INTRODUCTION
Due to the increasing prevalence of Diabetes Mellitus (DM) and an increase in the elderly population, there has been an increase in cases of Peripheral Arterial Disease (PAD). It is important to note that the biggest cause of lower-limb amputations in the elderly population is PAD.1,2,3 Despite the current progress in revascularization procedures for Critical Limb Ischemia (CLI), more than 100,000 major amputations are performed annually in the US.4,5
In recent years, due to increased recognition of the functional advantages of preservation of the knee joint and advances in revascularization procedures, many surgeons recognize the benefits of preservation of the knee joint when performing amputation surgery. As a result, the ratio of Trans-femoral (TF) to Trans-tibial (TT) amputation has decreased over the years.2,6,7,8 However, patients with higher level lower limb amputations resulting not only from vascular disease but also from tumor and trauma exist. Because of the increase in the elderly population, most patients have multiple comorbidities and rehabilitation is not always easy. It has been reported that the rehabilitation success rate for elderly lower limb amputees is 66-76% for TT and 46-53% for TF amputees.9,10,11 However, the rehabilitation success rate for patients with PAD is lower than the generally reported success rates.
It has been reported that rehabilitation success rates are only 34%-47% for TT amputees and 9-20% for TF amputees.12,13,14 Thus, many older patients may not be considered successful prosthetic rehabilitation candidates. Furthermore, it is not easy to predict the outcomes of these patients, to decide the indication for prosthetic rehabilitation even for experienced clinicians.15 If predictions of successful prosthetic rehabilitation could be made more accurately in older patients with higher level lower limb amputations before commencing rehabilitation, it would greatly help to delineate an efficient multidisciplinary rehabilitation approach with clearer rehabilitation goals.
Several predictive factors affecting successful prosthetic rehabilitation have been described in previous research. However, most previous research studied subjects with various amputation levels and wide age ranges, from young to elderly patients. Furthermore, as indicated by Moore,10 despite the increased energy consumption required for prosthetic walking the higher the level of amputation, previous research has not included an evaluation of the physical fitness of amputees. Thus, this previous research may not be enough to clinically determine rehabilitation goals. In this study, subjects were limited to unilateral trans-femoral and hip disarticulation amputees aged 60-years or above who entered our center with no previous prosthetic rehabilitation history. The physical fitness of amputees was evaluated using an exercise load test. The aim of this study was to determine the threshold of physical fitness level in terms of maximum oxygen uptake as a predictive factor for achieving prosthetic walking in elderly with unilateral trans-femoral amputation or hip disarticulation.
MATERIALS AND METHODS
Subjects
The patients were 69 unilateral lower limb (trans-femoral amputation or hip disarticulation) amputees (44 men and 25 women) who were hospitalized at Hyogo Rehabilitation Center (Kobe Japan) for prosthetic walking training and who had never been fitted with prosthesis before. All of them were referred to our center for prosthetic rehabilitation. Their age was 67.3±5.5 years (Mean±SD, Range 60-81 years). The cause of amputation was PAD in 25 cases and non-PAD in 44 cases. The amputation level was TF in 58 patients and Hip Disarticulation (HD) in 11 patients. None of the patients had any Steinberg factors11 impeding prosthetic walking such as mental deterioration, advanced neurological disorders, congestive cardiac failure, advanced obstructive pulmonary disease, or advanced hip flexion contracture. The patients were informed of the purpose of this study and the associated risks, and verbal and written consent was obtained. The study protocol and methods were approved by the Institutional Review Board of Hyogo Rehabilitation Center (Kobe Japan).
Rehabilitation Program
The rehabilitation program was identical for all patients. Training programs for walking with prosthesis emphasize acclimatization to the use of a prosthesis, bearing an adequate amount of body weight on the prosthesis, and the correction of abnormal walking patterns. Once amputees can overcome these problems and achieve a walking speed within a certain range that suited them, their training was completed. This program emphasizes on endurance, and aimed at achieving prosthetic walking with any necessary ambulatory aids (cane, crutch, or walker) at amputees most comfortable walking speed.
Evaluation of Prosthetic Ambulation Ability
After completion of the rehabilitation program, patients were permitted to use any necessary ambulatory aids and asked to walk at their most comfortable walking speed on a level surface. Patients who could walk at least 100 meters without ambulatory aids or with only one cane were classified as successful prosthetic users. All others were classified as failed prosthetic users.
Investigation of Clinical Information
Information about each patient before fitting prosthesis was collected retrospectively from clinical charts made during admission. This information included cause of amputation (PAD or non-PAD), number of co-morbidities, and ability to stand on the non-amputated leg (possible or impossible). Co-morbidities were common in these patients, and included the presence of hypertension, DM, end-stage renal disease, hepatic disorders, cerebral vascular disturbance, ischemic heart disease, degenerative joint disease, visual disorder, endocrine disease, malignant disorder such as metastasis, and inflammatory disease such as chronic osteomyelitis. Standing was assessed as possible if patients could stand either unsupported or supported by one hand on a desk.
Evaluation of Physical Fitness
Lower limb amputees performed one-leg cycling tests with the non-amputated leg. This test was conducted before the patients began prosthetic rehabilitation. The details of this method have already been reported.16 A cycle ergometer (Lode Angio WLP-300ST, Holland, Netherlands) that can be manipulated in a supine position was used.
The test was conducted with the patients seated with their upper bodies reclining at an angle of approximately 45 degrees. This incremental exercise test was begun with 3 minutes of unloaded pedalling, followed by increments of 5~15 W/min, until the patient’s self-assessed maximum load. The test patients were directed to turn the pedals 60 times per minute. Each patient operated the ergometer with his or her non-amputated leg. During exercise, respiratory gas was monitored with a respiromonitor (Minato RM-300 system, Osaka, Japan) to obtain oxygen uptake (VO2). At the same time, electrocardiograms and heart rate were monitored by a stress test system (ML-5000, Fukuda Denshi, Tokyo, Japan), and cuff blood pressure was determined every minute with an autoelectrocardiometer (STPB-780, Colin, Komaki, Japan).
The maximum oxygen uptake (ml/kg per minute) during exercise, as a proportion of the predicted maximum oxygen uptake (%VO2max; ml/kg per minute) was used as an indicator of physical fitness.
STATISTICAL ANALYSIS
Continuous variables (Age and %VO2max) were compared using t-tests, and categorical variables (sex, cause of amputation, number of comorbidity, level of amputation and ability to stand on non-amputated leg) using chi-squared tests to determine which variables differed significantly between the success and failure groups. The variables that achieved statistical significance in t-tests or chi-squared tests at the 0.05 level were then included in multivariate logistic regression analysis. Pearson correlation co-efficients were calculated to determine the strength of the relationship between variables. The model was simplified in a stepwise fashion by removing variables with a P value greater than 0.05. Odds Ratio (OR) and 95% Confidence Interval (CI) were calculated for successful walking with prosthesis associated with independent variables. Model fit was tested with Hosmer-Lemeshow statistics. Sensitivity and specificity in predicting successful walking status were calculated. Sensitivity was defined as the percentage of the success group who were correctly identified. Specificity was defined as the percentage of the failure group who were correctly identified. The ability to predict the outcome of successful walking was assessed by the area under the Receiver Operating Characteristic (ROC) curve.
Statistical evaluation of the data was carried out using the SPSS® statistical package (SPSS Inc., Chicago, IL, USA) for Windows®.
RESULTS
In the prosthetic ambulation ability evaluation, there were 47 amputees in the success group (30 men and 17 women) aged 66.6±5.3 years, 10 were HD amputees. There were 22 amputees in the failure group (14 men and 8 women) aged 68.8±6.0 years, 1 was a HD amputee. In the failure group, 5 amputees could walk more or less than 100 m with two canes, 10 could walk with crutch, 1 with walker, and 6 could not walk at all and used wheelchair. There was a significant difference between the two groups in cause of amputation, number of co-morbidities, ability to stand on the non-amputated leg, and %VO2max (p<0.05). No significant difference was observed between the two groups in age, sex and the level of amputation (Table 1). No high correlation was determined between variables.
Table 1. Results of Success Group and Failure Group
|
Success Group
n=47
|
Failure Group
n=22
|
p value
|
| Agea) |
66.6±5.3
|
68.8±6.0
|
p=0.124b)
|
| Sex (male/female) |
30/17
|
14/8
|
p=0.988c)
|
| Cause of amputation (PAD/Non-PAD) |
13/34
|
12/10
|
p=0.030c)
|
|
No. of Comorbidity
≦1
2
≧3
|
36
11
0
|
8
8
6
|
p<0.0001c)
|
| Level of amputation (TF/HD) |
37/10
|
21/1
|
p=0.077c)
|
| Ability to stand on non-amputated leg (Possible/Impossible) |
45/2
|
12/10
|
p<0.0001c)
|
| %VO2max a) |
64.7±14.2
|
44.7±9.3
|
p<0.0001b)
|
a) Mean±SD b) Non-paired t-test c) χ2: chi-squared test
TF: trans-femoral, HD: hip disarticulation, PAD: peripheral arterial disease
Significant difference was observed between the two groups in cause of amputation, number of co-morbidities, ability to stand on the non-amputated leg, and %VO2max (physical fitness). No significant difference was observed between the two groups in age, sex and the level of amputation. |
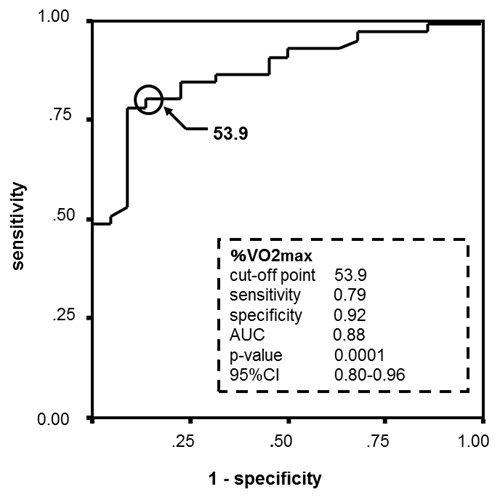
Cause of amputation, the number of co-morbidities, one leg standing, and %VO2max were subjected to logistic regression analysis as independent variables. Based on the calculated OR, %VO2max was found to be significantly related to successful prosthetic walking (p=0.002) (Table 2). ROC analysis showed that %VO2max best differentiated subjects who belonged to the success group from those who belonged to the failure group at a threshold score of 53.9 (Figure 1). The sensitivity of success prediction was 79% and specificity was 92% (Hosmer-Lemeshow goodness of fit test, p=0.93).
Table 2. Stepwise Logistic Models for Predicting Successful Prosthetic Walking
|
Predictor
|
OR
|
95% CI
|
p value
|
| Cause of amputation (PAD/Non-PAD) |
0.59
|
0.12-2.95
|
p=0.521
|
| No. of comorbidity (≦1, 2/≧3) |
0.52
|
0.14-1.90
|
p=0.321
|
| Ability to stand on non-amputated leg (Possible/Impossible) |
5.48
|
0.73-41.38
|
p=0.099
|
| %VO2max |
1.13
|
1.05-1.22
|
p=0.002
|
| Hosmer-Lemeshow test |
χ2=3.02
|
p=0.93
|
|
OR: Odds Ratio.
95% CI: 95% Confidence Interval
Logistic regression analysis showed that %VO2max (physical fitness) was significantly related to successful prosthetic walking. |
Figure 1. ROC Analysis for %VO2max
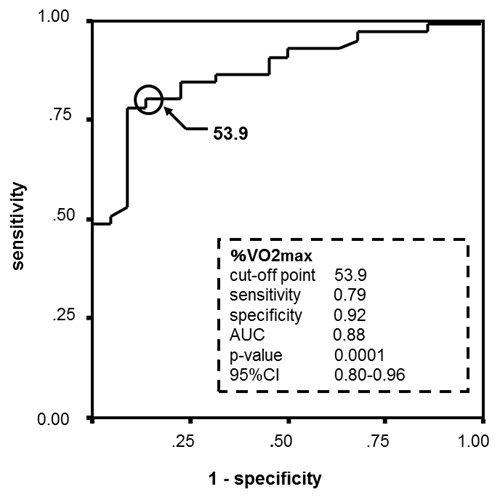
ROC analysis showed that 53.9 were the threshold score of %VO2max for distinguish
success group from failure group, and its sensitivity was 79%, and specificity 92%.
DISCUSSION
A number of researchers have identified cause of amputation,3,17,18 number of coexisting factors,19,20,21,22,23 ability to stand on one leg,17,20,24 and physical fitness20,25 as important factors related to successful prosthetic rehabilitation. Our results were in agreement with previous reports in many respects. Based on the logistic regression analysis applied in this study, %VO2max as an indicator of physical fitness was found to be significantly related to successful walking. Various experts have indicated that physical fitness adequate to meet the energy consumption demands of prosthetic walking is important for geriatric lower limb amputees to regain practical prosthetic walking ability.11,26,27,28 Furthermore, Moore10 and Steinberg11 have stated the importance of evaluating the physical strength of amputees before they begin rehabilitation. However, these researchers have not discussed the level of physical fitness required for successful prosthetic rehabilitation. Very little research has mentioned the possibility of using physical fitness level as a predictive factor for successful prosthetic rehabilitation.29 We previously reported that 50~60% VO2max can be regarded as a guideline for the physical fitness level required for successful prosthetic rehabilitation in older lower limb amputees.20,25 However our previous research did not identify the specific value of physical fitness. By choosing an optimal cut-off value of 53.9%, sensitivity was calculated as 79%, and specificity, 92%. Thus quite high predictability of rehabilitation success was achieved. This is the first research that has specified physical fitness level as a predictive factor for successful prosthetic rehabilitation.
Morey30 examined the relationship between directly measured peak oxygen uptake and self-reported physical functioning in older adults aged 65-90 years old, and reported that individuals with the oxygen uptake less than 18.3 ml/kg/min had significant difficulty in the performance of daily tasks. Bruce31 proposed an assessment method to predict maximum oxygen uptake (VO2max) from an individual’s age. According to his report, the predicted VO2max of active older men aged 60-70 years old can be expressed as 33 and 27 ml/kg/min, and active older women aged 60-70 years as 24 and 20 ml/kg/min, respectively. Therefore, 53.9% VO2max was within 18.3 ml/kg/min, that was detected as a minimum guideline for older adults to be able to perform daily tasks. According to Posner,32 around 60% VO2max represents an exercise intensity approximately equal to the anaerobic threshold value for people in their 50-70 s. Kurdibaylo27 conducted exercise load tests on lower limb amputees using arm ergometry and reported that the movement capabilities depend to a large extend on the physical fitness of the subjects, and 40-60% VO2max was the acceptable exercise intensity that lower limb amputees could bear. Therefore, our value of 53.9% VO2max seemed not to be an excessive exercise intensity.
In this study, we classified the patients who could walk at least 100 meters without ambulatory aids or with only one cane as successful prosthetic users. Because there is no standard definition for successful prosthetic rehabilitation,21,33 and we considered that prosthetic users who could walk at least 100 meters had sufficient ability for prosthetic ambulation in their community. Actually, in the success group, 39 of 47 patients (82.9%) could keep their walking ability with prosthesis at 6 month after discharge from our center. On the contrary, in the failure group, only 4 of 22(18.2%) patients could walk with two canes or crutch after discharge. Therefore, our classification seems to be appropriate.
As to prescription of prosthesis, type of suspension was Canadian socket for all hip disarticulation amputees, and suction socket for all Trans-femoral amputees. Knee mechanisms were as follows; 47 success group amputees,19 were prescribed single axis knee joint, 19 polycentric knee joint, 9 fixed knee joint, and 22 failure group amputees, 7 were single axis knee joint, 7 polycentric knee joint, 8 fixed knee joint, respectively. At 6 month follow up after discharge, 39 success group amputees who could keep their walking ability, 16 were single axis (dropout rate 15.8%), 17 polycentric (10.6%), 6 fixed (33.2%), and 4 failure group amputees who could keep their walking ability, 1 were single axis (dropout rate 85.8%), 1 polycentric (85.8%), 2 fixed (75.0%), respectively. We found no relationship between the type of prosthesis and the outcome of 6 month follow-up.
The limitation of this research is the necessity of expensive and special apparatus, and thus measurement of physical fitness cannot be easily and routinely performed. Since independence in activities of daily living has been significantly associated with walking ability after rehabilitation with a prosthesis,34 and 53.9% VO2max is the value within the range of minimum guideline for the older adult to perform daily tasks,30 when the apparatus is not clinically available, assessing whether an amputee is independent in performing daily tasks using a wheelchair before commencing prosthetic rehabilitation might be an alternative method to estimate physical fitness. If an amputee is found not to be independent, there might be a great possibility that he will not be a candidate for successful prosthetic rehabilitation.
CONCLUSION
In summary, this study showed that by using an optimal cut-off value of 53.9% VO2max, the predictability for achieving sufficient prosthetic walking ability on the basis of physical fitness was quite high. However, clinical judgment from the perspective of physical fitness alone is insufficient. Incorporating other predictive factors with the findings of this study is essential for increasing predictive accuracy.
ACKNOWLEDGEMENTS
Financial Disclosures: The authors received no specific funding for this work.
AUTHOR’S CONTRIBUTIONS
Study concept and design: T. Chin. Acquisition of data: T. Chin, H. Kohno and M. Toda. Analysis and interpretation of data: N. Maeda and M. Toda. Drafting manuscript: M. Toda and T. Chin. Critical revision of manuscript: A. Kitagawa.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest regarding the publication of this paper.
CONSENT
The subjects were informed of the purpose of this study and the associated risks, and signed consent was obtained.