food allergens/haptens and at the same time, to avoid malnutrition. It should be achieved by providing relatively simple decision making rules to be used in making aware food choices. DBPs should be formulated with respect to relevant consumer groups (with special version for children), each should consist of the following sections:
– Description of target group,
– Explanation of food allergies – short information about various types and effects of food allergy and intolerance, and where to seek for relevant information,
– Objectives of dietary changes – clearly defined and stated objectives of shaping specific dietary patterns which help avoiding unnecessary exposure to food allergens/haptens,
– Barriers to dietary behaviour change – a list of socio-cultural, economic, ethical and other barriers to dietary behaviour changes; each group of consumers will be provided with pertinent explanation of such obstacles, and will be encouraged and motivated to overcome these barriers,
– General information about commercially available allergenic food products most frequently consumed in Europe,
– Demonstrating proper dietary behaviours relevant for different types of food allergy and source of protein allergen/hapten, such as meal preparation at home, buying behaviours regarding the selection of low vs. highly processed foods, avoiding certain allergens, reading labels.
As in case of SOPs, DBPs should be addressed to different consumer groups, specifically:
– DBPs for pregnant and breastfeeding mothers to inform about the use of allergy-friendly food and culinary practices in home meal preparation to prevent from or to minimize the risk of food allergy, as well as best practices to be followed in breastfeeding,
– DBPs for parents and caregivers of infants who are not breastfed (weaning period) and of very young children not capable of self-managing their allergy/intolerance. It should provide advice on allergy-friendly infant formulas and how to prepare meals for children with various types of food allergy, in order to prevent the risk of allergic reactions and at the same time, to avoid malnutrition,
– DBPs for children at the age of kindergartens and schools, who take first steps in self-management of allergy, to educate them to be responsible for their eating behaviours outside home,
– DBPs for adolescents with already shaped attitudes and dietary behaviour patterns, being exposed to strong peer pressures; it should inform them how to select allergy-friendly foods,
– DBPs for adults, to provide people with information about food nutritional value and allergen content in raw food products and processed foods; it should allow them making aware choices of food and learn proper meal preparation practices at home, in accordance with their preferences, age and health condition.
The integrated framework of allergy management – which SOPs and DBPs are part of – should take into account cross-country differences in the prevalence of food allergy and intolerance. For example, in case of peanut allergy it has been observed that societies in which peanuts are consumed fried or boiled (i.e. China) have lower peanut allergy prevalence compared with the societies where roasted peanuts are more popular (i.e. US).42 The above SOPs and DBPs should be prepared in cooperation with various professionals and representatives of the consumer and allergy associations, and distributed following approval of the relevant regulators.
CONCLUSIONS
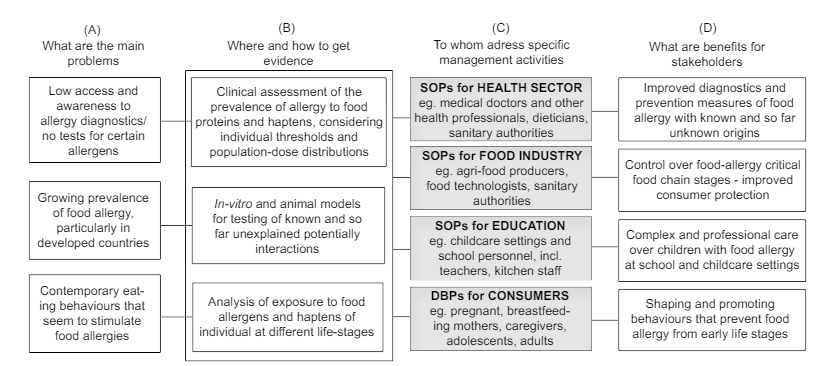
The above considerations have been summarized in Figure 2. It shows that the integrated approach to management of food allergies should respond to three major problems identified: 1) low access to allergy diagnostics combined with the fact that there are no tests for all the allergens, 2) growing rate of food allergy, particularly in developed countries where the consumption of processed foods is very high and still increasing, 3) contemporary eating behaviours that seem to stimulate food allergies (column A).
Figure 2: Integrated approach to management of food allergy – SOPs and DBPs. Source: Own research.
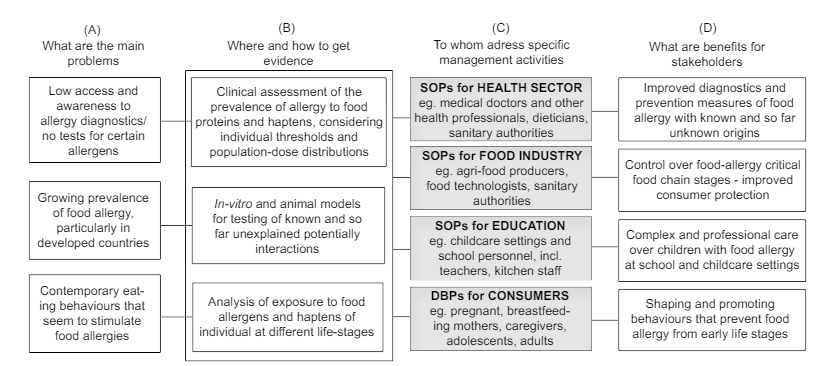
We acknowledge the fact that more research is needed to gain the complete knowledge on food allergy (Column B). Particularly, it requires clinical assessment of the prevalence of allergy to haptens, on which present evidence is insufficient. Other research activities should be based on in vitro and animal models for testing known and so far unexplained, potentially allergenic interactions. More research is also needed to analyse the exposure to food allergens (and haptens) of individuals at different life stages. The integrated and systematic approach to management of allergy (Column C) consists of Standard Operating Procedures (SOPs) and recommendations addressed to three groups of professionals: 1) health sector, 2) food industry sector, 3) educational sector, and Dietary Behaviour Principles (DBPs) for different groups of consumers. They reflect benefits for different groups of stakeholders (Column D). It is also important to involve relevant regulators and actors such as media and consumer/allergy associations, who would implement and communicate the SOPs and DBPs.
CONFLICTS OF INTEREST: None.