INTRODUCTION
Difficult laryngoscopy has been shown to be more frequent in cardiac surgery versus general surgery. In one study, the incidence of difficult laryngoscopy in cardiac surgery was almost double that compared to general surgery patients.1 The incidence of difficult laryngoscopy is also higher in diabetic patients, with an incidence reported to be as high as 30% in long-term diabetics.2 In Singapore, the prevalence of diabetes mellitus in patients presenting for coronary artery bypass grafting (CABG) is high and despite a seemingly normal airway examination based on head and neck examination, one may encounter unexpected difficulties.
CASE REPORT
We present a 53-year-old man diagnosed with triple vessel coronary artery disease (CAD) scheduled for CABG. He weighed 64.4 kg, was 163 cm tall and had a body mass index (BMI) of 24.2. He had a significant 30-year history of juvenile onset diabetes with a fair blood glucose control demonstrated by a recent HbA1C of 7.9%. He was on a subcutaneous insulin regiment of Mixtard 34 units in the morning, 15 units at night, and oral Metformin 250 mg twice a day.
His complications related to diabetes include hypertension and ischemic heart disease. He had suffered two previous myocardial infarctions that were treated with percutaneous coronary interventions. His pre-operative transthoracic echocardiogram showed a left ventricular ejection fraction (LVEF) of 20% and he had multiple previous hospital admissions for congestive heart failure. His renal function was otherwise normal with an estimated glomerular filtration rate (eGFR) of 102 ml/min. He did not have retinopathy or neuropathy prior to surgery.
On examination of his airway, his mouth opening (>3 finger breadths), thyromental distance (6 cm), and neck mobility were normal. Mallampati score was II and his dentition was normal. No difficulty with intubation was anticipated.
Standard monitors (e.g., 5 lead ECG, pulse oximetry), a right radial arterial line, and right internal jugular central venous catheter were placed prior to induction. Following induction of general anaesthesia, successful bag mask ventilation was confirmed before neuromuscular blockade was given.
Direct laryngoscopy with a Macintosh blade revealed only the tip of the epiglottis. The laryngoscope blade was advanced deep into the vallecula, but lifting the epiglottisto visualise the vocal cords was difficult as it was very stiff. Attempts to intubate with a stylet or a bougie using a video laryngoscope were also unsuccessful. A straight Miller blade was then used, which just lifted the tip of the epiglottis, allowing a tactile blind maneuver of a bougie through the vocal cords. An endotracheal tube was then successfully railroaded over the bougie into the trachea.
The surgery was uneventful and the patient made a full recovery. Post-operatively, the patient was assessed for limited joint mobility associated with diabetes mellitus and he demonstrated a positive Prayer sign. (Figure 1)
Figure 1: Limited Joint Mobility Syndrome Demonstrated by the “Prayer Sign”.

DISCUSSION
Limited joint mobility syndrome (LJMS) or diabetic cheiroarthropathy is a long-term complication of diabetes mellitus with an incidence of 8-58%.3 It is associated with microvascular and macrovascular complications of diabetes.
LJMS typically affects metacarpophalangeal and proximal interphalangeal joints. It manifests as progressive, painless stiffness in the hands and fingers, fixed flexion contractures of metacarpophalangeal joints with thick, waxy scleroderma-like skin appearance. Patients are unable to approximate the palmar surfaces of the phalangeal joints, exhibiting what is termed the “prayer sign”.
LJMS may also affect other joints of the body leading to other sequelae. For example, involvement of the joints of lower limbs, increase the risk of falls in diabetic patients.3 It has also been proposed that this joint rigidity may also affect the cervical and laryngeal areas making laryngoscopy more difficult.4 Salzarulo et al5 were the first to report “Stiff Joint Syndrome” as a cause of difficult intubation back in 1986. They attributed their difficulties to the limitation of movement at the atlanto-occipital joint.
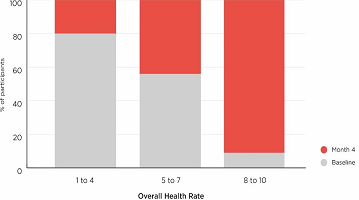
The palm print has been used as an objective assessment of the degree of interphalangeal joint involvement. It is obtained by painting the palm of the dominant hand and pressing it firmly, with fingers spread, against a white piece of paper. A palm print score from 0-3 based on the degree of visibility of phalangeal areas on a piece of paper has been assessed as a factor to predict difficult laryngoscopy.4,5,6,7 Several studies have compared it to other common clinical airway indices such as the Modified Mallampati score, thyromental distance and degree of neck extension and have found it to be the most sensitive predictor of difficult laryngoscopy in diabetic patients with sensitivity ranging from 75-100%.6,7 The palm print test when used in combination with other airway assessment indices may improve the predictability of difficult laryngoscopy.
CONCLUSION
In conclusion, the palm print test is a useful and easy bedside test which can be used in combination with other clinical indices to help better predict difficult laryngoscopy in long-term diabetic patients.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONSENT
Consent has been taken from the patient for purpose of using patient photograph for publication in print or on the internet.