INTRODUCTION
Type 1 diabetes may be considered one of the most common endocrine and metabolic conditions worldwide, affecting nearly half a million children under the age of 15 years.1 Roughly 80,000 new cases involving patients younger than 15 years are added every year and an anticipated rise in incidence of 4% may be expected.2,3,4Best estimates are that between the ages of 15 to 25 years, another half a million young individuals are likely to have type 1 diabetes.
The ocular complications of type 1 diabetes can be blinding. Blindness in the younger population inflicted with type 1 diabetes can have lifelong, catastrophic consequences on quality of life, ability to live independently, education, productivity and longevity. In considering a worldwide distribution, one quarter of children with type 1 diabetes live in Europe, while 23% live in Southeast Asia. North America and the Caribbean represent roughly 19% of cases.5 China, with a population of 1.3 billion, is also experiencing a rise in type 1 diabetes with an incidence of 0.59 per 100,000 persons per year.1This number may appear deceivingly low when compared to that of the European countries; however, it is staggering when taking into consideration the total population of the country. In viewing mortality rates, children residing in high-income countries afflicted with the disease, have a mortality rate doubled than that of their counterparts without the disease.6 In Sudan, the mortality rate is 42.6 deaths per 100,0007 as compared to 0.63 deaths per 100,000 in the same age group of children living in the United States.8
Early detection of diabetic eye disease can lead to early treatment and prevention of this vision loss. The purpose of this study was to assess the feasibility of performing large-scale screenings of children with type 1 diabetes and their accompanying families using a non-mydriatic digital camera. In utilizing this technology, we integrated high resolution capturing devices; as well as, digital post-processing imaging as part of an efficient screening protocol. Further evaluations of this process included auto refraction, visual acuity, intraocular pressures and Spectral Domain-OCT analysis.
MATERIALS AND METHODS
Retinal screening was performed during the annual Friends for Life (FFL) Conference in Orlando, Florida between July 1 and July 6, 2014. Friends for Life is the largest association dedicated to educating children with type 1 diabetes and their families on all aspects of the disease. In addition to providing families with the most advanced knowledge in diabetes care, FFL offers education regarding eye health and a respective retinal screening to all children with type 1 diabetes.
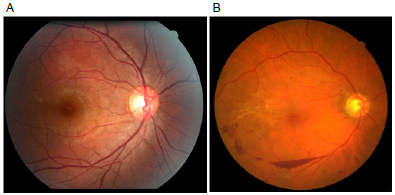
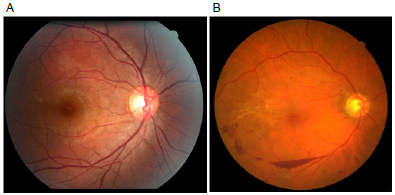
The screening program captured both right and left eyes of children as young as 5 years of age without the use of mydriatic agents. All images were captured in a dimly lit room at a level of 125 candelas. Retinal screening was performed utilizing a Canon CR-2 Plus AF (Tokyo, Japan) non-mydriatic retinal camera with a CMOS chip, a resolution of 18 megapixel and an ISO setting of 400 (range available is from 200 to 6400 ISO). The CR-2 Plus AF has a 45-degree field of view and minimum pupilary dilation of 3.3 mm that enables multiple images to be stitched together to increase the field of view of the posterior pole from 45 degrees to 110 degrees. We used the autofocus function of the Canon CR-2 Plus AF; as well as, the auto capture (with blink detection preventing unintentional capture). To improve imaging quality, we made use of the auto exposure feature that resulted in consistent, good color (hue); as well as, good overall exposure and balance of all captured images. It has been well documented that a static image, such as a retinal photograph (Figure 1A), has a higher sensitivity in pick-up rate for evidence of retinopathy as seen in Figure 1B; as patients tolerate better a single flash than continuous bright light from an indirect ophthalmoscope.9-11 Furthermore, with high-resolution digital imaging, it becomes possible to separate specific layers of the posterior pole.
Figure 1: A. Healthy, retinal view at an angle of 45 degrees. B. View of the posterior pole demonstrating retinal hemorrhages of a subject with DM1.
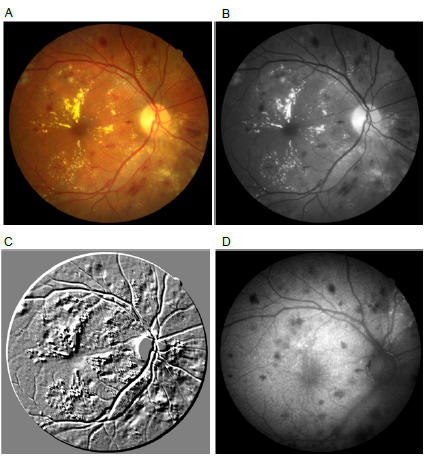
A typical color image is composed of Red, Green, and Blue (RGB) light. All images were postcapture-processed using a propritary software, image SPECTRUM V5 (Canon USA, Irvine, CA, USA) that met all FDA as well as HIPAA regulation standards. The postcapture imaging software automatically separates a color image into 3 monochromatic images highlighting the area of the retinal layers (green channel at about 550 nm) of a subject with diabetic retinopathy findings (Figures 2A, 2B and 2C). Figure 2D illustrates a fundus auto-fluorescence of the same eye, highlighting retinal hemorrhages and masking the exudates seen in other modalities as seen in Figures 2A, 2B and 2C.
Figure 2: A. Color photo of patient with diabetic retinopathy and posterior pole exudates. B. Monochromatic view of red free extraction of color image. C. Topographical view of retina demonstrating 3D-like view of the retina with retinopathy and exudates. D. Fundus Auto-Fluorescence image demonstrating retinal hemorrhages and masking macular exudates.
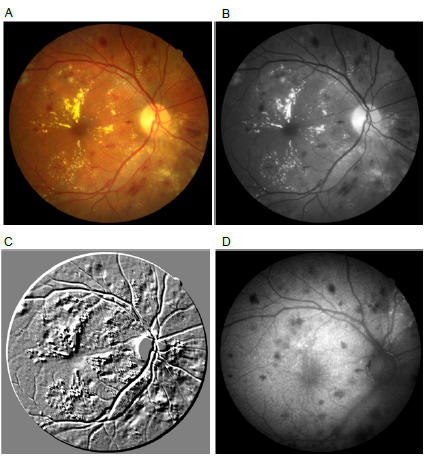
In the search for evidence of diabetic retinopathy, using a green (red free image), monochromatic channel postcapture, increases the image contrast and can highlight small dot hemorrhages that can otherwise be missed. RGB allows a visual representation of where the event is happening; for example, if there is a retinal hemorrhage, it will be best seen in the G channel, thus confirming retinopathy. Another post-processing filter used in screening for retinopathy is called Emboss. This pre-set monochromatic filter allows us to observe the captured retinal image in 3D, topographical view of the green layer of the retina at 550 nm (Figure 2C). Retinal auto-fluorescence is another area of interest in ocular imaging that looks specifically for lipofuscin. We used auto-fluorescence imaging to determine if small changes associated with retinopathy could be visualized. Subjects with a positive finding (mild diabetic retinopathy) were counseled and a referral to an ophthalmologist was recommended.
RESULTS
One hundred and fifty eight children with type 1 diabetes underwent retinal screenings throughout the 2014 Annual Meeting of “Friends for Life”. The children ranged from 5-30 years of age, with a mean age of 14 years. Seventy nine percent (79%) of the children were Caucasians, with twenty-one (21%) reported as “Other Race” and 56% were females. Duration and HbA1C were self-reported, with a mean of 7.8 years (range 0.4 to 25 years) and 7.9%, respectively. Visual acuity was 20/20 for 57% of the right eye and 61% for the left eye. Table 1 provides patient demographics along with clinical characteristics of the screened population. Our success rate for artifact-free images was 92% for all screened children and a 5% pick-up rate was found for early signs of diabetic retinopathy in this population.
Table 1: Patient demographics and clinical characteristics.
|
Race
White 79%
Other 21%
|
|
Age (y)
Mean 14
Range 5 to 30
|
|
Gender
Male 44%
Female 56%
|
|
Duration of DM1 (y)
Mean 7.8
Range 0.4 to 25
|
|
Visual Acuity
Right (20/20) 57%
Left (20/20) 61%
|
In subjects with positive findings, retinal pathology was noted on digital imaging and involved retinal hemorrhages and vascular changes consistent with microaneurysms. No subjects presented with proliferative diabetic retinopathy and one subject presented with a cataract.
DISCUSSION
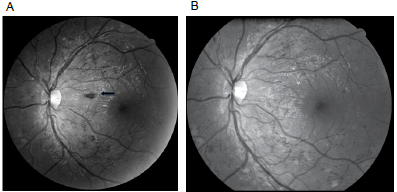
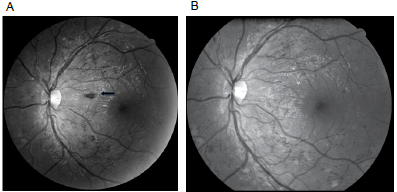
The Friends for Life organization prides itself on several objectives; one of which is to connect families with one another, while educating them on the nature of type 1 diabetes and how to prevent its complications. The complications of type 1 diabetes are caused, but not limited to, duration or onset of diabetes, poor control of glucose levels (H1 AC) and a combination of poorly controlled HbA1C and high blood pressure (Figures 3A and 3B).
Figure 3. Retinal images of DM1 left eye. A. Complications of DM1 due to a combination of poorly controlled H1 AC and high blood pressure with associated flame hemorrhages. B. Result of improved control of H1 AC and high blood pressure three weeks post screening.
Routine, yearly retinal exams are performed to help manage and educate children and their families to maintain healthy retinas. Advanced imaging technologies permit us to utilize high resolution digital imaging to enable analysis of various layers of the retina and determine the health of the nerve fiber layer, retinal layers and the choroid. With diabetes, our primary interest lies in the retinal layer best visualized in the green (red free) layer. As the initial image resolution of the Canon CR-2 Plus AF is 18 Mp, when separating the layers into RGB, one is left with 3 images with resolutions of roughly 6 Mp each. This allows us to best observe changes which could be missed with lower resolution. In addition, when performing auto-fluorescence imaging (that does not require the injection of sodium fluorescein to the subject), we have been successful in identifying new areas of retinopathy not yet visible in baseline color retinal imaging as demonstrated in Figure 2D. The inability to determine an imaging technology as a gold standard presented as a limitation to our study. However in future studies, confirmation through office physical examination can be performed.
Although a gold standard for imaging technology has not been determined, these emerging technologies assist in an early diagnosis and are made readily available to patients and their families throughout the event.
CONCLUSION
Ocular complications associated with type 1 diabetes post +/- 12 years of onset of the disease may include: diabetic retinopathy, macular edema and cataracts if left unchecked. With the prevalence of diagnosis at a young age, type 1 diabetic patients can experience vision complications by the time the child is a teenager. Duration of the disease, poor glycemic control, elevated blood pressure and sedentary life style all pose as risk factors to retinopathy that if left unchecked, can lead to vision loss and even blindness. The purpose of yearly exams as recommended by the American Academy of Ophthalmology,12 the American Academy of Optometry;13 as well as, the American Diabetic Association14 is to detect early ocular changes.
Retinal imaging used in mass screenings can help identify early retinal changes; as well as, aid in the management and care of retinas demonstrating changes associated with diabetes. Advances in digital imaging software can assist eye health care providers in the detection and isolation of ocular events. Remote reading centers can use advanced imaging tools to best isolate and detect subtle changes easily missed in early signs of retinopathy. In our experience, use of both remote telemedicine and high resolution imaging systems, with associated software management systems, can greatly aid in the intervention and maintenance of the patient’s ocular care. Thus, early detection is pivotal in the management of and in maintaining vision and quality of life for children with type 1 diabetes.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest
CONSENT
Consent was obtained at the time of examination.