INTRODUCTION
Carotid cavernous fistula (CCF) infrequently occurs secondary to traumatic supraclinoid pseudoaneurysm of the internal carotid artery (ICA).1 A thorough search through PubMed has given evidence of only seven reported cases of the condition.2,3,4 CCF commonly occurs after head injuries, rupture of an aneurysm in the cavernous segment, or as a result of iatrogenic damage to the vessel during transsphenoidal surgery as in this case.5
The cases that have been reported in the past have been treated using one of the listed methods which are trapping, a combination of trapping and controlled embolization, and inserting a thrombogenic agent into the site of aneurysm. Even though these procedures have a positive post-operative outcome, they had a great impact on morbidity and mortality, thus, they are not applicable in all cases.6 Alternatively, the endovascular treatment option has shown promising results, through the placement of coils with stents, or coils without stents in the treatment of dissection of great vessels, fistulas, and extra-cranial arterial pseudo-aneurysms, while maintaining a patent flow through the parent artery. This case report discusses a post-traumatic iatrogenic CCF after a supraclinoid pseudoaneurysm that was treated through the coiling of the aneurysm.
CASE REPORT
A 45-year-old woman presented to a neurosurgeon with headaches and vertigo. Investigations and the clinical findings were suggestive of pituitary adenoma. The case was discussed in a multidisciplinary team meeting as well as with the patient and family. After discussing all the complications, the transsphenoidal route intervention was performed. However, during the procedure, there was massive bleeding from the carotid, and the operating team suspected that there was iatrogenic internal carotid artery damage; therefore, further surgery was abandoned. The patient kept deteriorating because of on-going hypovolemic shock, despite medical treatment and packing of the site. Consequently, the patient was moved to and managed in the intensive treatment unit (ITU), additionally, she was also referred to the interventional radiology (IR) for the possibility of emergency coil embolization.
As soon as IR received the patient’s information, the IR on-call team and cathlab team, arranged a digital subtraction angiography (DSA) on the patient with the aim of saving the patient’s life despite her rapid clinical deterioration. The clinical examination revealed a combination of proptosis and chemosis of the conjunctiva of the right eye with facial swelling (right>left) (Figure 1).
Figure 1. Proptosis and Chemosis of the Right Eye

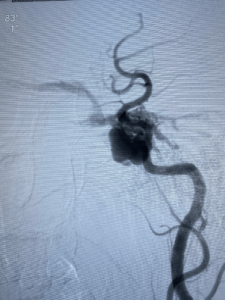
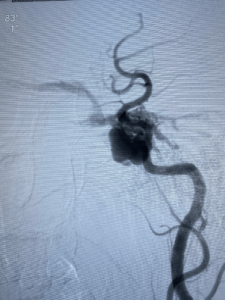
Upon further investigations with DSA, the patient was found to have a massive 3 cm×1 cm supraclinoid aneurysm that had ruptured into the cavernous sinus leading to the formation of a CCF with the dilation of the superior ophthalmic vein (SOV) (Figure 2).
Figure 2. The Communication between the Aneurysm with Cavernous Sinus
Following the DSA and considering the clinical scenario, the patient and the family was offered coiling of supraclinoid pseudoaneurysm. The consent for the procedure and publication of the case was undertaken.
Procedure
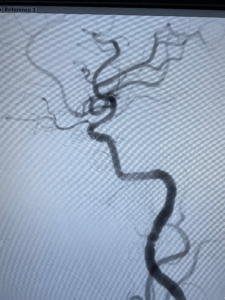
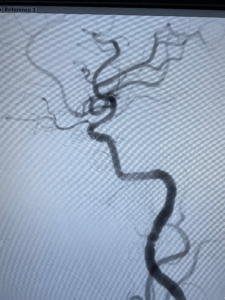
The origin of the aneurysm was located by insertion of a femoral micro-catheter. The aneurysm was noted to be proximal to the bifurcation of the ICA. The location of the aneurysm was noted to be anterior to the ophthalmic artery. Coiling of the aneurysm fully closed the CCF (Figure 3).
Figure 3. Complete Occlusion of Carotid-cavernous after the Aneurysm Coiling
There were no intra-operative or post-operative complications, and the patient reported improvement in her right eye vision during her follow-up visits. Currently, the patient has been followed for a year, with complete resolution of the proptosis, chemosis, and fascial puffiness. She has not developed any new complaints during the follow-up (Figure 4).
Figure 4. Post Recovery Picture

DISCUSSION
It is well-established that intracranial pseudoaneurysms can result from an iatrogenic procedure or head trauma. However, these cases are infrequent and only account for around 1% of all intracranial aneurysms. This fact led to the conclusion that the pseudoaneurysm was iatrogenic in nature after the patients complained about visual symptoms, history, the age, as well as the deterioration that happened post-procedure, including presence of the CCF, absence of the neck, and the location of the aneurysm which was away from the point where the ICA had branched. The combination of these signs points towards a traumatic origin.7
A cause of the traumatic aneurysm of the supraclinoid ICA may be a direct injury to the ICA by a skull base fracture. Other causes include, torsion of the ICA wall caused by the movement of the brain when the impact happened, and fracture of the surrounding bony structures.8 It has been determined that aneurysms that are of traumatic origin have a high mortality rate.
CCF presents in a unique way, including proptosis, and chemosis with restricted eye movements, secondary to abducent nerve involvement with or without oculomotor nerve palsy. Furthermore, diplopia, reduction of vision, retinal hemorrhage, and bruits can be observed. These signs suggest the overfilling of the draining vein of the superior ophthalmic vein9 together with the inferior petrosal sinus. The increased drainage of superior orbital vein leads to eye symptoms with deterioration of vision as a result of low perfusion to the optic nerve and the retina, leading to retinal hemorrhage, chemosis and proptosis. Supraclinoid segment pseudoaneurysms are commonly linked to subarachnoid hemorrhage which may present as CCF. In the current case, the iatrogenic supraclinoid pseudoaneurysm was treated using the transarterial approach. This approach resulted in the closure of the fistulous tract and the improvement of the eye symptoms exhibited.10
The best treatment of pseudoaneurysm with similar manifestations is to eliminate the fistula and secure the carotid flow through the application of various endovascular methods. Surgical clipping has an elevated risk of pseudoaneurysm formation as a result of its delicate anatomy.11 Each case should be investigated to rule out fistulous tracts, and pseudoaneurysms while maintaining the patency of the flow in the main artery.
DECLARATION OF THE PATIENT’S CONSENT
The authors of this document affirm that the necessary consent forms were filled in at all steps. The patient had provided her consent for the pictures and clinical information that is published here. The name and identity of the patient will not be revealed, but their anonymity will not be assured.
FINANCIAL SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.