CASE REPORTS
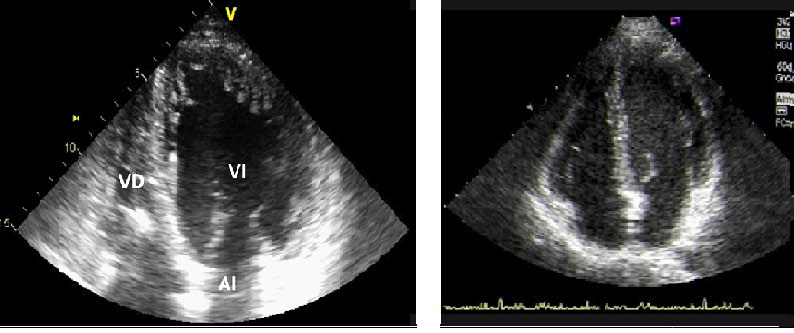
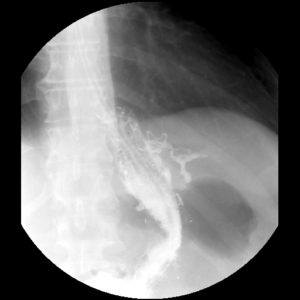
Case 1: A 54-year-old male with Sleep Apnea Syndrome (SAS), Diabetes Mellitus (DM) type 2, hypertension, Morbid Obesity (MO) and Dilated cardiomyopathy (DCM) was referred to our hospital for bariatric surgery. In addition, the preoperative cardiac ultrasound showed a Ventricular Ejection Fraction (VEF) of 24%. He had a Body Mass Index (BMI) of 41 kg/m2 and underwent an uneventful Sleeve Gastrectomy (SG). Three years after the surgical procedure, the patient co-morbidities and quality of life have improved, and the cardiac ultrasound confirmed an increase of his VEF from 24% to 36% (Figure 1A-1B).
Figure 1A: Preoperative cardiac ultrasound in case 1 showing a dilated left ventricle. 1B: The cardiac ultrasound, 12 months later, revealed a decreased in left ventricular dilatation and a ventricular ejection fraction improvement.
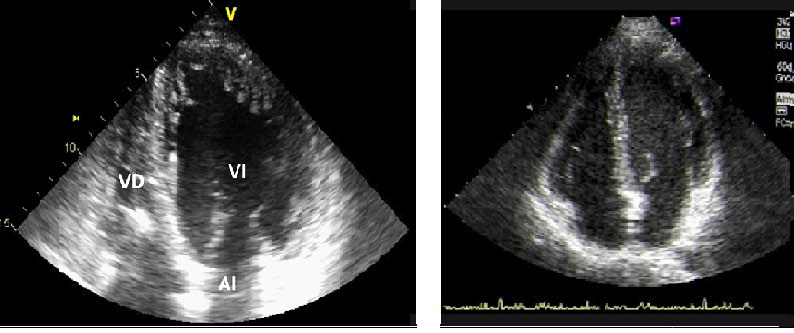
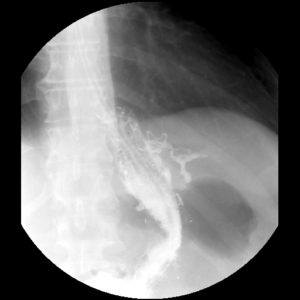
Case 2: A 46-year-old male with DM type 2, hepatitis B, hypertension, MO and DCM, was operated on with a VEF of 27%. On physical examination, a BMI of 37 kg/m2 was the most relevant finding. During the SG, the last cartridge of the stapler failed and the patient developed a leak near the esophagogastric junction, albeit a prompt reoperation was done during the first 48 hours. All the subsequent therapeutic approaches with stents, glues or metallic clips were unsuccessful (Figure 2) and finally, a total gastrectomy was performed, with an excellent recovery. 18 months after the first bariatric procedure, the patient showed an improvement of 10% in his VEF as well as in his co-morbidities.
Figure 2: Barium swallow of case 2 patient after failure to control the gastric leak (V) by a metallic clip (arrow).
In both cases, the BMI was under 28 kg/m2 after the first year of the bariatric operation.
DISCUSSION
Obesity causes anatomical and functional heart impairment, which can be ameliorated with weight loss surgery, as an increase in cardiac output, preload and post-load.1,2,3 In patients with DCM, these hemodynamic changes produce impairment in the systolic left ventricular function and a larger heart dilatation. In the recent literature there is some evidence about the positive impact of BS on specific cases of heart disease as DCM.3,4,5,6 Furthermore, some patients with DCM who are in an end-stage heart failure have been denied cardiac transplantation due to MO. Nevertheless, it has been shown that the cardiac function improvement after different bariatric procedures can avoid the necessity of an ulterior cardiac transplantation.4,5,6
On the other hand, those patients usually have other comorbidities linked to the metabolic syndrome (SAS, DM, hypertension) that improve after weight loss.
Which bariatric technique is the best for such patients?
This is a difficult question but the simplest is the best in this scenario. For this reason, we preferred sleeve gastrectomy instead of gastric bypass. However, we had a dreadful complication in our second case due to a technical problem but, at the end, the gastric leak was solved and the patient was able to experiment the benefits of a significant loss of his weight.
If we focus on functional heart changes, VEF increase is perhaps one of the most relevant indicators, and it has been highlighted in other cases.4,6 Nowadays, is appropriate to confirm the durability of this benefit and how is the long-term heart behaviour of these patients with larger prospective studies.
In summary, BS offers an important improvement in obese patients with DCM. Thus, it should be consider when other weight loss approaches were unsuccessful because bariatric operations are quite safe and effective at the present time.