Of the estimated 415 million people living with diabetes worldwide, 10% have Type 1 Diabetes (T1D) meaning they will remain insulin dependent until a cure is found. Globally, we can observe an increasing trend of about 5% per year in newly diagnosed cases of T1D involving children as well as adults. T1D places vital organs at risk; additionally, it increases the likelihood of contracting other autoimmune diseases. Life expectancy of individuals affected with T1D can be shortened by as much as 12 years. Careful monitoring of diabetes (glucose, blood pressure, and body mass index (BMI)), including early detection of retinal changes, is key to maintaining a long and healthy life.
For over a decade, the week of July 4 has been set aside by a group called “Children with Diabetes” (CWD) thafigurt meets in Orlando, Florida, USA (near Disney World) to educate children about various aspects of diabetes. Siblings, parents, and grandparents of children with T1D also participate in this educational, yet fun event. Earlier this month, a total of 2,300 individuals attended this event where, among many other things, families could have their children’s eyes screened at no cost with the latest technology available. A group of 16 screeners (Figure 1) with various medical backgrounds partook in this effort and for 5 days screened 216 individuals ranging in age from 4 years to 76 years (average age, 23 years).
Figure 1: “Children with Diabetes” Screening team 2016, July 2016.

Front row: C. Khouri, B. Szirth, K. Duong, M. Shah, L Deeb, L. Thangma Athesvaran,
Back row: S. Mendez, K. Soules, B. Peach, R. Ragam, K. Dunlap, J. Stroud, R. Freund, H. Cope, M. Ferm, C. Weng.
Photo credit: Corporate Image Photography.
The screenings included visual acuity measurement, blood pressure monitoring (with an average reading of 103/65 mmHg blood pressure is responsible for 38% of non-vascular damage when not controlled), BMI assessment, pupillary measurements, automated visual acuity measurement, automated intraocular pressure monitoring, ocular coherence tomography (OCT), ocular coherence tomography with angiographic views (OCTA), and non-mydriatic high-resolution 21 megapixel color and autofluorescence digital retinal imaging. Three reading/interpretation stations were set up where screened individuals and parents received both a reading of their results and digital copies of their tests.
The average age at onset of T1D in this group was 9 years, while the duration of T1D was ten years. A valuable set of innovations in T1D consists of the insulin pump (IP) (average number of years using the IP was 7 years) and the continuous glucose monitoring system (CGMS) (average number of years wearing this device was 3.5 years). The CGMS has come a long way and can now display glucose levels via smart phone technology and alert parents when children’s glucose levels are getting low or too high. Glucose levels in our group varied between 57 and 525 mg/dL with an average of 177 mg/dL (average glycated hemoglobin (HbA1c) percentage was 7.7%).
A unique facet for the children at ‘Friends for life’ is that they are surrounded by other children with diabetes, all while playing and visiting theme parks, and literally becoming “Friends for Life”. They are able to share their experiences, fears, and success stories through the years via various social media platforms. We found that this interaction helps them a great deal in adhering to daily regimens that help ensure good control of T1D. The children with diabetes are never alone to face their condition and parents can connect with other parents that may have similar challenges (children undergoing puberty, children leaving home for college, etc).
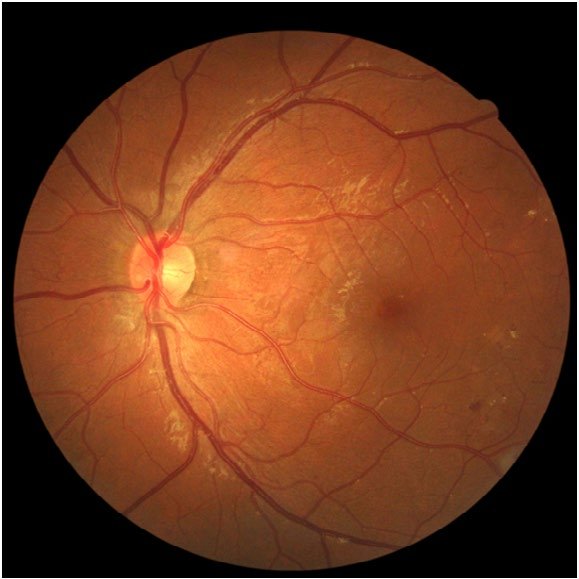
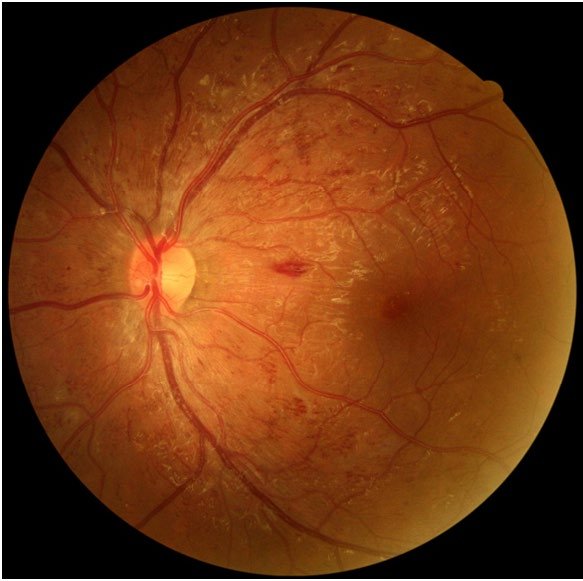
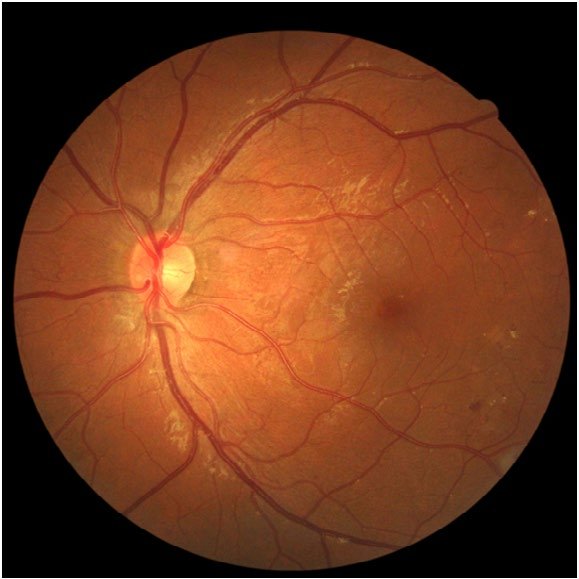
One notable case involved an adolescent whom we had followed up for 5 years and who had all his blood glucose numbers well under control for diabetes.1 Suddenly, he decided (at 19 years old) to no longer follow a good control regimen for his T1D. We did not see him at CWD that year and the following year he reluctantly returned (parental pressure) and underwent a screening. His only complaint at the time was that his feet were hurting (likely due to diabetic neuropathy) and that he found it difficult to walk. He requested a handicap parking tag that we did not facilitate for him! When checking his visual acuity, he had dropped one line of vision from previous visits, his blood pressure was 145/95 mmHg, and his HbA1c was >14% (glucose level was 525 mg/dL). Previous retinal examinations had shown healthy retinas. At the time of his visit in 2015, the 22-year-old subject had a combination of 440 blot and flame hemorrhages between the right and left eye (Figure 2) as well as intraretinal microvascular anomalies (IRMAs). OCT imaging showed very early signs of macular edema, while OCTA findings showed an intact foveal net (foveal avascular zone (FAZ)). After an intense 90-minute consultation with our subject and his family, we were able to convince him to resume use of his incontinentia pigmenti (IP). Within 8 months we succeeded in bringing down his HbA1c to 8.1% (from >14% and his blood pressure to 110/75 mmHg (controlled medication). Eight months after returning to a controlled regimen (in 2016), the subject1,2 had only 2 small blot hemorrhages, no IRMAs, and no flame hemorrhages (Figure 3) and his feet no longer hurt.
Figure 2: Forty-five degree field of view of the left retina captured in non-mydriatic mode in july 2015 (left eye).
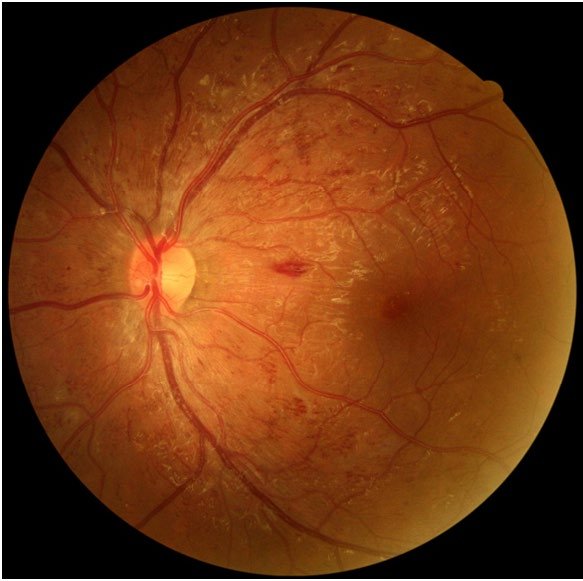
Figure 3: Forty-five degree field of view of the left retina captured in non-mydriatic mode in July 2016 (left eye).
 The beneficial effect of well-controlled T1D cannot be stressed enough, as these individuals face the likelihood of living a fulfilling life over the course of many decades. The value of having a group such as CWD where children and adults with T1D can live in close kinship, connected through social media, cannot be overemphasized. This is as important as their individual health statistics; the availability of a group support for the hundreds of children that live everyday with diabetes makes all the difference in the world while we all await the release of the artificial pancreas.
The beneficial effect of well-controlled T1D cannot be stressed enough, as these individuals face the likelihood of living a fulfilling life over the course of many decades. The value of having a group such as CWD where children and adults with T1D can live in close kinship, connected through social media, cannot be overemphasized. This is as important as their individual health statistics; the availability of a group support for the hundreds of children that live everyday with diabetes makes all the difference in the world while we all await the release of the artificial pancreas.
ACKNOWLEDGEMENTS
CWD 2016 team: Rob Freund, RN, Sarah Melendez, RN, Kimball Dunlap, RN, Belinda Peach, Stephanie Lambert, Paula Fairchild, Doris Chong, D. Smith, B. Schmidt, J. Lopez, Donna Cope, Robert Cope, Scott Kyllo, Laura Billetdeaux, and Jeff Hitchcock. As well as manufacturers Optovue Corporation, CA, USA as well as Canon USA Inc., NY, USA.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.


 The beneficial effect of well-controlled T1D cannot be stressed enough, as these individuals face the likelihood of living a fulfilling life over the course of many decades. The value of having a group such as CWD where children and adults with T1D can live in close kinship, connected through social media, cannot be overemphasized. This is as important as their individual health statistics; the availability of a group support for the hundreds of children that live everyday with diabetes makes all the difference in the world while we all await the release of the artificial pancreas.
The beneficial effect of well-controlled T1D cannot be stressed enough, as these individuals face the likelihood of living a fulfilling life over the course of many decades. The value of having a group such as CWD where children and adults with T1D can live in close kinship, connected through social media, cannot be overemphasized. This is as important as their individual health statistics; the availability of a group support for the hundreds of children that live everyday with diabetes makes all the difference in the world while we all await the release of the artificial pancreas.



