INTRODUCTION
About 100-years have passed since the first experiments led by the pathophysiologist Paulesco who corrected hyperglycemia by injecting pancreatic juice into the diabetic dog.1 In December 1922, after visiting Toronto, the Danish physiologist August Krogh with his diabetic wife Marie, a physiologist herself, extracted insulin from 2 kg of fresh bovine pancreas at a time in the cellar of his home in Hellerup (Copenhagen, Denmark), with the help of Hans Christian Hagedorn and the pharmacist Norman B Jensen. In May 1923, Hagedorn founded the Nordisk Insulin Laboratorium with August Kongsted, owner of the Löve (Leo) pharmacy and the pharmaceutical industry of the same name, and immediately produced sufficient amounts of insulin to successfully treat the first eight patients with diabetes admitted to the Kommunehospital in Copenhagen.2,3
Meanwhile, in January 1923, Eli Lilly had already produced 100,000 Units of insulin (“Iletin”) per week, and in May 1923, in England, Burroughs Wellcome and the Boots Pure Drug Company were marketing insulin (20 U per ml in 5 ml vials) for £ 1.25.4
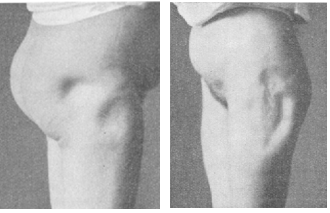
In the same years, lipodystrophies, i.e., complications at the injection site, immediately occurred (Figure 1).5-14 Until the advent of human insulins in 1982 and the first fast-acting analog in 1999, lipoatrophic (LA) lesions were widespread (Figure 2).
Figure 1. One of the First Cases of Lipoatrophy at Insulin Injection Sites5
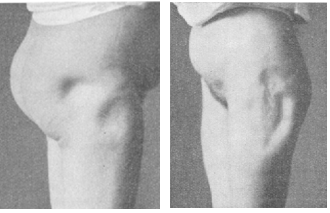
Figure 2. Lipoatrophy in the Vicinity of the Navel of a Patient Who Injected NPH Insulin (Personal archive)

After that, LA disappeared, and lipohypertrophy (LH) lesions took over. Currently, LH represent 95% of the local insulin injection complications and involve significant metabolic consequences representing cardiovascular risk factors.15-18 such as hypoglycemia, wide glycemic variability, and poor metabolic control. Such phenomena are well-known, and extensive literature on LH epidemiology, risk factors, and consequences is available. Nevertheless, LH are as widespread as 47% of insulin-treated patients on average, with peaks of almost 70% according to some authors.19,20 However, only a few attempts have been made to understand why patients fall into so many injection technique errors.
The reason for such a wide variability in LH rates relies on the different diagnostic tools used despite readily available national and international recommendations,17,18,20,21 the non-observance of a structured, systematic search for lesions21,22 and the limited interest of healthcare professionals to the argument. Therefore, this insulin treatment complication can fully be defined as “forgotten”.22,23
RISK FACTORS FOR LIPOHYPERTROPHY
Risk factors underlying such a high LH frequency include:
• Failure to rotate injection sites, concentrating the shots areas as small as a credit card15
• Reuse of the same needle several times15,20,22,23
• Cold insulin injection23,24
• Longstanding high number of injections/day23
• Large injected volume (still debated, though)23
• Use of long and thick needles (now mostly substituted for by ultra-short and ultra-thin ones).25-27
CONSEQUENCES OF LIPOHYPERTROPHY
A Case of Imperfection
Lipohypertrophy are not mere imperfections. They have severe metabolic consequences, leading to distorted insulin absorption and impacting the blood glucose profile. A few years ago, we published the case of a lady who had a visible LH on the abdomen and wanted to wear a bikini on the beach during the summer season. So, she repeatedly and vigorously massaged the unsightly fatty lump on her abdomen using the most disparate cosmetic creams.
The result was that she woke up in the emergency room in the hospital after a severe hypoglycemic event – which she did not remember at all – caused by the “squeezing” of the insulin trapped in the LH nodule.28
A Case of Monster-Lipohypertrophy
In another case, we describe the presence of two LHs arranged symmetrically on the sides of the navel. They were as large as two mandarins with a hollowed, hyperchromic center, which turned out on ultrasound examination to be an LH with gelatinous/liquid content. The liquid extracted and analyzed contained an insulin concentration 13 times higher than the circulating insulin levels! After three-years of regularly performed and proper educational training on correct injection techniques, the protuberances were over, and the dyschromia attenuated. Still, the cicatricial umbilications were only partially reduced.29,30
Beyond these anecdotal references, there is a rich literature that defines the metabolic damage caused by LH:
• Wide glycemic variability15,16,17
• Unpredictable and often severe hypoglycemia31,32
• Poor metabolic control15-32
• High frequency of chronic diabetes complications33
• Higher health care costs,33,34 including higher insulin consumption15,33,34
PRACTICAL CONSIDERATIONS
Why do patients stubbornly inject insulin into the lipodystrophic nodules? The answer is complex and largely depends on educational deficiencies when starting insulin therapy, aggravated by the lack of injection site monitoring that all diabetes teams should perform systematically and periodically.33-36
However, that also depends on the painless nature of the “mistreated” and, therefore, denervated lesioned skin tissue.34 Indeed, about half of these patients inject insulin four times a day (i.e., 1460 times per year!) and, therefore, despite aiming to attain better blood sugar levels, they do their best to avoid the annoying and systematic pain upon injection.
WHY DOES A PERSON WITH DIABETES GRADUALLY FORGET LESSONS LEARNED?
The answer is not simple, but one can resort to a fundamental principle of therapeutic education, borrowing the axiom that says “knowing is not the same thing as knowing how to do”. Indeed, Charlie Brown (the famous character of the creator of cartoons Charles M. Schulz) said to Lucy that he had taught Snoopy to whistle and, when objected that Snoopy could not whistle, reacted that he had taught him to, which did not necessarily mean that Snoopy had learned. A primary principle of medical pedagogy and therapeutic education is verifying learning in the field.37 As early as 1972, American diabetologist Leona Miller observed that people with diabetes were hospitalized more frequently and had a more extended stay than those without diabetes. Furthermore, by analyzing all hospitalizations and their causes, she realized that many could be avoided by providing the population with continuous educational support and telephone service to help manage problems. Miller had therefore activated a 24-hour telephone service in her operating unit to help address issues related to the disease. In addition, all patients who went to the hospital emergency room for matters related to diabetes were automatically redirected to the telephone counseling service and, only if deemed appropriate, re-admitted to triage. Following the setting of this system, she observed a 44% reduction in hospitalizations of patients with acute complications (hypoglycemic coma, hyperglycemia, leg amputation due to necrotic foot lesions) in just two years and an 80% reduction in hospitalizations for those regularly followed by the clinic with an estimated saving for the health system of 3.4 million dollars.38
In addition, as diabetes is mostly asymptomatic, patients pay attention to issues less crucial for health, yet relevant for daily routine. For instance, elderly people with arthropathies and motor difficulties face problems at uncomfortable-to-reach skin areas or are used to longstanding hard-to-die habits, or even display poor self-care due to a slightly depressed mood, a typical trait of diabetes. Finally, it should be remembered that it is challenging to intervene in consolidated errors and bad habits after years of incorrect insulin injections (unpublished personal observation).
WHICH CLINICAL FALLOUTS ARE EXPECTED FROM A POOR INJECTION TECHNIQUE?
First of all, a randomly irregular absorption of the insulin injected into the LH disrupts the expected synchronism between the post-meal rise in blood sugar and the immediate glucose-lowering effect of the drug. Such phenomenon inevitably leads to the above-mentioned metabolic changes potentially precipitating cardiovascular events.39
In the second place, glucose control worsens, with frequent sudden drops in blood sugar not explained by known common causes like food errors, missed meal, vomiting, diarrhea, or wrong insulin dose calculation. All this represents a metabolic challenge for the whole family.34
An episode of severe hypoglycemia, i.e., one causing unconsciousness, requires the intervention of a family member, a caregiver, or any other person and, sometimes, short-term hospitalization through emergency calls to the family doctor or the first-aid number. Such an episode may also cause the absence from work to the patient and caregiver.34
The national tariff of health services allows the calculation of increased costs due to LH complications. We recently found ten times higher costs of hypoglycemia in diabetic patients with LH than in those without LH and showed them to drop by over eight times, i.e., almost down to control levels, after an adequate, systematic multimodal educational training on correct injection techniques.33,34
Also, daily insulin doses can be 20-25% lower when injected into the healthy skin rather than injected into LHs nodules. This brings about savings, too, which, although twenty times lower than those due to prevented hypoglycemic events, is of great economic value if projected on a broad scale to large populations living on basal and fast-acting insulins.15,32,33,34
We found the following uncommon sources of injection errors: (i) the choice of unusual, not recommended skin areas (Figure 3), (ii) careless needle screwing onto the pen with internal needle bending on the upper rubber tip and thus preventing insulin from flowing into the patient’s subcutis; (iii) broken needle stumps inadvertently left in the upper grommet of the pen causing insulin to flow through the freshly inserted needle only partially and to be dispersed out for the rest (Figure 4); (iv) failing to remove the innermost needle shield, which prevents skin piercing (Figure 5); (v) the habit to syringe insulin out of a pen container rather than out of a vial (Figure 6). We could record all the above errors merely by paying attention to our patients’ behaviors (unpublished personal data) and have never been the subject of systematic studies. However, they might be much more frequent than we can imagine. We will not know that until we are ready to check our patients systematically for the injection sites, the devices employed, and device handling during insulin injection.
Figure 3. Example of Incorrect Injection Site: Lipohypertrophy in the Volar Site of the Forearm, Shown by the Arrow, Just Below the Crease of the Elbow (Personal Archive)

Figure 4. Needle Stump Broken, shown by the Arrow, Remaining Within the InsulinPen Rubber. When a New Needle is Screwed onto This Pen, Some of the Insulin Leaks Outside Through the Needle Stump, Thus Changing the Injected Dose (Personal Archive)

Figure 5. Components of an Insulin Pen Needle. The Arrow Indicates the Internal Needle Protection, Not Always Removed by the Patient at the Time of Injection: In That Case No Real Injection Occurs and the Insulin Flows Out of the Skin (Personal Data)

Figure 6. Incorrect Practice of Aspirating Insulin from a Pen with a Syringe. Apart from the Economic Waste, Pressure Differences Inside the Pen Reservoir will Affect the Accuracy of the Following Injection (Personal Archive)

WHAT CAN WE DO TO PREVENT LIPOHYPERTROPHY?
Indeed, the picture is not comforting. Suffice it to say that a recent survey conducted in China on several hundred care providers (doctors and nurses) mercilessly documents that over 50% of physicians know little or nothing about LH and their metabolic consequences. What is worse, they do not know how to avoid or counter them.40 Nor is it any better in the nursing field. We can easily understand this phenomenon after reading the results of a national survey conducted in China on Knowledge, Attitudes, and Practices of over 200,000 nurses from various hospital departments, from which emerges the pressing need for an improvement in skills and clinical practice, although slightly less than for doctors.40-42
Things are not better in the Western world, where the presence of LH in at least 45% of patients living on insulin mercilessly documents the inefficiency of its treatment system.34
Apart from a few willing people who strive for therapeutic education (including that on correct injection techniques) all the time, in most cases, LH does not represent an issue simply because forgotten or ignored.19,20,41
So? Considering that 3 to 4 million people with diabetes live in Italy and that about 40-50% of these will sooner or later be on insulin, both doctors and nurses should follow specific educational courses with practical refreshers on correct injection techniques. Therefore, in the university courses, postgraduate courses, and specialization courses, more emphasis should be given to correct insulin injection techniques, and general practitioners (GPs) clinics and diabetology units should provide specific educational courses on insulin injection methods. In our youthful memories of university courses, none of such classes existed, and only the experience in the field sometimes made up for the training gaps in the following years. As explained so far, only a few doctors and nurses take on the issue of LH due to incorrect injection techniques initially, by showing what to do at the moment of first insulin prescription or, during follow-up visits, verifying injection sites and supporting patient knowledge and skill maintenance.
Finally, insulin manufacturers could include visuals and detailed descriptions of how inulin is injected and handled in pen and vial packs and not just how you use your devices.
HOW TO CURE LIPOHYPERTROPHY LESIONS?
Clinicians proposed several topics on treatment approaches, including liposuction, aesthetic surgery, enzyme-based/corticosteroid cremes, and massage, in addition to changing the injection site. The latter is the most consistent solution, considering that LH depend on repeated traumas and/or anabolic insulin-related signals inducing macroadipocyte differentiation and fibrous reactions.15,43 Corticosteroids, liposuction, and aesthetic surgery have not provided significant results so far, although, based on our own experience, they might be beneficial in particular cases.15,44 Several ‘‘suggestions” in favor of soothing cremes and massage lacking scientific evidence are also available on the web. However, as from a case report published by our group, the thermic and mechanical effects of massage can even be dangerous because of eventually occurring untimely release of LH-stored insulin into the bloodstream, and consequent severe unexpected hypoglycemic events.28,29
Preliminary data are available on 3C-Elastargene (Colipex®, Harmonium Pharma, Italy), i.e., a product proposed as an emollient and soothing skin care body cream, specifically designed to improve LA in children and adolescents with type 1 diabetes (T1D), using insulin pump therapy.45
A 6-month, double-blind, randomized trial to test the efficacy of 3C-Elastargene in children with T1D using insulin pumps was conducted. The main aim of the study was to evaluate the cream’s effectiveness in improving patients’ skin healing, and making disappear the white scars usually left after infusion set removal. The secondary aim was to evaluate any effect of the cream on metabolic control. The investigators observed: (i) glycated haemoglobin (HbA1c) significantly improved in patients using 3C-Elastargene (baseline 8.08±0.80%, after 6-months 7.51±0.53%, p=0.005, delta -0.53%), but not in the placebo group (baseline 7.98±0.74%, after 6-months 7.76±0.79%, p=0.19, delta -0.22%); (ii) no differences were found in body mass index (BMI) or insulin requirement before study vs. after 6-months; (iii) white scars wholly disappeared in 8 patients and improved in 10 within
the 3C-Elastargene group, vs. no changes observed in the placebo group.45
However, even these data are entirely preliminary and deserve further studies on a more comprehensive range of patients.
The fact is that the only real weapon we have at our disposal today against LH is a correct and complete structured educational action, periodically repeated over time and the veri ication of injection habit changes in patients on insulin. Only the time elapsed between the change in behavior from incorrect to correct, by letting the areas of traumatized LH tissue rest, can allow the skin to recover a previously lost condition of normality. There are no data on the duration of this process. Still, by experience, 6-months to a few years28-30 are needed for that, depending on the LH size and features because the larger LHs are, the longer the time necessary for their resorption.
Unfortunately, most people who don’t need to inject insulin into their skin attach little importance to the injection. Vice versa, it takes on much more relevance for those who use the insulin pump or perform 4 injections per day, i.e., 1460 injections per year!46
That’s the reason why we feel like stressing this concept until translated into real practice.
Guidelines, recommendations, consensus documents should pay more attention to correct insulin injection technique.47
ACKNOWLEDGMENTS
We are indebted to Paola Murano, General Manager of the Nefrocenter Research Network, for the effective and continuous, spontaneously offered support toward carrying out the paper. Special thanks go to patients who have consented to be photographed for this publication.
FUNDING INFORMATION
No funding or sponsorship was received for this study or the
publication of this article. None of the authors or coworkers received funding or another type of payment for this paper.
AUTHORSHIP
Felice Strollo, Giuseppina Guarino, Ersilia Satta, Carmine Romano and Sandro Gentile contributed equally to the conception and
drafting of this paper. All named authors meet the International
Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the
work as a whole, and have given their approval for this version to
be published.
DISCLOSURES
None of the authors has received funds or any form of direct or indirect financing for this article or has incompatibility with the contents of the text.
COMPLIANCE WITH ETHICS GUIDELINES
The manuscript does not directly use human or animal data for which it does not respond to this need, and therefore does not even require an authorization procedure.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.