INTRODUCTION
As the medical term suggests, Adhesive capsulitis condition occurs when the shoulder capsule becomes inflamed (capsulitis) and this inflammation in turn causes bands of sticky connective tissue (adhesions) to develop between the joint’s surfaces, the shoulder becomes painful to move, and movement is often completely restricted. It occurs in 2-5% of the general population, with an incidence rate of 2.4 per 1000 years. Women are affected more frequently, in the fourth or sixth decade of life with a peak incidence in the age range of 50-55 years. The non-dominant arm is more likely to be involved.1
The usual diagnosis (and often misdiagnosis) for shoulder issues, is arthritis, rotator tear, adhesive capsulitis (frozen shoulder), bicipital tendinitis and bursitis. There may be true structural damage to the joint; however, trigger points are very often the true cause of the pain. Trigger point will always cause the involved muscle(s) to be weak and easily fatigued, prohibiting the involved muscles from building mass. It is found that about 95% of patients, who suffer from shoulder issues, also have trigger points in the supraspinatus, infraspinatus, teres minor and subscapularis (the SITS muscles) stabilizers; levator scapulae, rhomboids, pectoralis minor, trapezius, and serratus anterior.2
Trigger points develop within muscle sarcomeres. Sarcomeres are the basic building blocks of muscles consisting of actin and myosin myofilaments; muscles move when these myofilaments slide over one another. Trigger points develop when this process becomes attenuated and the sarcomeres becomes overactive; the actin and myosin myofilaments stop sliding over one another. As a result, the sarcomere becomes turned to the permanently ‘switched-on’ position leading to a state of contraction which leads to muscle hypertonia, weakness, shortening, and fibrosis (muscle stiffness).3
Methods of treating trigger points include electrotherapy modalities namely (transcutaneous electrical nerve stimulation, ultrasound, low-level laser therapy, electromyography), local anesthetics (Botulinum toxin injection, dry needling), manual therapies (spray and stretch technique, deep pressure massage, mechanical vibration, ischaemic compression), muscle biopsy, thermotherapy, manipulative therapies and magnet therapies.4,5
Treating the trigger point by ischemic compression involves applying sustained pressure to the trigger point with sufficient force and for long enough to slow down the blood supply the pressure is gradually applied, maintained, and then gradually released. It is held as long as 60 seconds.6 By myofascial release method, in which both hands are crossed and heels of hands are kept transversely across the top of the tissue with some compressive force, and force is applied with the heels of palm in the cross direction equally for 30 seconds and repeated for 3 times.7 Frictional massage in parallel direction to fiber orientation for 5-10 minutes ‘frees up’ scar tissue within a trigger point, allowing muscle fibers to move more normally, increasing blood flow through the tissue and decreasing nerve sensitivity,8 followed by ice massage with ice cubes for 10-15 minutes is particularly useful in treating pain in small areas irritated by trigger points in muscle, tendon or bursa and should precede massage and stretching programs to cause pain relief.9
The study will investigate whether physical therapy techniques to inactivate myofascial trigger points (MTrPs) can reduce symptoms and improve shoulder and neck function in daily activities in population of chronic periarthiris shoulder patients.
MATERIALS AND METHODS
All 10 eligible patients both male and female were informed about the study; consent was taken from the willingly participating patients. Baseline assessments were performed which included a range of motion of neck and shoulder outcome measures of pain intensity on visual analogue scale (VAS) and neck disability index (NDI) were recorded. The study was conducted in a busy Physiotherapy Clinic in Ludhiana, Punjab, India. Data were collected on day 0 and day 14 and statistically analyzed and results were obtained and comparisons were made between day 0 and day 14 on included patients.
Treatment starting with inactivation of the active myofascial trigger points by manual techniques employing compression technique combined with the intermittent cold application by using ice-cubes followed by myofascial release, friction massage and stretching the muscle daily for 2 weeks with follow-up on 14th day was given.
RESULTS
This study showed that the values on paired t-test were significant and relevant in statistical and data analysis on 5% level of significance. So there is an increase in neck flexion and neck extension and a decrease in NDIS and pain on VAS.
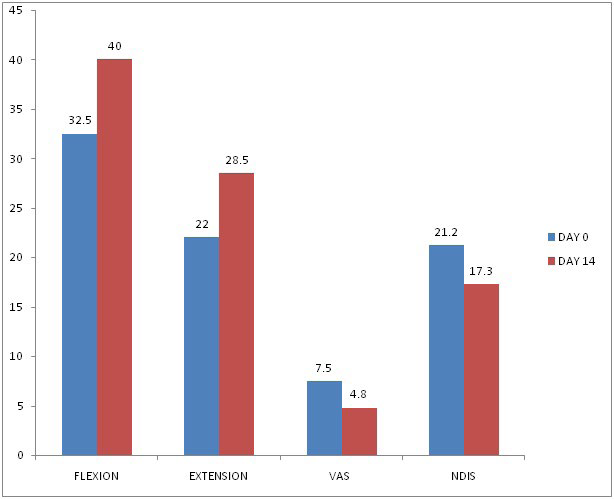
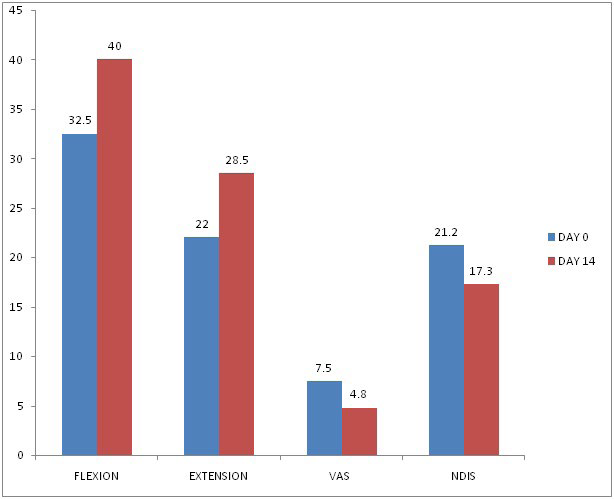
This study shows the effectiveness of a comprehensive MTrP therapy program in patients with shoulder pain. NDIs questionnaire score was smaller than expected on the basis of results from other studies. With a smaller mean value, observation of great differences between baseline and follow-up at 14 is less likely. The number of patients who improved in this study as seen on reduction in VAS and NDIS is a clinically relevant result (Table 1 and Figure 1).
| Table 1. Average Values of Range of Motion of Cervical Flexion and Extension, Pain on VAS and NDIS at Day 0 (Pre Treatment) and Day 14 Day (After Treatment) |
|
Days
|
Cervical Flexion |
Cervical Extension |
VAS |
NDIS
|
|
Day 0
|
32.5 |
22 |
7.5 |
21.2 |
| Day 14 |
40 |
28.5 |
4.8 |
17.3
|
Figure 1. Values of Range of Motion of Cervical Flexion and Extension, Pain on VAS and NDIS at Day 0 (Pre Treatment) and Day 14 Day (After Treatment)
DISCUSSION
Halkovich et al analyzed the effectiveness of the spray and stretch technique, versus passive stretch, in 30 normal volunteers. In that study the authors reported this study patients who received spray and stretch technique had a greater improvement in the Read Only Memory (ROM) than patients who received passive stretch alone.10
The intervention group showed a significant improvement on the shoulder pain and dysfunction and NDIS.
Hains et al reported the effectiveness of ischemic compression therapy of MTrPs in shoulder muscles in patients with chronic shoulder conditions compared with sham compression. The intervention group underwent 14 day sessions of therapy (comprising 60-second ischemic compression of MTrPs, myofascial release, frictional massage and cryotherapy in trapezius muscle regularly without any other therapeutic measures.11
The current study has shown that a decrease in active MTrPs is a better outcome. Thus, this study shows the effectiveness of a comprehensive MTrP therapy program in patients with shoulder pain. NDIS questionnaire score was smaller than expected on the basis of results from other studies. With a smaller mean value, observation of great differences between baseline and follow-up at 14 is less likely. The number of patients who improved in this study as seen on reduction in VAS and NDIS is a clinically relevant result.
CONCLUSION
This study evaluated the effectiveness of a 14 day comprehensive MTrP physical therapy treatment program in patients with chronic, nontraumatic, unilateral shoulder pain and associated neck disability and restricted cervical and shoulder ROM.
CLINICAL SIGNIFICANCE
There was an increase in neck flexion and neck extension and decrease in NDIS and pain on VAS. Myofascial trigger point release is effective in treating neck disability and increasing range of motion.
FUTURE SCOPE OF STUDY
There is a need for further research with adequate sample size and comparable with equal distribution may be taken off over sufficient duration to arrive at quality and better results by taking more variables and more conditions and within the same age group and sex. The management of MTrPs is not restricted to MTrP inactivation, but it requires correction of perpetuating factors that are clinically apparent but not yet necessarily scientifically established.
CONFLICTS OF INTEREST
None of the authors have any conflicts of interest.