INTRODUCTION
The Coronavirus disease 2019 (COVID-19) pandemic, also known as the coronavirus pandemic, is an ongoing global pandemic of COVID-19, caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2).1
There is no longer any need to prove that COVID-19 is a respiratory disease with pulmonary manifestation. However, a rising number of evidence support that COVID-19 related coagulopathy and has reached other systems. Although efforts to recognize and manage SARS-CoV-2 infections have focused primarily on respiratory complications, some patients with COVID-19 infection may experience gastrointestinal manifestation from this disease.2,3,4
A recent study reports the involvement of mesenteric ischemia in some patients with COVID-19 and gastrointestinal symptoms.5 To our knowledge, only six cases have of mesenteric ischemia associated with COVID-19 have been reported.6,7,8,9,10,11 The present report describes 3 cases of mesenteric ischemia events in previous symptomatic individuals with confirmed severe COVID-19.
CASES
Case 1
We report the case of a 66-years-old woman Ms. B, who was referred to our institution for asthenia, anorexia, cough, dyspnoea associated with fever which she had experienced for the preceding 2-days, but no pre-existing symptoms of gastrointestinal disease. Her viral polymerized chain reaction (PCR) test for SARS-CoV-2 returned positive 4 days ago and her husband and child were recently diagnosed positively at COVID-19. Clinical examination revealed crackling sound on the lungs, electrocardiogram was normal. On arrival, her oxygen saturations were 91% on room air. Laboratory studies demonstrated an increased C-reactive protein (61 mg/L), Fibrinogen (4.74 g/L), Procalcitonin (0.11 ug/L) and a mild thrombocytopenia (117×109 /L). D-dimer levels, brain natriuretic peptide (BNP), troponin I, renal function and liver function were normal.
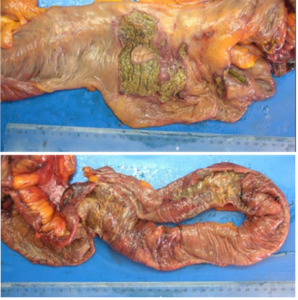
On day 1, she was transferred to the intensive care unit (ICU) for worsening hypoxic respiratory failure and was intubated. On hospital day 30, the patient was still in the intensive care unit, under intubation and 2 mg/hours of noradrenaline, in front of septic shock associated to a pronounced abdominal distension with a melena, an abdominal computerized tomography (CT) was made. Transversal CT scan image showed bowel dilatation and slices showed an hypodensity and an enhancement of the wall of part of the small bowel, with a permeable coeliac trunk, mesenteric superior and inferior vein (Figure 1).
Figure 1. CT Scan Showing Hypodensity and Un-enhancement of the Wall of Part of the Small Bowel (black narrow

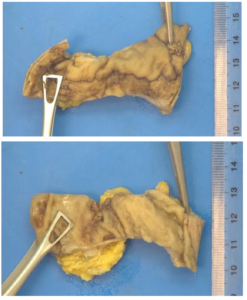
An immediate surgical exploration was done by laparotomy, in peri-operative it was observed at the distal ileum ischemic, non-necrotic lesion with a patchy distribution (Figure 2). A multidisciplinary decision was made with the intensive care unit team to practice the resection of 100 cm of bowel. The pathologist analysis concluded to ulcerative colitis lesion associated with ischemic bowels lesion, limited to the mucosa, the vessels of the below mucosa showed an aspect of vasculitis, with no evidence of thrombotic events.
Figure 2. Macroscopic Appearances of the Surgical Specimen of Bowel Resection
Case 2
The second one, Mr. B 60-years-old men who consult the ER for dyspnoea, tachypnoea associated with fever (39.6 °C). The patient was schizophrenic, actually stable with Haloperidol therapy. The clinical examination found a seesaw breathing, crackling sound on the lungs no pre-existing symptoms of gastrointestinal disease, the polymerase chain reaction (PCR) COVID-19 test was positive. On arrival, his oxygen saturations were 95% on room air. Laboratory studies demonstrated an increased C-reactive protein (91 mg/L), lymphopenia (0.72×109 /L), D-Dimer (1819 ng/mL), Glomerular filtration rate (59.8 mL/min/1,73 m2) a hepatic cytolysis with liver transaminases alanine aminotransferase (ALT) (228 U/L), aspartate aminotransferase (AST) (115 U/L), N-terminal pro-b-type natriuretic peptide (NT-proBNP) (470 ng/L) troponin I (0.957 ug/L).
The patient was admitted in conventional COVID-19 unit, with empiric antibiotic therapy. On the day 1 in the hospital, the patient was tachypnoeic, a 68 mmHg of PaO2 on 12 L/min O2 under a high concentration mask, the patient was transferred to the ICU for worsening hypoxic respiratory failure, intubated and sedated.
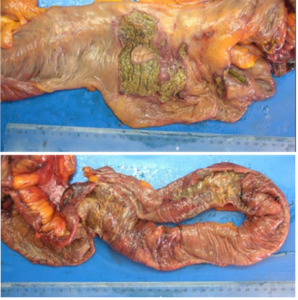
On hospitalization day 27, the patient presented a severe sepsis with hyperlactatemia (1.8 mmol/L) on Noradrenalin 1 mg/h associated to an abdominal distension, CT scan showing no dilatation, but a slice of peritoneal fluid with compartmentalization in the pouch of Douglas with a permeability of the abdominal vessels and no pneumoperitoneum. A surgical exploration was made, it was found an abundant purulent discharge on the peritoneal cavity, and a perforation of the bowels at 3.70 m of the duodenal-jejunal angle and at 1 meter of the ileo-caecal junction associated with false membrane and inflammatory large momentum next to the perforation. The resection of the perforated bowel was practiced and a double ileo-stormy was made, the analysis of the peritoneal discharge sample concluded about the presence of coagulase negative staphylococci (CoNS), analysis of the surgical specimen (Figure 3) revealed the presence of a bowel wall inflammation and ulcerous area. On post-operative day 3, the patient was in septic shock with acute fever, an increased C-reactive protein (166 mg/L) and a rising Lactatemia (7.9 mmol/L). He received 11 mg/hours of Noradrenaline, the CT scan was non-contributory and explorative surgery was made, bowels with macroscopic normal aspect were observed, no sign of inflammatory lesion was found in peri-operative. However, a layer of intraperitoneal effusion could be seen and has been taken in the Douglas pouch.
Figure 3. Macroscopic Appearance of the Surgical Specimen of Bowel Resection

Case 3
The third Mr. A 63-years-old man patient, dyspnoeic for 3-days, without fever. On arrival, his oxygen saturations were 45% on room air, 55% after 5 L of O2 (lunettes). The clinical examination found a seesaw breathing, crackling sound on the lungs, no pre-existing symptoms of gastrointestinal disease, and the PCR COVID-19 test was positive. Laboratory studies demonstrated an increased C-reactive protein (114 mg/L), lymphopenia (0.58×109 /L), D-Dimer (1296 ng/mL) NT-proBNP (295 ng/L), lactate (1 mmol/L) troponin I level, renal function and liver function was normal.
The patient was intubated and admitted in ICU on day 1, and on day 4 in front of a septic patient with an abdominal distention, an abdominal CT scan showed a distension of sigmoid colon with an infiltration of fat, (Figure 4) a clear mesenteric vessel was noted, and an important gastric dissension was described too. At day 7 (24th of May), a sigmoidoscopy was practiced and showed at 30 cm of the anal margin on 5 centimetre a large and deep ulcer with erythematosus aspect, the biopsy result of this lesion concluded to colitis ulcers necrosis looking like ischemia lesion.
Figure 4. CT Scan Showing a Distension of Sigmoid Colon with an Infiltration of Fat (black narrow)

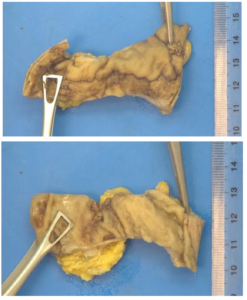
Therefore, on day 9 of hospitalization, a surgical exploration was made by laparotomy, an abundant serous discharge was observed on the peritoneal cavity, no ischemia lesion was observed in the colon, and his macroscopic aspect look healthy, however, in front of the sigmoidoscopic result a left colectomy was made with a terminal left colostomy. The pathologist observation (Figure 5) of the surgical specimen of colectomy showed an ulcerative area on 2 cm with inflammatory aspect, it was observed a hyalin aspect with endothelial inflammation on the small mesenteric vessel around. The aftermath of surgery was therefore simple: the patient was extubated on day 2 from surgery, getting back slowly to eat and noradrenaline was progressively stopped. On postoperative day 4 (30th of May), the patient described an acute abdominal pain and an abdominal tenderness was clinically found, the patient was intubated for worsening hypoxic respiratory failure extracorporeal membrane oxygenation (ECMO) laboratory studies show a decreasing hemoglobinemia 7.1 g/dL, a rising hyperlactatemia (9 mmol/L) the patient was under 9 mg/hours of Noradrenaline and a surgical exploration was made, an important hemoperitoneum was observed and evacuated essentially localized next to the colectomy area, the peritoneal cavity was explored and no more lesion was observed with a normal macroscopic bowel aspect, haemostasis was made, the abdominal cavity was washed and drained, and the hypothesis of a lesion of the sigmoid artery during the first intervention was made in front of the macroscopic aspect found in this area.
Figure 5. Macroscopic Appearance of the Surgical Specimen of Colectomy
DISCUSSION
With the cases of our patients, no evidence available has conclusively demonstrated thrombotic or embolic events in large gastrointestinal vessels eg., veinous or arterial mesenteric vessels by radiologic or pathologist analysis. Nevertheless, pathologist has showed necrotic, colitis, inflammatory aspect of bowel with endothelial inflammatory of the small vessels.
The exact mechanism and pathway of gastrointestinal lesion in severe COVID-19 patients are not known yet, Arshad Hussain Parry et al12 has exposed four possible mechanisms, in isolation or in varying combinations who could account for this complication in severe COVID-19. First coagulation disorder induced by systemic inflammation state (hypercoagulability), endothelial activation, hypoxia and immobilization may lead to mesenteric vascular thrombosis Preliminary pathological evidence has shown bowel necrosis with small vessel thrombosis involving the submucosal arterioles, thereby pointing to an in-situ thrombosis of small mesenteric vessels rather than an embolic event.
Moreover, elevated levels of von Willebrand Factor have been reported in severe COVID-19. von Willebrand Factor is released from Weibel-Palade bodies in response to endothelial damage. Vascular endothelium expresses angiotensin converting enzyme 2, the target receptor for SARS-CoV-2, which can possibly explain the endothelial cell tropism of SARS-CoV-2 and subsequent endothelial dysfunction or damage with resultant vascular thrombosis.
In addition, expression of angiotensin converting enzyme 2 on enterocytes of small bowel, the target receptor for SAR-Cov-2, may result in intestinal tropism and direct bowel damage. Finally, shock or hemodynamic compromise which is commonly associated with severe COVID-19 pneumonia may lead to a non-occlusive mesenteric ischemia.
All our patient were sedated, intubated, in shock with catecholamines and the lesion observed associated to gastrointestinal symptomatology could be ischemic lesion causes by low flow, more than that we know that patient in care unit (ICU) with ischemic colitis are often under-diagnosed, since the parallel co-morbidities and the nonspecific nature of symptoms that mimic almost any abdominal pathology, can mislead the doctor. Moreover, sedated, or ventilated patients can mask many of the characteristic features of ischemic colitis and make the diagnosis challenging.13
CONCLUSION
In conclusion, patients infected with SARS-CoV-2 may show atypical presentations, such as gastrointestinal symptoms, precise knowledge of the mechanism of bowel lesion in COVID-19 patients is essential. Treating clinicians must be aware of the hypercoagulable state of COVID-19 patients and judicious use of prophylactic anticoagulation in hospitalized patients should be considered in regard to intensity of thromboprophylaxis to reduce the morbidity and mortality associated with this disorder.
INSTITUTIONAL BOARD PERMISSION
The study is approved by the institutional review board.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.