INTRODUCTION
The exponential growth of technology is both exciting – making new things possible, faster, easier and accessible – and overwhelming in terms of communication, entertainment, and health care.1 In health care, the therapeutic relationship, engagement and communication of participants is key for effective treatment. This is particularly the case for in-person mental or behavioral health, as well as via telepsychiatry (i.e., video; TP), telebehavioral health (TBH) and other technologies. Compared to in-person care, TP and TBH appear equal or better.2 Outside of health care, engagement is key in entertainment such as computer games, which have replaced many in-person recreational activities. Indeed, generations X, Millenial/Y and Z have grown up with technology (i.e., text, e-mail, Twitter, social media; Facebook in 2017 had 1.37 billion daily active users).3-4 As of 2017, 95% of adults in the U.S. have a cell phone and 77% have a smartphone,4 to socialize/interact with others and accomplish tasks.5
The interface between technology (i.e., a system) and the participants is of great interest in psychiatry, psychology and other behavioral sciences.6 Technology may change the nature of interaction for participants, who may be an individual/group, people/ patients and virtual characters. Technology may affect communication, usually defined as an exchange of information, thoughts and feelings among people using speech or other means, with clarity, responsiveness and comfort.7 TP (i.e., two-way synchronous video) and other technologies on a spectrum are used to simulate real-time experiences related to feelings, perception, images, and interaction.8 Engagement may also be affected by technology, but even low-cost TP and TBH systems facilitate a “social presence” for participants to share a virtual space, get to know one another and to discuss complex issues.9-10 Engagement in health care is defined as “the strengths-based process through which individuals with mental health conditions form a healing connection with people that support their recovery and wellness within the context of family, culture, and community…[part of the] therapeutic alliance”.11
TP is part of a much larger technology world, which includes virtual environments (VE), virtual reality (VR), augmented reality (AR), immersive VR (IVR) and computer-mediated communication (CMC). How the participants experience the technology system/others, that is if they feel present (i.e., telepresence (TPr), affects their response to it/others and accordingly, how they feel/ think. After starting with phobia and cognitive rehabilitation in the 1990s,12 research has spread across fields such as social neuroscience,13 neuroscience,14 the military (e.g., Army),15 communication,1 computer science,16 tourism,17 robotics,18 artificial intelligence,19 virtual clinical interviewing 20 and mental health care.6,21 The specificity of context, ecological validity and ability to evaluate longitudinally open up tremendous opportunities for research.12
The goal of this concept paper is to understand how psychiatric and behavioral health care are affected by TP by learning about TPr, VR, and AR. The paper provides a brief overview of the scientific literature related to the development and experience of the therapeutic relationship, in general, as well as how technology affects it, engagement and communication. More specifically, this paper will help the reader to:
1. Review the basic concepts of therapeutic relationships, engagement and communication in the context of in-person care.
2. Review TP and TBH compared to in-person care, in terms of how technology affects the therapeutic relationship, communication and engagement, and
3. Explore research findings from TPr, VR, and AR that may apply to the clinical therapeutic relationship, engagement and communication.
METHODS
The goal of this concept paper is to help clinicians, teachers and researchers consider the intersection of the following three topics: 1) the therapeutic relationship in psychiatric and behavioral health care; 2) how TBH affects the therapeutic relationship, engagement, communication, and boundaries; and 3) research findings on TPr, VR and AR applied to clinical care. Sections two and three are supported by a keyword using single terms combined from concept areas. The philosophical approach to the keyword search was done according to the six-stage process for scoping reviews,22 which are typically undertaken to examine the extent, range and nature of research in a topic area and identify gaps in knowledge rather than to examine more specific, narrow topics, study designs and outcomes as is typically examined in systematic reviews.
A literature search was conducted using the search strategy and keywords process toward the following concept areas23: 1) therapeutic relationship, engagement, communication, boundaries, clinical; 2) telepsychiatry, telemental or telebehavioral health, telepsychology; e-health, video (synchronous, asynchronous); 3) psychotherapy via technology (teletherapy, online therapy, distance counseling, and e-therapy, behavioral telehealth, telepsychotherapy; 4) computer/technology-mediated communication (robot, web-based, apps, text, e-mail, Internet (hybrid, channel, medium, interpersonal, feedback, context, distraction); and 5) telepresence related to technologies (virtual, augmented, reality, environment). The search prioritized references for peer-reviewed journals, evidence-based findings and tested hypothetical approaches.
Searches were done in regular medical and psychology indexes, as well as OTSeeker, ABI/INFORM, Technology Mediated Communications, Arts & Humanities Citation Index, Project Muse, ProQuest Research Library Plus, Sociological Abstracts, Computers & Applied Sciences Complete and IT Source. Two authors (DH, KR) independently, in parallel, screened the search results for potentially relevant studies based on titles and abstracts; then they reviewed the full-text articles for final inclusion based on inclusion/exclusion criteria. Peer-reviewed publications with systematic data collection and analysis, including qualitative and quantitative data of studies targeting participants aged 18 and over, were prioritized. Authors also included those with narratives and other findings relative to integrative discussions of the concepts of interest. Finally, references of the papers and excluded systematic reviews were reviewed, as were books and popular literature, to find sources of information related to the core concepts.
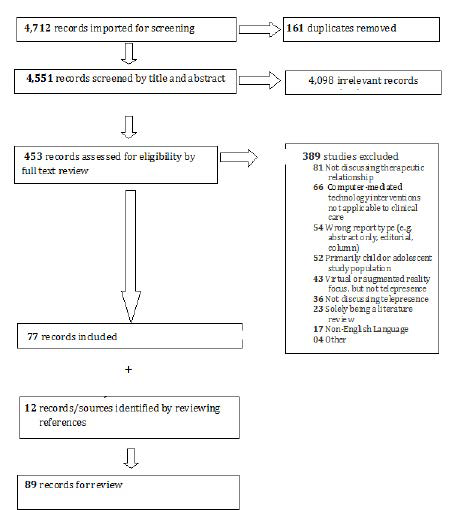
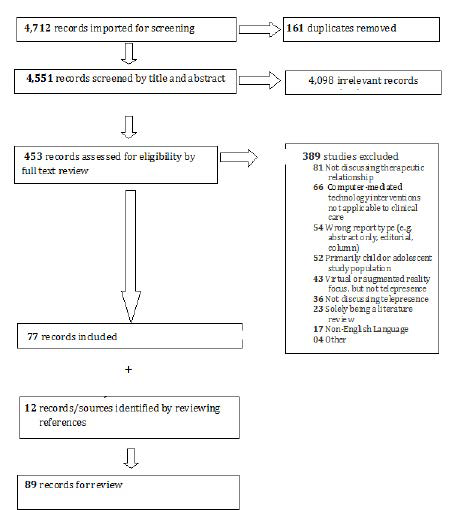
Figure 1 shows that from a total of 4,712 potential references, authors (DH, KR) found 453 eligible for full text review and found 77 papers directly relevant to the concepts. Of the eligible studies, 389 were excluded for: not discussing therapeutic relationship (81); computer-mediated technology interventions not applicable to clinical care (54); being the wrong report type (e.g. abstract only, editorial, column (65); a primary child or adolescent study population/focus (52); a VR or AR focus without TPr (43); (only) incidental TPr focus (36); solely being a literature review (23); non-English Language (17); or other reasons (4). A total of 12 other papers, books and sources of information were found from the methods described above. In the search for integrative discussion of the topics, themes and other areas of interest, disagreements at any stage were resolved through discussion or a third reviewer. Data were extracted from each included paper (or source): hypothesis/methods, concept/synthesis, and evidence of analysis, context, participants and outcomes.
Figure 1. Prisma Diagram of Studies and Other Papers Reviewed
THERAPEUTIC RELATIONSHIP IN PSYCHIATRY, MENTAL AND BEHAVIORAL HEALTH
Clinicians use a variety of models (e.g., biopsychosocial, psychoanalytic, psychodynamic, motivational interviewing, cognitive behavioral) to place a presenting problem in the context of the patient’s life and to understand determinants of identifiable symptoms and their underlying psychopathology. Whether one uses communication technology or not, the clinical process is fundamentally the same. To accomplish this task, the professional needs to hear the patient tell their story in her/his own words. Clinicians use behavioral health skills like listening, questioning, exploring seminal issues, identifying contradictions and using reflection to clarify problems and prioritize core values.24 The traditional psychodynamic case formulation focuses on central conflicts, anticipates problems and helps guide treatment.25 A bio-psycho-socio-cultural (BPSC) model has been suggested10 in follow-up to Engel’s biopsychosocial (BPS) model in medicine.26
Stories are well described in their role in healing, conveying abstract meaning (e.g., myths), moving people to change and teaching learners to apply knowledge and learn skills.27 The profound intimacy and a shared experience of storytelling is believed to provide some of the crucial elements of understanding and healing. Stories are also open to interpretation – which foretells the experience of TPr – so clinicians explore the patient’s subjective understanding of the experience by listening without bias and attention to detail, context, history and meaning. For patients and medical learners, neutral understanding of subjective experiences helps by increasing partnership, reducing performance anxiety and improving “diagnosis” of obstacles or performance difficulties. Understanding the patient/learner perspective facilitates partnering to address complex situations.24
Stories are subjective in nature and the meaning is determined by the psychological relationship between participants. Intersubjectivity – a term used in philosophy, psychology, sociology, anthropology, and psychoanalysis28 – suggests that agreement or a shared understanding on a given set of meanings is key for clinical care.29 Similarly, in medicine, outcomes are improved by shared decision-making between team members facing complex situations.30
Early TP and TBH literature began a discussion about TPr that related to in-person and telepsychiatric care.2,8,31 TP is not experienced in a uniform way and behavioral health care is not delivered in a uniform way. Patients vary by personality, disorder, age, culture, language and psychosocial history. Second, healthcare settings differ: primary care and behavioral health clinics; emergency departments; patient, group and nursing homes; shelters; hospices; schools; forensic facilities; correctional facilities; the battlefront; workplaces; public health; and academic centers. Third, services include evaluation, triage, assessment, and direct care/treatment/management, and these vary in terms of intimacy, breadth and scope of interactions.10
THERAPEUTIC RELATIONSHIP, ENGAGEMENT AND COMMUNICATION ISSUES RELATED TO TELEPSYCHIATRY AND TELEBEHAVIORAL HEALTH
Overview
Ultimately, the goal is to create an environment that facilitates therapeutic engagement and emotional wellbeing for all parties.8,32 A TP competency framework proposed clinical skills, teaching methods, and faculty development.33 The domains include clinical care, communication, professionalism, systems-based practice, practice-based learning, knowledge, and technology (skill). The Coalition for Technology in Behavioral Science’s (CTIBS) inter-professional, evidence-based framework for TBH competencies added virtual environment and telepresence, evidence-based and ethical practice and telepractice development domains.32 These were followed by social media34-35 and mobile health36 competency sets, which cover a variety of clinical adaptations.
Therapeutic Relationship
The patient’s requests, needs and preferences are the clinician’s first priority. If technology is used, reflection can help determine how it affects care and when it may be useful (e.g., video, text). Decisions related to the suitability of any specific technology, then, are often optimally made at the beginning of an evaluation as part of the consent process – usually by the patient and clinician – once the latter understands the needs/preferences among available choices.32,37 care may change over time with the addition of new technology (i.e., telephone, text messaging, app), but the therapeutic relationship needs to attend to all legal and ethical mandates for in-person and TP care (e.g., preparing for emergencies by gaining familiarity with the availability of community resources and emergency resources where the patient is located).
The office, a regular appointment duration and a regular schedule are instrumental in creating a positive environment and the therapeutic frame.25,27 The frame is the foundation or structure that promotes security, trust and confidentiality to explore and discuss anything. In-person and TBH care requires a clinical environment that is private, professional and warm – this includes good seating (e.g., ergonomic support), adequate lighting (e.g., for facial illumination), secure/private entries and soundproofing. When considering a medical setting for the originating (i.e., patient) site, it may be helpful to avoid some rooms (i.e., examination table) and to furnish the room to make it warmer and more personal. If a clinician uses more than one site of care (e.g., main, home and/ or part-time offices), the rooms should be professionally similar in design and technical layout. If the room in the home is used for other things, planning ahead is critical to ensure it is clinically conducive (e.g., others not around, avoid interruptions). As with a behavioral health office in a busy primary care clinic, a sign signifying the need for relative quiet, avoiding interruptions and using alternative spaces for transit may help.
The therapeutic relationship and frame also includes all other correspondence and administrative procedures, technically. Good practice planning and preparation allows the clinician to be accessible and responsive (i.e., a way to receive a timely message if a patient calls to say s/he is 10-minutes late); a centralized communication method rather than a phone line that only communicates with the main office is suggested. While both clinicians and patients may enjoy the telehealth’s flexibility regarding settings, all participants should treat the visit as if it is a regular doctor’s office visit and be on time. Also, with regard to scheduling, it may be better to opt out of a possible appointment, or reschedule, rather than try delivering care in a sub-optimal environment (e.g., mobile from a car or even while parked along a road) or from a different office that may be disruptive.
For TP, the clinician chooses technology to maximize presence, with near-optimal fit of visual and audio mediums (e.g., clarity and visibility, camera angle, spacing/centering of images). She/he needs technical proficiency to meet reasonable patient preferences; similarly, adaptation is necessary for non-video engagement (e.g., telephone; asynchronous modalities such as social media, text, and email). If the participant has not used telemedicine or TP before, s/he may feel anxious, distracted due to the equipment and/or self-conscious being seen/seeing others on the screen. The presence of others in the room (e.g., trainees) is typically optional, since it may feel uncomfortable. Many patients may also inquire if the session is being videotaped and clinicians may debunk that idea and/or explicitly discuss that as part of the consent process.
The evidence-base for therapy by TBH is growing. Satisfaction is high and communication is good since new technology has more than adequate bandwidth.2,8 Studies in adults generally involve patients with depression and anxiety – often military populations with posttraumatic stress disorder (PTSD) – and these studies show comparative efficacy of TBH to in-person services. The therapeutic alliance and bond between the patient and clinician is very good according to formal studies and instruments (e.g., Working Alliance Inventory).38-39 One preliminary study on therapeutic alliance and attrition among participants receiving anger management group therapy showed that no significant differences, overall, but a lower alliance with the telegroup leader than those in the in-person format.40 Client/patient ratings of satisfaction with psychotherapeutic interventions and therapeutic alliance in treatment are comparable between TBH and in-person delivery41 and predict a good therapeutic alliance and therapy outcomes.42 In addition, nonverbal cues get lost, which has implications for psychotherapy, in general, and especially for the treatment of patients who have difficulties relying on a secure therapeutic relationship.43 Overall, TBH sometimes is better than in-person care.44
Trust is a key part of the therapeutic relationship and CMC may exacerbate challenges in communicating with truth and trust.45 These communications transcend physical materiality, time, and space, and yet they have a sense of immediacy and interaction that builds “trust” without evidence. Typically, evidence (i.e., causality) is based on proximity, time, perceiving consequences to actions, performance, and corporeality of experience.45-46 The asymmetrical form of CMC limits social negotiation of meaning and provides a sense of control regarding what messages are received and when. Receivers construct meaning from the messages they send/receive and sometimes assume users’ preference and responsibility for truth.47 Social information processing theory48 suggests users make attempts to achieve communication goals, but if cues present obstacles, they adapt behaviors to accomplish the goals (e.g., using emoticons, deeper questions).49 They may not realize ill-intended consequences, though.
A clear consent process may reduce anxiety and allay basic concerns about TP and TBH. This includes challenges due to interruptions due to the location, telephone calls and ambient noise (i.e., loud music, television and traffic). Participants should not be multi-tasking (e.g., talking while driving in traffic, typing a note on the computer, checking e-mail). In many cases, preparing a short video for patient education may help all parties prevent/ minimize interruptions and distractions and give patients permission to inform the clinician of any factors that might be distracting or upsetting. Other subjects include privacy and confidentiality (e.g., cellular phone and email may or may not be secure or private) and emphasize shared decision-making about therapeutic issues (e.g., technology as an impediment, patient education to call the clinician instead of posting suicidal thoughts on social media). A back-up plan that involves other synchronous communication equipment (e.g., telephone) may be necessary to regroup after a faulty video connection.
Therapeutic Engagement
Overall, patient engagement may be viewed on the level of the clinician – the focus of this paper – as well as team, clinic, practice network or health system.50 Patient engagement is defined as the degree to which patients actively participate in care.51 Related to information technology, specifically, the Health Information Management Systems Society posits that technology informs, engages, empowers, partners and supports the patient’s e-community.52 Systems need more patient-facing technologies, support staff for information technology, smooth workflow for clinicians’ and privacy measures. Technology-based patient engagement strategies (e.g., patient portals, risk assessments, decision aids, access to scheduling, texts, social media) are variably used (e.g., 3% texting; 62% social media) and studied despite providing connectivity.53 Video, telephone, tablet, portal, web site and home-specific (e.g., alarm systems, monitoring systems, tracking devices, and sensors) interventions are increasingly common.54 To be effective, systems need participants/groups to actively give input, contribute to implementation and successfully adopt technology initially and long-term.55
As previously discussed, technology may change the nature of our interaction.8 Some populations may be more comfortable with technology: children in general report novelty; those with significant behavior/conduct/chemical dependency issues report less stigmatization; and anxious patients report less anxiety.56 Technology may help people explore, engage and experiment with ideas and involved partners in new ways, and in that sense, it “changes” dynamics or facilitates a different culture, which makes new things possible.6 Still, further, technology may advance, engineer and create completely new material – to truly innovate ideas and practices – in ways that were previously just not conceivable.6 A patient’s perspective is best captured in her/his primary language10 or use of an interpreter,32 though research shows that communication with synchronous video is less problematic than asynchronous communication using English as a second language.57
With video, words and body movement replace in-room behaviors (e.g., handshake). Projecting one’s voice, looking directly into the camera of a moment, and amplifying one’s hand gestures effectively communicate interest and empathy.32 There are some potential telepresence problems inherent to using a video camera for facial contact. Video conferencing transmits a close-up view of each participant’s head and neck. Aberrations in appearance or social propriety can be particularly disconcerting to patients who are forced to tolerate such distractions without being given invitations to comment. The clinician should also strive to make eye contact by looking into the camera, rather than primarily offering the patient a view of the top of his/her head during furtive note taking.
Whether related to technology or not, other distractions need to be minimized. These may include being too far away or too close to the camera, rocking in one’s chair, tapping a pen or fingernails on the desktop, tolerating ambient music or television sound – these may be greatly amplified to the listener/viewer, particularly with sensitive microphones and high resolution screens. Grooming issues may also need attention, such as covering any facial lesions, trimming nose and ear hairs, and cleaning one’s glasses. Depending on lighting, glare from eyeglasses, shiny baldheads and reflective glass from artwork may also be a serious distraction. Other distractions may include people walking by, cars, buses, trains or activities off camera and their associated noises. Similarly, noise from jangly earrings or other hanging jewelry, loud sipping, lip smacking, ice, or gum chewing are to be minimized. Additional portable devices should be turned off and put away unless one of the parties has courteously informed the other that an interruption may occur. If an urgent call occurs, clinicians need to know how to check into whether their microphone/camera are on or off, lest they erroneously assume that they are not being heard/seen when actually, they are.
Communication
Properties of specific digital technologies inevitably shape communication, which depends on the norms of users, the quality of the conversation and the degree of presence allowed by the technology.58 The telephone yields presence at a distance through one sense only, namely sound and its influence on remote perception. The quality of telephony varies in three dimensions: the accuracy with which sound is reproduced, the speed of transmission and the capacity for two-way rather than one-way communication.58 Analog radio transceivers have a delay and with distortion, but conventional landline calls in the same town; those at a distance and/or by cell phone may have delays. TPr is affected by latency (i.e., delay in time), which is negligible with delays of 250-milliseconds, but while noticeable at 2-seconds; communication usually does not break down in either case, though.59
Historically, video conferencing may affect communication and require special effort, but it facilitates social presence, mutual connection and understanding.8-9,60 A longitudinal study of primary care patients – when offered the same mental health clinician – showed no differences in preference or outcomes for TP or in-person care for an initial evaluation and follow-up visits.61 A study and a review of the literature found in-person and TBH outcomes to be similar with outcomes, satisfaction and other measurements.2 Decreased ability to detect non-verbal cues has been reported during video conferencing for patient interviews,62 but as can be expected, audio-only communication increases information exchange while video conferencing increases engagement.9,63
More revealing research with qualitative and quantitative measures has explored conversational flow, finding a shorter duration via in-person at 9-minutes versus 11-minutes with telemedicine. This was attributed to more “small talk”, patient education, psychosocial discussion and other themes.64 It is also one thing for people to talk/feel about a remote space in the same way they talk about local space, compared to doing a task the same way in a remote space,65 which felt “far away”.66 One study compared participation in four ways: 1) audio only, 2) scene-oriented video conferencing; 3) scene-oriented video plus drawing; and 4) faceto-face.65 Results suggested that 30% of the variance in self-reported presence could be accounted for task-specific experiences. Another study compared the experience of TPr of emotionally charged versus emotionally neutral verbal exchanges and found an increased sense of TPr verbal exchanges was connected to stronger emotions.67
Looking at other technologies historically, clinicians noted other factors related to technology used for clinical care. Early theoretical discussions related to text and e-mail communication suggested that a “cuelessness” phenomenon may occur, wherein the participants become more task-focused and produce “depersonalized content”.68-69 Later, some speculated that non-verbal elements of interpersonal communication may change, including eye contact, gestures, posture, fidgeting, nods, grins, smiles, frowns and lip-reading.70 Recently, keyboard characters known as “emoticons” are being used (e.g., facial expressions) to convey the author’s feelings in email or text messaging.71 All of these factors may influence the therapeutic relationship.8
Media differ in the extent to which they enable the transmission of information. This is referred to as “richness” and it is based on four criteria: feedback, multiple cues, language variety and personal focus.72 Oral media are generally believed to be richer than written media, and synchronous media are believed to be richer than asynchronous media. From the business literature, in-person contact is generally considered to be more appropriate and effective than video CMC, though both are satisfactory for exchanging information and getting to know someone.73 However, richness or high social presence media via immersive systems appear more appropriate for negotiating/bargaining, getting to know someone, generating ideas, resolving disagreements, making decisions and exchanging confidential information.74 A study of 19 group- and social presence-based tasks tested the effectiveness high social presence media for exchange of information, interactive discussion, discussion of sensitive/confidential issues, building relationships and trust and making decisions.73 High social presence media appears better than low social media for some things (e.g., clarifying, expressing feelings, discussing sensitive topics, giving feedback, resolving conflicts), but not others (e.g., negotiation, giving orders, building trust, enforcing authority).
There are constraints of asynchronous technologies (e.g., text, email or social media posts) and special effort may be required to create telepresence, as these technologies do not include facial and non-verbal expressions.70-71 Limitations to keyboard characters have been discussed in the literature for over a decade.71,75 Emoticons – paralinguistic cues to convey emotional meaning – are increasingly popular and contribute to a greater social presence and language comprehension, particularly when combined and aligned with the text. Emoticons have drawbacks, too, though, as they may not adequately capture the spirit of a feeling as it would be expressed in person, and negative emotion is sometimes experienced more strongly than intended.
Boundaries, Technology and Clinical Care
Professionals must attend to boundaries similar to in-person care with TP and TBH video, but other technology-mediated options (e.g., email, telephone, text messaging, apps) require more thought.31-32 At a minimum, this means being amenable on reasonable expectations, consistency, triaging concerns (e.g., suicidal thoughts discussed in-person or by telephone, not text) and professional responsiveness (e.g., responding to an email the next day if received after clearly communicated office hours). It also means clarifying communication when terms/symbols have multiple or ambiguous meanings (e.g., sentence/thought fragments, acronyms, and emoticons). Overall, given the complexity of these issues and the potential convergence of distractions and interruptions, clinicians may perform better after obtaining professional training76 to think through the issues with telepresence and competence related to TP and TBH.32
Spontaneity, engagement and other “in-time” communication techniques may have negative consequences in a professional relationship. Patients already struggling with boundaries (i.e., those with personality disorders or traits) or impulsivity may be poor candidates for some technologies. Sudden action could affect boundary, privacy and security issues, though such events may give them an acceptable way to practice improvements. Those patients may need more literal education and clinicians should approach that care with caution. The tendency for people to respond to a text almost before thinking about it could affect boundary, privacy and security issues for any group of patients.36 Hence, clinicians need to encourage reflection and discussion about boundary issues (e.g., texting, searching others’ information online). In addition, they may need to give more literal instructions and selectively use available technology options (e.g., to use text and social media) based on pros/cons.
RESEARCH ON TELEPRESENCE, VIRTUAL REALITY AND AUGMENTED REALITY RELATED TO TP AND TBH
Overview
The evolution of technology in our society goes back some time. Use of the telegraphy was applied to healthcare early in the 1700s and together with the telephone, began to have a significant impact by the 1900s.77 TP started about 1959.2 VR and AR became more common in the 1980s and 90s. Human life and neuroscience shape our experience with technology. There are “good” (i.e., increasing access to patients and the specialists who can treat them; enjoyment, excitement) and/or “bad” (i.e., stress, distraction and neurological development; internet gaming, and addictions) outcomes.78 Technology is also great for training for things that are too difficult and/or dangerous to try in real life or in an office, such as flight training for pilots and space exploration. Publications have discussed negative impact if youth spend too much time on computers with video games and pornography, rather than interacting with peers.79
TPr then – via VE, VR, AR and CMC – may inform our communication, engagement and clinical work when definitions, uses and measures are applied to TBH. TPr is a phenomenon whereby technology creates an experience that allows the user to “feel as if they were present, to give the appearance of being present, or to have an effect at a place other than their true location”.80 VR and AR can serve as a frame or foundation, determining: 1) to which degree the user is separated from the physical world; 2) which stimuli are introduced and how; 3) who and what can be manipulated by artificial intelligence or human control; and 4) what is subjective versus “objective” and quantifiable.80 Telepresence and how it applies to care at a distance is more of an experience rather than knowledge.
Virtual Environment (VE)
VE is defined as a 3D digital space generated by computer technology with digitally recreated simulations of real-world activities, often involving dynamic social and emotionally engaging stimuli.81 A meaningful system for VR results in three dimensions related to the user’s experience – or feeling of being there – otherwise known as TPr. In VEs, input from movements; tracking with data gloves or sensors, pointing/moving options such as using a joystick; and output devices for any sense that allow interaction. Visual options remain critical from low- (e.g., projection and fish-tank), mid- (e.g., head mounted) to high-end (e.g., cave automatic virtual environment (CAVE)) options.
Questions/implications for clinical care:
1. Has a patient been in a VE and if so, what was/was not comfortable about it?
2. Does a patient feel/think/act in the same way in a VE and does learning in a VE transfer to behavior change in the real world?
Virtual Reality (VR)
VR is defined software application that can involve hardware that allows a user to navigate through, and interact with, a VE in very near real time.81 Users perceive, feel and interact in a manner similar to how they would interact in a physical space.13 VR has been used in the treatment of alcohol misuse,83 anxiety,84 autism spectrum disorders,85 eating disorders,86 stress management and posttraumatic stress/phobia, (e.g., VR exposure therapy (VRET)).82,87 The VR industry mainly provides devices for medical, flight simulation and military training, but0 otherwise, game industries are leading the way. Head-mounted mental health applications88 are also being studied.
One type of VR is interactive virtual reality (IVR), which is generally seen as a way to further stimulate the senses by using a higher quality and quantity of stimuli combined with a greater number of interactions. In that sense, IVR may be better at “extracting” the user from the physical world and “inserting” her/him into a synthetic sensory information space that emulates typical real life stimuli.82 Fidelity of the synthetic stimuli – that is, a match between the level of quality and the interactions is key – otherwise, the experience quickly dissipates for the user.89
Questions/implications for clinical care:
3. What has the patient learned about her/himself, their relationships or their world by using technology?
4. Is this learning sustained over time? If yes, which types of VR experiences are more or less conducive to sustained, generalizable learning?
Augmented Reality (AR)
AR is defined as a live direct or indirect view of a physical, real-world environment whose elements are “augmented” by computer-generated or extracted real-world sensory input. Another aspect of technology-based experience is AR, a live direct or indirect view of a physical, real-world environment whose elements are “augmented” by computer-generated or extracted real-world sensory input. Such input can include sound, video, graphics or GPS data. AR existed in the 1970s and 1980s, mostly in the United States Air Force (USAF) and National Aeronautics and Space Administration (NASA).90 The term “augmented reality” was introduced in 1990 by Tom Caudell, while he was working for Boeing on Computer Services Adaptive Neural Systems Research and Development.91 AR advanced significantly with live training involving combat vehicles.92
Questions/implications for clinical care:
5. What is the impact of disconnection, pixelation and other distortion with TP and TBH, and is it as significant as with VR or AR?
6. Are TP and TBH a preferable healthcare option versus in-person care, even though it is not an exact depiction or like being there?
Computer-Mediated Communication (CMC)
CMC refers to asynchronous or real-time human communication with computers (or two or more electronic devices) as tools to exchange text, images, audio, and video. Traditionally, it refers to computer-mediated formats (e.g., instant messaging, email, chat rooms, online forums, social network services), but now includes other forms of text-based interaction such as text messaging. Research on CMC focuses largely on the social effects and is sometimes referred to as “Internet studies”. Basic qualities of CMC are synchronicity, anonymity and the recorded pathway (except for instant messaging, unless one has a message log set up). Users’ interests and motivations for action may be in making an impression, building a relationship and/or deception.45,58
For text-based and instant messaging communication, emoticons have become a popular resource to enrich text-based communication since 1982,93 and they enable better comprehension.94 Studies are in progress to map the brain regions involved in emotional processing related to emoticons.71 Given that they are unnatural, iconic, and static representations of human facial expressions, studies have revealed mixed and concerning trends. While convenient for shorthand reasons, they may not reflect a sentiment accurately. In addition, emoticons may not be an adequate replacement for words, which while often preferred, require greater skill and time to communicate. Finally, users employ emoticons for different reasons, making them imprecise for users speaking different languages or attributing different meanings. This may be particularly true across cultures.
Questions/implications for clinical care:
7. Is there a need for text-based communication? If yes, what are those needs and goals?
8. Is it easier/preferable to talk about problems asynchronously and/or anonymously with a healthcare provider?
9. How might emoticons be effective for some patients and not others?
Telepresence (TPr)
Definitions vary for TPr, VR and AR (Table 1).1,14,16-18,81,95-104 TPr appears to have three components: 1) a personal presence or actually being in the VE; 2) environmental presence, as if acknowledged/affected by the VE; and 3) social presence, as if not being alone and/or being with others.95,105-106 TPr in the context of health care (e.g., TP or TBH) became relevant after some of these terms were defined, as two-way audio and video communication systems came. These systems proved adequate for describing complex ideas and providing a modest sense (or “limited”) TPr. The experience of TPr improved as companies added high definition, specifically designed rooms/units to shape participants in a participatory circle and configured people as life-size and natural. Overall, innovative research in TPr is happening in science, linguistics,65 art and other fields.107
| Table 1. Historical Definitions of Telepresence (TPR), Virtual Reality (VR), and Augmented Reality (AR) |
| Author |
Definition |
Comment(s) |
| TPR |
Witmer & Singer, 1998 95 |
The “sense of being there” in one place or environment (i.e., a virtual environment), even when one is physically situated in another. |
The sense of being in an environment other than one’s real location depends on the level of senses involved also known as immersion. Mediums which may stimulate a person’s senses more allows them to be more immersed in their artificial location leading to greater level of presence. |
| Lombard & Ditton, 1997 1 |
“The perceptual illusion of non-mediation.” |
Perceptual illusion is the continuous sensory input from a media (i.e., computer), which a person fails to acknowledge and interacts/communicates similar to as they would in real life. |
| Buxton, 1991 96 |
“The use of technology to establish a sense of shared presence or space among geographically separated members of a group.” |
|
| VR |
Meehan, 2001 97 |
“Perceiving stimuli as one would perceive stimuli from the corresponding real environment.” |
The perceptual illusion that one may experience – from the medium being used – the affect and cognitive processes of others, which leads to behavior as if in a real environment. |
| Mair, 1999 18 |
The experience of being fully present interactively at a live realworld location remote from one’s own physical location and the ability to experience a remote presence such as a person as physically present and interacting with you. |
Original definition by author: “The experience of being fully present interactively at a live real-world location remote from one’s own physical location.” (This definition was modified and expanded due to emergence and expansion of telepresence robots, so the remote operator and user(s) also the remote user feels present in remote location.) |
| Schultheis & Rizzo, 2001 98 |
“An advanced form of human-computer interface that allows the user to interact with and become immersed in a computer-generated environment in a naturalistic fashion.” |
|
| AR |
Guttentag, 2010 17 |
“The use of a computer-generated 3D environment – called a virtual environment – that one can navigate and possibly interact with, resulting in real-time simulation of one or more of the users five senses.” |
|
| Riva, 1998 14 |
A subjective experience cheating the individual out of the illusion that he/she is there, that this experience is real. |
|
| Pratt et al, 1995 81 |
Virtual reality is an application that, in very near real time, allows user to navigate through, and interact with, a VE. |
|
| Coates, 1992 99 |
Electronic simulations of environments experienced via head mounted eye goggles and wired clothing enabling the end user to interact in realistic three-dimensional situations. |
|
| Milgram et al 1994 100 |
“A form of virtual reality where the participant’s head-mounted display is transparent, allowing a clear view of the real world.” |
|
| Torrejon et al 2013 16 |
Augmented Reality (AR) is a technology that enables users to interact and combine 3D virtual objects with the physical world in real-time applications. |
Unlike virtual reality, augmented reality allows a person to still be present in real time (i.e. Pokémon Go). |
| Hugues et al 2011 101 |
Augmented reality can be described as an interactive visualization system (a head-mounted display, a computer, a game console, a smartphone, or a tablet) allowing the merging of digital contents with the real environment surrounding the user. |
|
| Cawood & Fiala, 2007 102 |
Augmented reality (AR) is the fusion of real and VR, creating an illusion that virtual elements generated by computer are overlapped with real world, in real time. |
|
| Höllerer & Feiner, 2004 103 |
Combine “real and computer-generated information in a real environment, interactively and in real time, and [which align] virtual objects with physical ones.” |
|
| Ludwig & Reimann, 2005 104 |
“Human-computer-interaction, which adds virtual objects to real senses that are provided by a video camera in real time.” |
|
Research on TPr has moved from subjective to objective/physiological measures in response to cues, largely related to complex interventions by VR and IVR.108 Virtual presence was described as the experience of interacting with a computer-mediated or -generated environment,105 others add the specific of being in one environment (there) when physically in another environment (here).95 Still taking it further, one may fail to perceive/acknowledge the existence of a medium in his/her communication environment and/or respond as if it is not there.1 The terms immersion and presence have been separated by defining immersion as “a description of the capabilities of a system”, whereas presence “characterizes the response of participants to the system.”109
Questions/implications for clinical care:
10. Is TP “good enough” in most regards to getting care?
11. How does TPr affect healthcare?
12. What is missing from TP compared to in-person care?
The core areas, components, and themes of the VR, AR and TPr experiences overlap.6 Steps toward outlining the subjective, physiological, and objective measures of TPr have been taken (Table 2),97,109,110,111,112 and not all people have the same experience due to age, generation, culture, learning style, personality, and other factors. The table outlines the approaches, measures and results of these three areas, along with the advantages and disadvantages of each. Research in social neuroscience13 and cognitive neuroscience14 is creating, exploring and testing environments used for learning, engagement and reflection by simulating day-to-day life, social situations with objective stimuli and reactions to unusual stimuli (e.g., disasters, moral dilemmas, stress response).
| Table 2. Measurement of Telepresence: Subjective and Objective Corroborative Measures |
| Types |
Subjective |
Physiological (objective corroboration) |
Behavioral/ Performance (objective corroboration) |
| |
|
– Assess user’s automatic responses without involving participants’ conscious deliberation (Van Baren & Ijsselsteijn, 2004) 110 |
– Assess user’s automatic responses without involving participants’ conscious deliberation (Van Baren and Ijsselsteijn, 2004) 110 |
| Approach |
– Self reporting, conscious, introspective judgment regarding their experience in VE or VR |
“The perceptual illusion of non-mediation.” |
Perceptual illusion is the continuous sensory input from a media (i.e., computer), which a person fails to acknowledge and interacts/communicates similar to as they would in real life. |
| Measures |
– Self-administered questionnaires
– Continuous subjective assessment to monitor any fluctuations of senses
– Interviews
– Qualitative measures
– Psychophysiological measures
– Subjective corroborative measures
– Patients rate their post-immersion experience on a numerical scale |
– Change in heart rate
– Changes in skin conductance/temperature
– Blood pressure
– Respiration rate
– HR response provides best assessment of presence (Meehan et al., 2001)97 |
– Facial expressions
– Reflex responses
– Postural responses (elicited by the moving-video s stimulus and maybe enhanced by vection)
– Social responses (emotions, feelings, mood)
– Sensori-motor responses (locomotion, ocular responses) |
| Test Results |
– Highly reliable
– Highly valid
– Sensitive
– Not objective: exposed to subject bias, but not experimental bias
– High applicability |
– Reliable
– Valid
– multi-level sensitivity
– Objective: minimal subject/experimental bias |
– Less reliable
– Valid
– Sensitive |
| Advantages |
– High face validity, meaning that they appear to measure the intended concept
– Do not interfere with the user’s experience while in the virtual environment
– Questionnaires are cheap
– Easy to administer, analyze and interpret
– More adaptable across different media contexts |
– Continuous measure of different levels of presence
– Relatively free of user bias because they are not under users conscious control
– Relatively free of user experimenter bias |
– Continuous measure of different levels of presence
– Relatively free of user bias because they are not under users conscious control
– Occur spontaneously, and therefore do not disrupt the experience
– Capacity to produce differential levels of response, making it easier to relate them to subjective ratings of presence (Freeman, et al., 1999) |
| Disadvantages |
– Subjective questionnaires are not objective, exposed to subject bias, though no to experimenter bias
– Retrospective; depends on patient memory
– May be biased by prior experience (Freeman, et al., 1999) (overcome by doing continuous assessment)
– Cannot discriminate between presence in a virtual environment and physical reality (Usoh, et al., 2000)112 |
– Affects physiological arousal in general and not presence directly
– Cost of physiological monitoring equipment – Skin conductance and temperature slower to change |
– Experimenter bias who observes and interprets behavior
– Lack generalizability (only applicable to specific environment or content) |
VR, AR and TPr in Other Areas of Medicine and Health Care
Historically, VR and AR arose in the medical literature circa 1995. VR has been used for pain management, rehabilitation, limb “replacement” and (IVR) surgical skill and decision-making training,113 in addition to the mental health areas previously mentioned. Surgery demands psychomotor, cognitive (i.e., automaticity) and inter-professional skills for expertise acquisition and “deliberate” practice.114-115 AR has also been used to locate veins (i.e., a near-infrared vein finder), for virtual X-ray view (based on prior tomography or on real time images from ultrasound and confocal microscopy probes) and laparoscopic liver surgery. The use of VR to training (i.e., 3-D anatomy, simulation) is helpful for safety, effectiveness, standardization, instructional flexibility and cost (AR is less expensive than VR).
Simulation helps with skills, knowledge and attitude development.76 This is particularly true in medicine (e.g., code blue), the military (e.g., medics, individuals and teams). Related to behavioral or mental health, VR and AR exposure therapy (VRET and ARET) allow control over the scenario, safety, variety of stimuli, confidentiality, repetition, and self-training.36,82 Furthermore, the user of an ARET is able to see her/his own body interact with the virtual elements. Furthermore, by embedding the virtual fear element in the real environment and allowing a direct “own-body” perception of that environment, the ecological validity of the scenario is increased.116
DISCUSSION AND CONCLUSIONS
TP and TBH care are similar to in-person care but require additional skills, preparation, and training. Clinicians can apply competency-based techniques with TP and TBH to maximize the therapeutic atmosphere in both physical and virtual environments, as well as to minimize distraction and interruptions. The specific concept of TPr is not frequently discussed, but nonetheless helpful for TP and TBH, as it pushes clinicians to make an effort to create the experience of being in-person while maintaining a private, distraction free and therapeutic environment of care. Careful selection and use of technology may contribute to a positive, inviting environment for engagement, a physical plant that provides stability and optimizing technology/media. Some patients may not be a good fit for many technology options, which already challenge boundaries, privacy, and other demands. Clinicians should approach that care with caution, as such patients already require significant time and energy.
Aside from simulation exercises to build clinical skills, VR, AR and other such technologies can inform clinical care. The use of VR and other technologies for training is increasing, due to its efficiency, low cost and flexibility in meeting learner needs via context-relevant “structural” VR environments (e.g. combat scenes, homes, classrooms, offices, markets).76,117 Virtual standardized patients (VSPs) and populating these environments with virtual human (VH) representations can engage human users in believable and/or useful interactions. Since an integral part of medical and psychological clinical education involves training in interviewing skills, symptom/ability assessment, diagnosis and interpersonal communication, human SPs will soon be replaced due to high costs to hire, train and maintain a diverse group of patient actors. Even with SP programs, there are considerable challenges for maintaining the consistency of diverse patient portrayals for training students.
Professionals need to responsibly select and use the technology based on functional knowledge of its strengths, applications and limitations (e.g., privacy, confidentiality, data integrity, security) before engaging patients with it. TBH practice is based on evidence, consensus and other professional, discipline-based guidelines, but the rapidly changing marketplace and healthcare reform are challenging educational and service delivery systems to deliver professionals who are fully prepared to deliver proficient, legal and ethical care. If behavioral health professions were to outline core telecompetencies and clarify how in-person care need be adjusted, they could proactively help professional organizations and regulatory boards, which attend to clinical standards (i.e., professional conduct, practice and treatment guidelines, standards of care, scope of practice). While technology competencies are being used in residency training programs, they have not been added literally in accreditation processes for two reasons.
Research in social neuroscience13 and cognitive neuroscience14 is creating, exploring and testing environments used for learning, engagement and reflection by simulating day-to-day life, social situations with objective stimuli and reactions to unusual stimuli. Clinical VR will have a significant impact on future research and practice. VR, AR and VE applications that foster TPrwill become indispensable tools in the toolbox of psychological researchers and practitioners and will only grow in relevance and popularity in the future.12 The main premise here is that the best evidence-based approach for assessing or treating a clinical health condition serves little value if clients do not seek it out and participate in it. VR is a tool for advancing care (e.g., self-help cognitive behavioral therapy; CBT) outside of the clinic, making treatment available to a wider group of patients who may be drawn to these types of technology-based interventions. Whatever succeeds in the marketplace will engender the need for professional guidelines, competencies and further professional training to promote its safe and ethical use.
This paper has several limitations. First, the scope it perhaps both two broad conceptually and too narrow in findings. Second, there is inadequate information about the intersection of the topics, which is a good reason for a scoping review approach, as the best approaches to research are still in progress with clinical populations. Adapting social neuroscience and other paradigms to clinical care to explore technology appears indicated. Third, this paper did not formally assess individual studies using tools typically used in systematic reviews or meta-analyses (e.g.; Cochrane Risk of Bias Tool),118 or the grade approach to assessing the quality of the evidence and strength of recommendations. However, for each study, at least two members of the team discussed and came to consensus on both the limitations and its usefulness to the overall review. Finally, future studies should more explicitly address the high degree of variability between treatment settings and more controlled environments. Additional evaluation/research, informal guidelines, elaboration of potential contraindications and integration of technology into stepped models of care are needed.
DISCLOSURE
On behalf of all authors, the corresponding author states that there are no financial or personal conflicts of interest. The authors participate in national organizations, but do not have leadership positions, nor would that participation impact competencies, as far as can be ascertained. The authors alone are responsible for the content and writing of the paper.
ACKNOWLEDGMENT
None.
ETHICAL CONSIDERATIONS
IRB approval was not necessary due to this being a review of literature.
FUNDING SOURCES
No funding sources were required for this literature review.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.