INTRODUCTION
Diffuse idiopathic skeletal hyperostosis is an ossifying disorder characterized by spinal and peripheral neuropathy. Forestier and Rotes Querol were the first two who discovered this disease and presented it as senile ankylosing hyperostosis of the spine by the name of Forestier Disease in 1950.1 They described it as an idiopathic disorder causing ossification in the anterior cervical spinal ligaments with its progression and eventual encroachment on adjacent structures. Since then many different terms other than Forestier Disease were used to describe this condition. These included ankylosing spondylosis, spondylosis deformans and ankylosing hyperostosis. Later in 1975 this pathology was designated by Resnick et al as Diffuse Idiopathic Skeletal Hyperostosis or DISH.2 They proposed the Resnick criteria as a flowing ossification at the anterolateral aspect of four contiguous vertebral bodies, a preserved disc height, and an absence of the degeneration or sclerosis of the corresponding apophyseal joint.3 Today, DISH is used for the more generalized form of the disease involving axial and extra-spinal ligaments, while Forestier’s syndrome is used to describe the cervical manifestation of this condition.
Based on radiological surveys of the cervical spine 2.4- 5.4% of individuals above 50 years of age have Forestier’s disease. The majority of patients with this condition will remain asymptomatic throughout their lives.4
DISH is not an uncommon disorder and a 12% incidence was discovered during random autopsies within a Veterans Administration Hospital population.3 Reports have shown an increase of 28% of the DISH in the elderly.5-8 The most common extra-spinal clinical manifestation of this disease presents as dysphagia followed by respiratory disturbances such as, dyspnea, sleep apnea, stridor and dysphonia.9-15
Infrequently, a concomitant association of swallowing difficulty and upper airway obstruction might be seen in a patient with DISH.16-21 This study reports two DISH cases observed in middle age men with a chief complaint of an increasing-intensity dysphagia over the past year. In both cases the dysphagia became more profound within recent months. Radiographies, reformatted CT scans, and a barium swallow confirmed the esophageal impingement by several large contiguous osteophytes considering voluminous at the C3-C5 levels.
CASES
Case 1
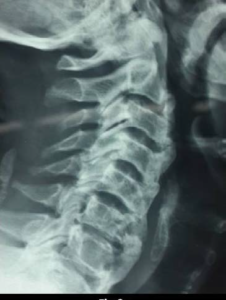
A 54-year-old man was admitted to our clinic with progressive dysphagia involving solid foods for one year that had become more pronounced within the last three months. He also described a limited neck motion over the past three years. Clinical examination confirmed the neck motion limitations while the neurological exam was found to be normal. Lateral cervical plain radiographs showed extensive ossification along the anterior aspect of the cervical spine from C2-C7 which was more prominent at C4-C5 with a ossification breakage at C3-C4 (Figure 1a). Sacroiliac joints were found to be normal. Barium swallow showed an esophageal impingement at the center causing a bifurcation of the esophagus into two lumens (Figure 1b). Cervical MRI was negative for any intra-canal pathology. The patient then underwent surgery under generalized anesthesia.
Figure 1. Lateral Cervical Radiograph Shows the Bridging Osteophytes from C2 to C6, note a Break at C3-C4

Figure 1b. Barium Swallow in AP View: Demonstrates Bifurcation of Barium Indicating the Marked Compression in the Midline

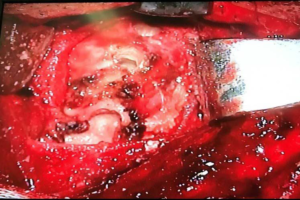
A left-sided longitudinal incision along the medial border of the sternocleidomastoid was made in a corridor between the esophagotracheal complex medially and the carotid jugular bundle laterally. The anterior aspect of the cervical spine was exposed, the prevertebral aponeurosis was incised, and the longus coli were appropriately retracted. (The candle flowing ossification was demonstrated as prominences of different sizes) (Figure 1c). Then, the osteophytes were marked and removed from C2-C7 utilizing an air drill (Figure 1d). The post-operative course was uneventful and the patient felt quite better during the follow-up encounter. A postoperative cervical X-ray revealed the clearance of the cervical spine from the osteophytes (Figure 1e). The patient made good recovery and is symptom free at 6-months follow-up.
Figure 1c. Intraoperative View Showing the Osteophytes
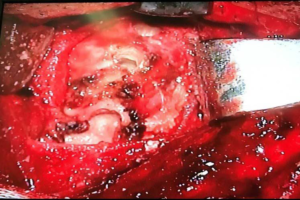
Figure 1d. Intraoperative Fluoroscopy

Figure 1e. Post-operative Lateral Cervical Radiograph: Showing Complete Resection of the Osteophytes

Case 2
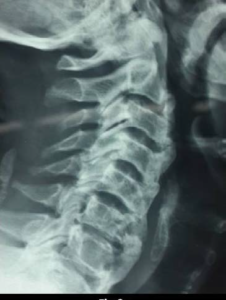
A 62-year-old man was admitted to our clinic with a chief complaint of dysphagia involving solid foods which had increased in intensity over the last 2 months. The patient also reported a history of neck stiffness. In the last one year he has also history of several attacks of left upper arm radiculopathy. Radiological survey of his cervical spine revealed an ossification of the anterior longitudinal ligament with the formation of large osteophytes from C2-C7 with elongated spiky spurs at C3-C4 and C6-C7. It also showed posterior osteophytes at C6-C7 (Figure 2a). A broken bridge of flowing osteophytes was also discovered at the C2-C3 level.
Figure 2a. Lateral Cervical Radiograph of the Second Case: Showing a Brided Cervical Spine with Osteophytes from C2 to C&, Note Posterior Osteophytes at C6-C7 Level (Arrow).
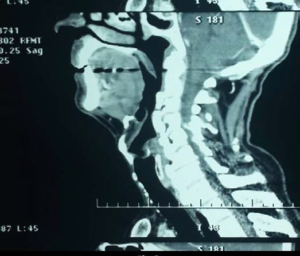
This pathology was confirmed by a diagnosis of DISH and through using reconstructed sagittal CT scans (Figure 2b). Cervical MRI was negative for OPLL and OLF, but showed a hard disc at C6-C7 level along with anteriorly developed osteophytes formation from C2 to C7 (Figure 2c). Barium swallow revealed the anterior displacement and blockage of the esophagus due to the enlarged osteophytes (Figure 2d). Under general anesthesia surgical access to the cervical spine was made through the left-sided standard anterolateral approach. After exposure of the anterior aspect of the cervical spine from C2-C7, the corresponding prominent osteophytes from C2-C7 were excised through the employment of a high-speed drill (Figure 2e). In the following step, the C6-C7 hard disc was removed utilizing subsequent interbody fusion with a cage. The patient had no post-operative complaints and his dysphagia was relieved completely within a month Postoperative X-rays during a 2-year follow-up showed no evidence of osteophyte recurrence (Figure 2f).
Figure 2b. Sagittal T2 Weighted MRI which Demonstrate Anterior Osteophytes and a Hard Disc at C6-C7 Level (Arrow)

Figure 2c. Reconstructed CT Images Showing the Brigded Made of Osteophytes
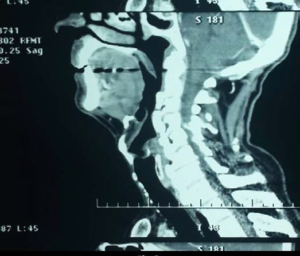
Figure 2d. Barium Swallow Shows Sever Obstruction from C4 to C7

Figure 2e. Intraoperative Fluoroscopy

Figure 2f. Post-operative Lateral Cervical Radiograph Demonstrating Resection of the Osteophytes as well as ACDF at C6C7 Level

At 2-year follow-up he experienced neither dysphagia nor brachialgia.
DISCUSSION
DISH is a non-inflammatory disorder with an unknown etiology which occurs among the elderly. In most cases the patients are male. It is a well-defined syndrome with the axial and peripheral manifestations of hyperostosis.2,9-15 The male: female ratio is 2:1
The etiology and pathogenesis of this syndrome are unknown. However, a wide range of factors have been considered in the development of this disease. The condition has potential associations with obesity, glucose intolerance, diabetes type II, hyperinsulinemia, hyperuricemia, dyslipidemia, hypervitaminosis A, as well as a high social status.22,23
DISH is often manifested as back pain and associated with a limited range of spinal motion; particularly of the neck. The cervical spine is affected in more than 75% of cases involving DISH.24-26 In such instances, besides experiencing neck stiffness, extensively enlarged osteophytes can result in a marked compression of anteriorly located anatomical structures.9-15,24-26 Compression of these structures may cause globus, dysphagia, aspiration, hoarseness, stridor, dyspnea, and sleep apnea of varying intensities within the patients with progressive DISH. Neurological deficits are rare in this disease and it occurs only when ossification of the posterior longitudinal ligament (OPLL) coexists.24-26
One of the most interesting features of DISH is dysphagia. According to Verllan, 204 cases of DISH induced dysphagia had been reported until 2011.18 Swallowing disorder is caused through the variety of mechanisms. With respect to direct compression, osteophytes below C4 can cause moderate to severe dysphagia as a result of direct impingement of the esophagus.9-11,27-29 The inflammatory reaction of the esophagus, fibrosis due to chronic irritation, and crico-pharyngeal spasm, are other known mechanisms of swallowing disorders involving DISH.9-11,27- 29 Therefore DISH, with the presence of prominent osteophytes below C4, should be regarded as a well-known cause of dysphagia; particular within the elderly.9-11,27-29 The most frequent level of involvement related to dysphagia is at C5-C6 followed by the C4-C5 levels.
Above C4, the vertebral bodies are in touch with the pharynx where large osteophytes through C2-C4 may result in dysphagia as well as dyspnea.12-15,30,31 In such instances, the patient initially complains of the sensation of a retropharyngeal foreign body or globus, which can later become a true dysphagia. Enlarged bony spikes at C3-C4 may also cause food aspiration due to the subsequent deviation of the epiglottis.30-31 The C2-C3 level is the least commonly associated level with regards to dysphagia Most of these disturbances may be aggravated through the extension of the neck as well as with ameliorate through its flexion. Difficulty during swallowing may persist even with flexion of the neck. This occurrence is due to fibrosis of the esophageal wall.
Respiratory discomfort is another feature of DISH. Ef fort dyspnea, dyspnea during sleep, stridor, continuous snoring, sore throat, a constant urge to clear the throat, and sleep apnea are the various patterns of respiratory distress manifested with this condition. In the majority of cases with respiratory distress, the offending osteophyte is located at the C3-C4 level.12-15,30,31 DISH respiratory distress is regarded to be secondary to a partial obstruction of the upper airway corridor subsequent to a combination of direct extrinsic compressions from the osteophytes as well as an internal compromise from a reactive intrinsic inflammation above the level of C4.
Combinations of dysphagia and respiratory distress are observed less frequently and it may be due to the excessive ossifications or more extensive compressions that develop.32-39 If the corresponding osteophyte is larger on one side it may result in a distortion of the upper aero-digestive corridors with an accompanying aggravation of the preexisting symptoms.32-39 Respiratory discomfort develops in a faster and more prominent fashion when a distortion is present32 Retrocricoid inflammation may also induce laryngeal edema, dysphonia, vocal cord immobility, and stridor.30-39
With an impingement of the esophagus, it is rare to observe the concomitant compression of the recurrent laryngeal nerve on the left side that is secondary to spiky spur formations. This too may cause vocal cord paralysis.16,39 In all, there is a direct relationship between swallowing pathology and respiratory distress when comparing the size of osteophytes. Usually with an osteophyte that is larger than 10 mm, the possibility of the above-mentioned complaints more frequent.
The utilization of plain radiographs is necessary to establish a proper diagnosis of DISH. The diagnostic criteria for DISH are appropriately outlined as an ossification within the anterior longitudinal ligaments of at least four continuous vertebral bodies, preservation of disc space height, absence of degenerative changes, normal apophyseal joints (which lack degenerative changes); and the absence of sacroiliac joint sclerosis.40-44
Axial and reconstructed sagittal CT images can measure the true size of the osteophytes and demonstrate the side of projection more precisely.40,41 The actual distance between the osteophytes and the pharyngolaryngeal tract, as well as the layers of incomplete ossification, can be properly demonstrated in reformatted sagittal CT imaging. A cervical MRI is necessary for the detection of intra-canal pathologies such as ossified posterior longitudinal ligament (OPLL), retro-odontoid pseudotumors, and the ossification of the ligamentum flavum (OLF).42-43
Besides plain radiographs, impingement of the aerodigestive tract can also be demonstrated through the use of a Barium Swallow. In Barium Swallow, the constricted tract is located over the anterior aspect of the largest osteophytes.9-11, 27-29, 32 This finding may infrequently present far from the bony ridges. In such cases, when anterior to the osteophytes, there may be several layers of incomplete ossification that are hardly visible within plain radiographs. Furthermore, the intrinsic inflammation that is anterior to these layers will result in a significant aero-digestive tract compromise.
Esophagoscopy is important to rule out pathologies causing intrinsic compressions. This procedure can be done with flexible endoscopy but must be performed very carefully due to the risk of esophageal perforation.45,46 Infrequently, the procedure might remain incomplete due to the difficulty of passing the scope.
Evaluation of swallowing with the use of videofluoroscopy allows a definite diagnosis of dysphagia. Doing so will clearly show the features of an extrinsic compressive effect on the esophagus.
A similar clinical condition with radiographic changes that also results in dysphagia and dyspnea are hypertrophic anterior cervical osteophytes. (HACO). In this condition, the epiphyseal joints are affected and the discs space heights are narrowed due to cervical spondylosis. Other disorders included within the differential diagnosis must include; oropharyngeal tumors, retropharyngeal abscesses, esophageal tumors, esophageal stricture, Zenker’s diverticulum, motility disorders, Plummer-Vincent’s syndrome and other cervical mass lesions.
Generally, treatment of DISH or HACO is only indicated when these become starkly symptomatic and will begin with conservative treatment approaches. A well-balanced diet and NSAIDs are highly useful for managing the swallowing problems in elderly patients with major comorbidities. Dietician assistance with consumption modifications based on the patient’s required caloric intake should be implemented also. Such modifications often include consumables which are mixed, soft, or semi-liquefied food staples. However, when the general health of the patient is considered too precarious, feeding with percutaneous endoscopic gastrostomy (PEG) should be considered.
Anesthesia may be difficult in the patients with DISH.47,48 In cases involving moderately sized osteophytes, fiberoptic-assisted intubation may prove to be beneficial. This particular procedure is often far more difficult with larger osteophytes.47,48 In those with marked dyspnea, an association with lessened dysphagia involving a preoperative tracheostomy before the induction of general anesthesia may be advised.32
The optimal therapeutic strategy for middle-age patients and the elderly (without comorbidities), who suffer from dysphagia, dyspnea, or both, is the surgical removal of the osteophytes.49,50 The anterolateral surgical approach with a longitudinal incision along the anterior border of the sternocleidomastoid muscle is recommended for osteophytes existing below the level of C2.32,49,50
The side of approach is up to the surgeon. The exception is when the osteophytes are more prominent on one side, which eventually dictates the side of incision. By creating a long incision and with adequate exposure, the osteophytes can be excised. The preferred tool will be a high-speed cutting burr.32,49,50 The surgeon can then smooth the site of pathology with a high-speed diamond match stick. In the case of radiculopathy or myelopathy due to a single level osteophytes, concomitant discectomy and fusion might become necessary.
Surgical complications are infrequent and include laryngeal paralysis, stroke, Horner syndrome, and cervical instability.51
Surgery can eliminate the symptoms caused by the compressive effects of osteophytes except in those who develop irreversible conditions. In fact, 70% of reported cases of dysphagia disappear shortly after resection. But in the remaining 30%, it may take several months to obtain the same level of improvement.52 Early resolution of the symptoms is due to the elimination of the mechanical obstruction of the esophagus. A slower resolution could be due to the more gradual recovery from peri-esophageal inflammation.52 Therefore, the outcome for dysphagia is rather positive; except in those with a longstanding history involving fibrosis which has replaced the original inflammation.51,52
Re-ossification with new osteophyte formations may occur after the successful initial surgical resection.53,54 An average rate of 1 mm/year of the radiological reappearance of DISH with new osteophyte formations has been reported.53,54 Therefore, it is possible that the previously excised osteophytes will again reach their preoperative size 14 to 20 years following surgery. Recurrence has been found to occur mostly at the site of broken bride and in mobile segments rather than within the segments without mobility. Hopefully, most patients with such recurrence will remain asymptomatic and surgery will only be indicated when dysphagia occurs and the upper airway becomes compromised.53,54 Prevention with non-steroidal anti-inflammatory drugs, biophosphonates, and low dose radiotherapy still remains questionable.
In summary, swallowing difficulty and most of upper airway malfunctions secondary to DISH are treatable conditions and they usually ameliorate with the careful excision of osteophytes. A responsible physician should keep this clinical entity within the differential diagnosis of dysphagia and upper respiratory dysfunctions.
ACKNOWLEDGEMENT
The authors appreciate the efforts of Miss Mona Karimi,the secretary of R&D section of our institute and Mr. Alireza Mojtahed for their great assistance
COMPETING INTERESTS
Written consent was obtained from the patients by the authors to reproduce information and photographs appearing in this article.
The authors have no conflict of interest to declare.
Authors confirm that the submitted article is Neither under consideration nor published previously.