1. Solbiati L, De Pra L, Ierace T et al. High-resolution sonography of the recurrent laryngeal nerve: anatomic and pathologic considerations. AJR Am J Roentgenol. 1985; 145(5): 989-993.doi: 10.2214/ajr.145.5.989
2. Fornage BD, Rifkin MD. Ultrasound examination of the hand and foot. Radiol Clin North Am. 1988; 26(1): 109-129.
3. Hughes RAC. Peripheral neuropathy. BMJ. 2002; 324: 466- 469.doi: 10.1136/bmj.324.7335.466
4. Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve. 2008; 37(5): 566-571. doi: 10.1002/mus.21009
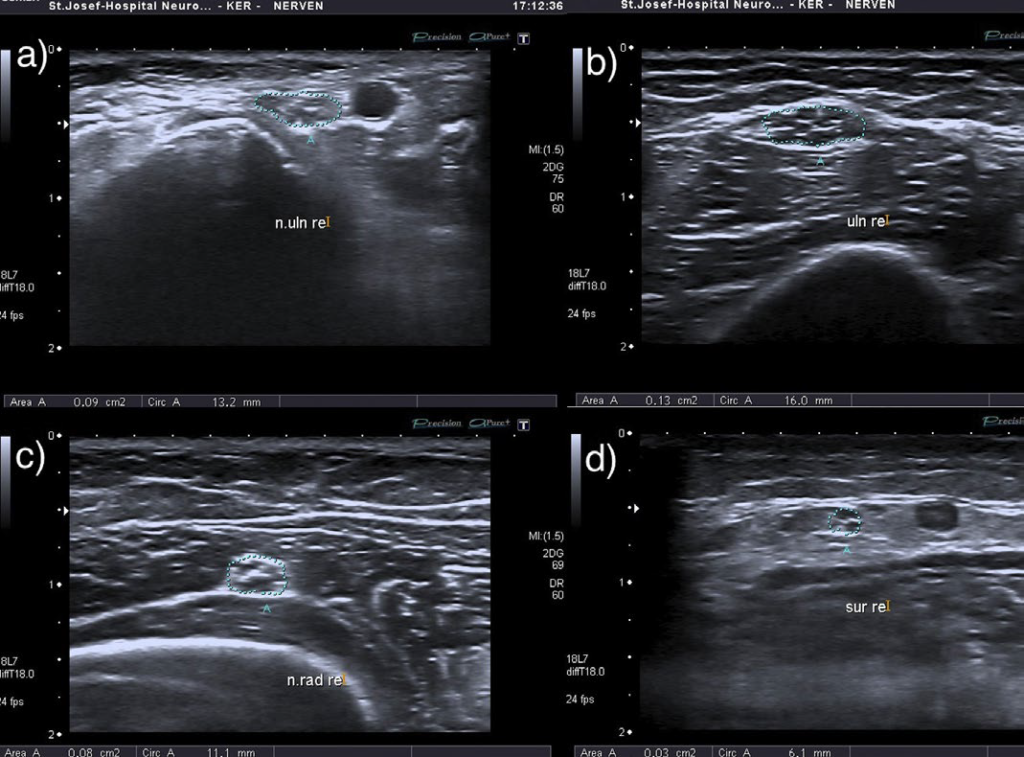
5. Kerasnoudis A, Pitarokoili K, Behrendt V, Gold R, Yoon MS. Cross sectional area reference values for sonography of peripheral nerves and brachial plexus. Clin Neurophysiol. 2013; 124(9): 1881-1888. doi: 10.1016/j.clinph.2013.03.007
6. Padua L, Martinoli C, Pazzaglia C, et al. Intra- and internerve cross-sectional area variability: new ultrasound measures. Muscle Nerve. 2012; 45(5): 730-733. doi: 10.1002/ mus.23252
7. Kerasnoudis A, Klasing A, Behrendt V, Gold R, Yoon MS. Intra- and internerve cross-sectional area variability: new ultrasound measures. Muscle Nerve. 2012; 47(1): 146-147.doi: 10.1002/mus.23520
8. Chiò A, Cocito D, Bottacchi E, et al. Idiopathic chronic inflammatory demyelinating polyneuropathy: an epidemiologi cal study in Italy. J Neurol Neurosurg Psychiatry. 2007; 78: 1349-1353.doi: 10.1136/jnnp.2007.114868
9. Iijima M, Koike H, Hattori N, et al. Prevalence and inci–dence rates of chronic inflammatory demyelinating polyneuropathy in the Japanese population. J Neurol Neurosurg Psychiatry. 2008; 79: 1040-1043. doi: 10.1136/jnnp.2007.128132
10. Hughes R. Chronic Inflammatory Demyelinating Polyradiculoneuropathy. J Clin Immunol. 2010.doi: 10.1007/s10875-010-9399-0
11. Taniguchi N, Itoh K, Wang Y, et al. Sonographic detection of diffuse peripheral nerve hypertrophy in chronic inflammatory demyelinating polyneuropathy. J Clin Ultrasound. 2000; 28(9): 488-491. doi: 10.1002/1097-0096(200011/12)28:9<488::aid-jcu7>3.0.co;2-7
12. Duggins AJ, McLeod JG, Pollard JD, et al. Spinal root and plexus hypertrophy in chronic inflammatory demyelinating polyneuropathy. Brain. 1999; 122(Pt7): 1383-1390.doi: 10.1093/brain/122.7.1383
13. Mizuno K, Nagamatsu M, Hattori N, et al. Chronic inflammatory demyelinating polyradiculoneuropathy with diffuse and massive peripheral nerve hypertrophy: distinctive clinical and magnetic resonance imaging features. Muscle Nerve. 1998; 21(6): 805-808. doi: 10.1002/(SICI)1097-4598- (199806)21:6<_x0038_05:_x003a_AID-MUS16>3.0.CO;2-R
14. Naganuma M, Doi S, Shima K, et al. Chronic inflammatory demyelinating polyradiculoneuropathy associated with multifocal nerve hypertrophy: report of a case with MRI study. Rinsho Shinkeigaku. 1991; 31(11): 1186-1191.
15. Matsuda M, Ikeda S, Sakurai S, et al. Hypertrophic neuritis due to chronic inflammatory demyelinating polyradiculoneuropathy (CIDP): a postmortem pathological study. Muscle Nerve. 1996; 19(2): 163-169. doi: 10.1002/(SICI)1097-4598(199602)19:2<163::AID-MUS6>3.0.CO;2-C
16. Matsuoka N, Kohriyama T, Ochi K, et al. Detection of cervical nerve root hypertrophy by ultrasonography in chronic inflammatory demyelinating polyradiculoneuropathy. J Neurol Sci. 2004; 219(1-2): 15-21. doi: http://dx.doi.org/10.1016/j. jns.2003.11.011
17. Imamura K, Tajiri Y, Kowa H, Nakashima K. Peripheral nerve hypertrophy in chronic inflammatory demyelinating polyradiculoneuropathy detected by ultrasonography. Intern Med. 2009; 48(7): 581-582. doi: http://dx.doi.org/10.2169/internalmedicine.48.1924
18. Jang JH, Yoo JK, Kim BJ. Ultrasonographic findings in chronic inflammatory demyelinating polyneuropathy. Am J Phys Med Rehabil. 2012; 91(6): 546-547.doi: 10.1097/PHM.0b013e31824121f1
19. Kerasnoudis A. Ultrasound findings in a case of chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 2013; 47(3): 443-446.
20. Kerasnoudis A. Ultrasonographic findings in chronic inflammatory demyelinating polyneuropathy. Am J Phys Med Rehabil. 2014; 93(1): 94.
21. Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normal and patients with polyneuropathy: an ultrasound study. Muscle Nerve. 2009; 40(6): 960-966.doi: 10.1002/mus.21431
22. Kerasnoudis A, Gold R, Klasing A, Behrendt V, Yoon MS. Correlation of morphological changes in CIDP with the disease duration. 85. Kongress der Deutschen Geselschaft für Neurologie (DGN). 27.09.12, Hamburg Germany. P555.
23. Kerasnoudis A, Pitarokoili K, Behrendt V, Gold R, Yoon MS. Correlation of Nerve Ultrasound, Electrophysiological and Clinical Findings in Chronic Inflammatory Demyelinating Polyneuropathy. J Neuroimaging. 2014. doi: 10.1111/jon.12079
24. Smith EC, Hobson-Webb LD, Massey E. Nerve ultrasound in motor conduction block: pre- and post treatment findings. Muscle Nerve. 2008; 38: 1369.
25. Granata G, Pazzaglia C, Calandro P, et al. Ultrasound visualization of nerve morphological alteration at the site of conduction block. Muscle Nerve. 2009; 40(6): 1068-1070. doi: 10.1002/mus.21449
26. Imamura K, Tajiri Y, Kowa H, et al. Peripheral nerve hypertrophy in chronic inflammatory demyelinating polyradiculoneuropathy detected by ultrasonography. Intern Med. 2009; 48(7): 581-582.doi: 10.2169/internalmedicine.48.1924
27. Jang JH, Cho CS, Yang KS, Seok HY, Kim BJ. Pattern analysis of nerve enlargement using ultrasonography in chronic inflammatory demyelinating polyneuropathy. Clin Neurophysiol. 2014. doi: 10.1016/j.clinph.2013.12.115
28. Padua L, Granata G, Sabatelli M, et al. Heterogeneity of root and nerve ultrasound pattern in CIDP patients. Clin Neurophysiol. 2014; 125(1): 160-165. doi: 10.1016/j.clinph.2013.07.023
29. Koller H, Kieseier BC, Jander S, Hartung P. Chronic inflammatory demyelinating polyneuropathy. N Engl J Med. 2005; 352(13): 1343-1356.doi: 10.1056/NEJMra041347
30. Vallat JM, Sommer C, Magy L. Chronic inflammatory demyelinating polyradiculoneuropathy: diagnostic and therapeutic challenges for a treatable condition. Lancet Neurol. 2010; 9(4): 402-412.doi: 10.1016/S1474-4422(10)70041-7
31. Dalakas MC. Advances in the diagnosis, pathogenesis and treatment of CIDP. Nat Rev Neurol. 2011; 7(9): 507-517. doi: 10.1038/nrneurol.2011.121
32. Hughes RA, Donofrio P, Bril V, et al. ICE Study Group. Intravenous immune globulin (10% caprylate-chromatography purified) for the treatment of chronic inflammatory demyelinating polyradiculoneuropathy (ICE study): a randomised placebo-controlled trial. Lancet Neurol. 2008; 7(2): 136-144. doi: 10.1016/S14744422(07)70329-0
33. Dionne A, Nicolle MW, Hahn AF. Clinical and electrophysiological parameters distinguishing acute-onset chronic inflammatory demyelinating polyneuropathy from acute inflammatory demyelinating polyneuropathy. Muscle Nerve. 2010; 41(2): 202- 207. doi: 10.1002/mus.21480
34. Ruts L, Drenthen J, Jacobs BC, Van Doorn PA. Dutch GBS Study Group. Distinguishing acute-onset CIDP from fluctuating Guillain-Barre syndrome: a prospective study. Neurology. 2010; 74(21): 1680-1686. doi: 10.1212/WNL.0b013e3181e07d14
35. Kerasnoudis A, Pitarokoili K, Behrendt V, Gold R, Yoon MS. Nerve ultrasound score in distinguishing chronic from acute inflammatory demyelinating polyneuropathy. Clin Neurophysiol. 2014; 125(3): 635-641.doi: 10.1016/j.clinph.2013.08.014