Maintaining good nutritional habits is key to optimal human body functioning. It’s important to understand not only what nutrients the body requires but also how much. Providing nutrients adequately can be challenging without an understanding of what the body needs, why nutrients are needed, and how to get them. A healthy diet provides the body with everything it requires to function at its best. Most dietitians recommend a balanced and nutritious diet, in terms of quantity and quality, to maintain or lose weight and improve health. We need energy daily from the food items we consume to keep our bodies functioning properly. This is measured in terms of calories. Nutrients that provide food energy are carbohydrates, proteins, and lipids. It’s important to be mindful of how many calories we consume, as exceeding our body’s needs can result in weight gain, which is stored as body fat.
To ensure proper bodily function, it’s important to recognize and be reminded of the following variety of necessary nutrients: 1) Water does not provide energy, but it is crucial for maintaining good health. If insufficient volume is consumed, a person runs the risk of becoming dehydrated and potentially developing serious health problems. Although fresh and raw fruits and vegetables are sources of water, it’s important to drink water regularly throughout the day, even if thirst is not felt. 2) Carbohydrates are great sources of energy and help maintain the balance of bodily fluids. Dietary guidelines recommend that 45-65% of daily caloric intake should come from this class of nutrients. 3) Proteins are essential for maintaining and repairing tissues. For adults who are physically active, it’s recommended that proteins constitute 10-35% of the daily caloric intake. Proteins are made up of amino acids, nine of which are known as essential because our bodies cannot produce them on their own and must be provided by diet. The presence of these essential amino acids (histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine) determines the quality of a protein. Deficiency in any of these essential amino acids can lead to various health problems such as muscle wasting, impaired immune function, and neurological disorders.1 Thus, to ensure optimal health, it is important to have an adequate amount of these essential amino acids, which are found in animal products like meat, eggs, and dairy or from plant-based sources such as beans, nuts, and seeds. 4) Lipids (fats and oils) need to be consumed in controlled and limited amounts. Energy from lipids should not exceed 30% of the total daily caloric intake, and saturated fats should make up less than 10% of consumed lipids. Limiting lipid intake can help maintain a healthy weight and reduce the risk of disease. Cholesterol and trans-fat ought to be consumed in extremely limited amounts. 5 and 6) Minerals and vitamins are required to maintain healthy bones and a normal metabolism. To ensure having enough minerals and vitamins, it’s recommended to consume a diverse range of nutritious food items, particularly fresh fruits and vegetables. However, some individuals may find it difficult to obtain all the necessary nutrients through diet alone and may benefit from vitamin and mineral supplements. It’s advisable to talk with a dietitian and other healthcare providers before taking any dietary supplements.
To ensure that healthy people would get all needed nutrients daily, a simple guide known as “MyPlate” (Figure 1) was devised by the United States Department of Agriculture (USDA).2 The aim of developing this method is to promote a balanced diet by dividing it into five food groups: fruits, vegetables, grains, proteins, and dairy. To follow this method, half of the plate should consist of whole fruits and a variety of vegetables, while one-quarter of the plate is devoted to grains, especially whole grains, and one-quarter to lean proteins. On the other hand, include a serving of low-fat or fat-free dairy milk or yogurt. This approach encourages a balanced diet that includes essential vitamins, minerals, and fiber while restricting unhealthy fats, such as saturated and trans fats, as well as excess sodium and added sugars.
Figure 1. MyPlate Food Guide2
According to a study published in the Journal of the Academy of Nutrition and Dietetics, planning meals using MyPlate was linked to better diet quality and more healthy dietary intakes.3 Meanwhile, this method may not be effective in changing dietary behavior if there are no healthy food options available for people.4
Disability is defined as a physical or mental impairment that limits a person’s ability to perform daily activities or participate in society. Disabilities can occur with the natural deterioration of bodily functions, as in the case of advancing in age, or be acquired due to congenital defects, the development of disease conditions, acquired injuries, and/or severe cases of substance abuse and addiction. Individuals with disabilities may not be able to function in life like normal and healthy people. Their situations can worsen due to disease conditions, which add difficulties to their lives. People with disabilities either live with their families and are cared for by their caregivers, or they reside in special institutions and centers and receive care from professional care teams. It is known that nutritional requirements vary according to many factors, among which are stage of growth, gender, physical activity level, and aging. As would be expected, special nutritional needs ought to be considered in cases of disability, with or without the presence of disease. Caregivers of individuals with disabilities, whether at home or in institutions, should have a basic understanding of human nutrition and the ability to evaluate appropriate diets for their recipients.
Research is increasingly directed towards studying aspects of nutrition for individuals with disabilities and related issues. Findings from examples in this field are illustrated herein. Adolescents and children with intellectual disabilities face challenges with food preparation or eating independently, which can put them at higher-risk for micronutrient deficiencies and obesity than their same-age peers.5 Generally, feeding difficulties have been identified by studies as a risk factor for inadequate nutritional status among children with disabilities. Children with neurological impairment and gastrointestinal disorders, as well as feeding difficulties, may suffer from malnutrition due to difficulty consuming enough calories and nutrients to maintain an adequate nutritional status. Implementing a standardized nutritional intervention, such as home enteral nutrition (HEN), as part of a multidisciplinary care approach can improve the nutritional status of these children.6 Constipation is a common issue experienced by adults with intellectual and developmental disabilities (IDD). This is often caused by neuromuscular abnormalities, a suboptimal diet, physical inactivity, poor oral intake, and medications that can further aggravate the condition. Healthcare providers can improve the health and well-being of patients with IDD by using recent evidence-based practices.7 To optimize the nutrition of children with disabilities, it’s important to raise awareness among parents and teachers about their dietary needs. This can be done through ongoing nutrition education and providing appropriate nutrition options to cultivate healthy eating habits in children with disabilities.8 People with intellectual disabilities (ID) are vulnerable to having difficulties with feeding and swallowing, which can lead to malnutrition, aspiration, and choking. To address this, a team of health professionals should work together, including a qualified speech-language pathologist (SLP) and a dietitian, to modify the person’s diet as needed. However, there is still a need for more research in this field. If appropriate, nutritional support should also be given. Studies have demonstrated that enteral feeding may enhance nutritional status and lower the occurrence of respiratory infections in individuals with ID.9 Children and adolescents who have cerebral palsy and severe disabilities are at a higher-risk for malnutrition, growth failure, and poorer nutritional status than healthy children.10 Patients with stroke are at risk of death and disability due to difficulty swallowing and poor nutrition. Therefore, it is advisable to provide oral nutritional supplements (ONS) to those who are malnourished or are at risk of malnutrition but do not have difficulty swallowing.11 For people with disabilities who have difficulty swallowing or have gastrointestinal disorders, nutritional support may be necessary. This can include enteral or parenteral nutrition. To ensure adequate nutrient intake and prevent complications, it is important to seek guidance from a dietitian when providing nutritional support.
Several studies have shown that malnutrition, specifically undernutrition, is a significant concern for elderly individuals, regardless of where they live, whether in developed or underdeveloped countries. According to one study, older adult patients diagnosed with congestive heart failure (CHF) who are malnourished are at a higher-risk for poor physical function and disability.12 Assessing the nutritional status of older adults through validated screening tools in the early stages can lead to better nutritional therapy for illnesses that are linked to malnutrition. This is particularly important given recent research that has improved our understanding of the aging process and the nutritional requirements of older adults. It’s crucial to establish treatment goals carefully and encourage collaboration among different health-related disciplines. Proper nutrition for elderly individuals is challenging because of the complexity involved, as detailed in a special report.13
Despite the type of disability encountered, all individuals ought to be provided with the nutrients that their bodies need. Sound dietary and nutritional intake should be adequate in both quantity and quality to support their growth and maintain their bodies. Some individuals with disabilities lead active lives and even participate in sports, making their nutrition especially important. Others may be bedridden or paralyzed and require special attention to the delivery of nutrients. Unlike the normal public, and due to their disabilities, they may encounter more challenges in maintaining a healthy diet. While there are presently no specific nutritional guidelines for people with disabilities, most experts recommend a balanced calorie intake for a healthy weight, along with adequate protein for muscle growth and repair. It is advisable that the disabled consume diets that contain high-fiber foods for regular bowel movements and those that provide adequate amounts of minerals and vitamins. Consistent hydration can be achieved through water and electrolyte-containing fluids, and texture-modified foods can be consumed for easier swallowing. It’s important to consult a dietitian for personalized nutrition plans based on individual needs.
It is important to realize that everyone has unique dietary needs, especially the disabled, depending on the type and severity of their disabilities. In addition to the type and extent of disability, requirements for both macronutrients and micronutrients vary according to individual factors like age, gender, and physical activity. For example, individuals with disabilities who are sedentary or semi-sedentary may require different (lesser) amounts of calories based on their age, gender, body composition, and physical activity level. Guidelines for daily energy requirements for sedentary women aged 19 to 30 are around 1800-2000 calories, and for sedentary men of the same age group, they are 2400-2600 calories. For those who are moderately active, daily energy requirements increase to about 2000-2200 and 2600-2800 calories, respectively.14 It would be expected that the daily energy requirements of disabled individuals who are sedentary or semisedentary would be lower than those of those who exert physical activity. However, it is important to note that energy intake for any disabled individual ought to be calculated carefully.
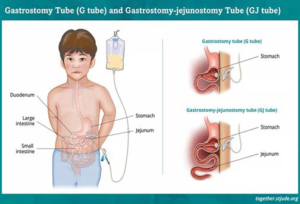
Generally, adults with and without disabilities require similar amounts of macronutrients (carbohydrates, proteins, and lipids) and micronutrients (minerals and vitamins); however, the recommended intake for micronutrients may differ based on individual needs. For instance, individuals with certain disabilities may need higher or lower-levels of specific micronutrients due to malabsorption issues or nutrient-medication interactions. That’s why it’s crucial to consult a dietitian to create a personalized nutrition plan that takes into account the existing medical condition, disability type, and overall nutritional status based on a thorough assessment. In certain situations, artificial (tube) feeding may be necessary. The nasogastric (NG) tube is a tube that is inserted through the nose and into the stomach. A visual representation of the NG is in Figure 2.15 The gastrostomy (G) tube is inserted directly into the stomach, and the gastro-jejunostomy (GJ) tube is inserted into both the stomach and small intestine, as shown in Figure 3.16 In cases where people with disabilities are unable to consume solid food, a specially formulated liquid known as an ONS can be administered through a tube to meet their optimal nutritional needs. Such is also known as nutrition support therapy, which is decided upon to be either enteral nutrition (EN) or parenteral nutrition (PN).
Figure 2. Guided Feeding Tube Placement through the Nose (NGT)15

Artificial methods of feeding patients, along with other interventions that prolong or support life, are often the subject of controversy. Patients who have suffered a severe head injury and slipped into a coma cannot eat on their own. Similarly, patients who have experienced severe strokes may face serious difficulties swallowing, making oral feeding impossible. Attempting to give food orally can result in “aspiration pneumonia”, as the food may be taken down into the lungs. To prevent aspiration pneumonia, patients and/or their families (with the required consent) may request that the doctor place a feeding tube. These tubes deliver liquid or powdered nutritional supplements to patients who cannot consume any food or liquid orally to avoid aspiration.
Figure 3. Guided Feeding Tube Placement through the Stomach (gastrostomy tube)16
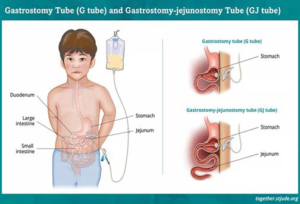
Different types of EN feeding tubes are typically categorized by their placement location, including: 1) a nasogastric tube (NG), which is a tube inserted through the nose and down the throat into the stomach for short-term nutritional support or to aspirate stomach contents; and 2) a nasojejunal (NJ) tube, which is a tube inserted through the nose and down the throat into the small intestine to provide nutritional support when the stomach is not functioning properly or to prevent the aspiration of stomach contents. Other tools are surgically inserted that include: 1) a gastrostomy (G) tube, which is inserted through the abdomen and into the stomach for long-term nutritional support for patients who cannot consume food or liquid orally; and 2) a jejunostomy (J) tube, which is inserted through the abdomen and into the small intestine for long-term nutritional support for patients who cannot tolerate feeding into the stomach. The exact caloric output capability of tube feeding varies depending on several factors, such as the formula used, the infusion rate, and the person (NG)s unique calculated nutritional needs. Patients who struggle with diseases or conditions that impair their food intake, nutrient digestion, or absorption may find it challenging to maintain good nutritional status. If tube feeding is not possible, total parenteral nutrition (TPN) is needed. TPN is a liquid mixture containing all necessary nutrients, including macronutrients, micronutrients, and other nutrients, and it is administered directly into the bloodstream via an intravenous (IV) catheter.
There are some considerations about the quality of life for patients who have artificial feeding tubes as well as those who are terminally ill that need to be addressed. Such questions include the following important ones: 1) What is the patient’s assessment of their current quality of life? 2) Are they willing to continue living, or do they wish to let go? 3) Is the patient currently conscious, or is there a possibility they may regain consciousness and achieve an acceptable quality of life in the future? 4) Will the tube procedure alleviate or worsen the patient’s suffering? 5) What are the patient’s wishes regarding this type of medical intervention?
The use of feeding tubes in individuals with disabilities and chronic diseases has been a topic of ongoing debate due to concerns about their impact on the patient’s quality of life. While some studies suggest that tube feeding can improve patients’ nutritional status and overall health, others indicate that it may not necessarily lead to an improved quality of life. For some people, the use of feeding tubes did not enhance their quality of life and worsened their overall well-being, leading to increased discomfort and distress. However, for others, the use of feeding tubes helped to enhance their nutritional status but did not necessarily lead to an improved quality of life.17 In this regard, a systemic review of sixteen relevant studies showed that when cancer patients are guided by dietitians in their use of enteral nutrition, there is a positive impact on their quality of life. Such an impact has been assessed through psychological measures and by taking other potential determinants such as malnutrition and complications into consideration. This study recommended that enteral nutrition be utilized whenever possible to prevent and treat malnutrition in cancer patients.18 Another systematic review analyzed the use of enteral nutrition in patients with dementia. While the review acknowledged potential complications, there were ethical concerns raised regarding the impact of tube feeding on the quality of life for patients. Therefore, it is crucial to consider the potential harm and benefit of feeding tubes on a case-by-case basis, using a holistic assessment, and involving patients and their families in the decision-making process.19 While tube feeding may be necessary in some cases to ensure adequate nutrition, it is important to recognize that it may not necessarily improve the quality of life for all patients, whether awake or mobile. Individuals who require tube feedings but do not receive them may experience malnutrition, dehydration, and other complications. Malnutrition can weaken the immune system, lead to muscle wasting, and delay wound healing, among other issues. Dehydration can cause fatigue, dizziness, and confusion, and if left untreated, may result in serious medical problems. In severe cases, insufficient nutrition and hydration may cause organ failure and death.
On the other hand, feeding through tubes may cause adverse side effects. Some common side effects include diarrhea, nausea, and vomiting, which can result from rapid nutrient infusion. These side effects can be managed with proper medication and by adjusting the feeding infusion rate. Infection is also a potential problem; thus, proper hygiene practices should be followed, and the tube should be regularly cleaned and maintained to prevent infection. If constipation is experienced, it can be managed with medication and by adjusting the feeding formula. Tube displacement and blockage are other potential risks that can cause pain and discomfort. To prevent these risks, the tube should be secured properly, its position should be continuously monitored, and it should be flushed regularly to prevent blockage.20 Aspiration is also a risk, which can occur when food or liquid enters the lungs instead of the stomach. To prevent aspiration, the tube should be properly placed and monitored. While these side effects can be managed with appropriate care and monitoring, it is important to collaborate closely with a dietitian, nurse, and treating doctor to ensure the feeding tube is being used safely and effectively. The benefits of tube feeding often outweigh the risks, especially for people with disabilities who cannot consume food orally.
To conclude, maintaining a balanced and diverse diet can be challenging even for people without disabilities to lead normal lives. Therefore, it is important for everyone to be aware of the basics of nutrition. This understanding will ensure the consumption of balanced and varied food options while maintaining the daily intake of the necessary nutrients. The well-being and quality of life of individuals with disabilities ought to be of concern to society at large. Proper nutrition for people with disabilities would be expected to be compromised, which requires special attention by their caregivers, qualified dietitians, speech-language pathologists, and healthcare providers. Nutritional assessment and management would be made on a “case-by-case” basis and according to the individual’s disability condition. Additionally, keeping all individuals well-hydrated should be emphasized.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.