OVERVIEW
A case study about wound bed preparation with the help of negative pressure wound therapy with instillation dwell time (NPWTi-d) over below knee amputation stump.
INTRODUCTION
Negative pressure wound therapy (NPWT) is a time tested method of managing wounds. Its efficacy in preparing any wound for the definitive treatment or its role as a bridging procedure is wellknown. But, the modifications of negative pressure wound therapy is comparatively new. When combined with oxygen, it is known as regulated oxygen negative pressure wound therapy (RONPT), whereas when combined with various medicated solutions, it is known as negative pressure wound therapy with instillation and dwell time.
Recently, we came across in the literature the NPWTi-d and its role in the wound bed preparation. In this article, we shall discuss our experience of using NPWTi-d in preparing a raw area over amputation stump for definitive wound cover.
MATERIALS AND METHODS
The study was conducted the Department of Plastic Surgery at a tertiary care center. This study was conducted after getting the informed consent and ethical committee clearance.
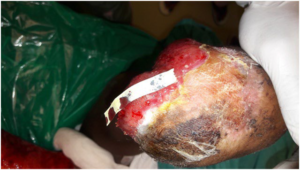
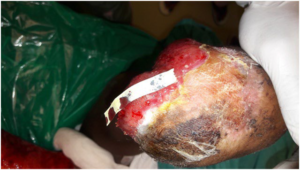
A 36-years-old female patient with no known comorbidities was admitted with infected raw area over the right below knee amputation stump and exposed bone. Initially the patient was treated with conventional wound therapy; wound irrigated with normal saline, swab taken for culture and sensitivity, thorough debridement of the wound followed by conventional dressing. The patient was treated with parenteral antibiotics based on exudate culture and sensitivity reports but the wound was not responding well and the dressing needed frequent change (Figure 1). So a decision to give a trial NPWTi-d for wound bed preparation was made.
Figure 1. Raw Area Over the Stump before NPWTi-d Application
Negative pressure wound therapy was applied with the help of sterile polyurethane sponge and two tubes. The tubes were inserted longitudinally into the sponge. Before NPWTi-d, the wound was thoroughly debrided and meticulous hemostasis was achieved. Then the wound was covered with a sterile vaseline gauze. The sponge with tubes was placed over the vaseline gauze, and held in position with the help of a transparent occlusive dressing. One tube was dedicated to negative pressure and other for the antimicrobial solution instillation (Figure 2). The antimicrobial solution used was ionic silver solution. The amount of solution to be instilled each time was decided as the amount of solution required to wet the sponge completely and up to the point when the transparent occlusive covering just begin to lift. Negative pressure was applied at 125 mmHg. The wound was bathed with ionic silver solution and it allowed to stay in the wound for 10-minutes, after every 2-hours of negative pressure application. This was continued for 1-week. The dressing was opened at the end of 1st week, wound was washed with normal saline, exudate swab was taken, fresh debridement was done, and a new dressing was applied. This was repeated for the next 3-weeks.
Figure 2. NPWTi-d Dressing Applied

RESULT
By the end of third week, the wound became clean, fully covered with healthy granulation and the wound bed was ready to undergo the definitive wound cover procedure (Figure 3).
Figure 3. Post-NPWTi-d Stump with Healthy Granulation

DISCUSSION
The large wounds, in any patient is difficult to treat and the downtime required to heal the wound usually runs into months. It adds on to the cost of treatment and stress onto the patient and bystanders as wells as on the medical care facility. The negative pressure wound therapy with instillation and dwell time is a method that can be of help as an adjunct to decrease the downtime to prepare the wound for any definitive procedure e.g. grafting or flap cover.
The concept of negative-pressure wound therapy was known since 1997.1-3 The devices used for NPWT was described by Argenta et al.1 It consists of a highly porous polyurethane sponge, a semipermeable dressing, connecting tubes, and a vacuum source.
The NPWTi-d is a relatively newer concept. Instead of keeping the negative pressure on a continuous manner, it is applied intermittently (a break for 10-minutes, for antimicrobial solution instillation after every 2-hours of negative pressure) because it has been reported that intermittent negative pressure is more beneficial for the wound bed preparation than continuous negative pressure.4,5 The pressure applied was fixed at 125 mmHg. Morykwas et al,4,5 suggested that pressures that are lower or higher than 125mmHg result in a significant decrease in the formation of granulation tissue. The wound is also instilled with antimicrobial solution or normal saline. The optimal effective dwell time for antimicrobial solution is not clear in the published literature but in vitro studies evaluating the effect of various antimicrobial/antiseptic solutions on various types of bacteria and yeast suggests that longer contact times (>10-minutes) is effective in decreasing microbial counts.6,7 It is difficult to suggest an ideal volume of instillation solution. Because with variations in size, depth, and shape of the wound amount of fluid required to get a complete bathe of the wound may also vary. Too much solution may cause difficulty in maintaining a negative pressure seal with the occlusive dressing and will produce maceration of the surrounding tissue, while insufficient volume will not allow the solution to bathe the entire wound surface. Therefore, any recommendation for an absolute volume of solution is not practically possible. The widely accepted recommendation is to monitor the foam until it is completely saturated and just begins to raise the transparent occlusive dressing.8
The NPWTi-d is effective in reducing the downtime of wound bed preparation. It decreases the number of dressing changes required, treatment cost and reduces the sufferings of the patient. The limitation of this study is that it was done on a single patient, so it is difficult to draw a definite conclusion. To get a more exact data a large randomized control study is needed.
The NPWTi-d is not a replacement to excisional debridement. It only acts as a bridging procedure to prepare the wound for definitive wound cover; at a lesser downtime, with minimal number of dressing changes, at a lower treatment cost and thus it decreases the sufferings of the patient.9
CONCLUSION
The NPWTi-d is effective in reducing the downtime of wound bed preparation. It decreases the number of dressing changes required, treatment cost and reduces the sufferings of the patient. The limitation of this study is that it was done on a single patient, so it is difficult to draw a definite conclusion. To get a more exact data a large randomized control study is needed.
DECLARATIONS
Author’s Contributions
All authors made contributions to the article.
Availability of Data and Materials
Not applicable.
Financial Support and Sponsorship
None.
Consent for Publication
Not applicable.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.