INTRODUCTION
The tarsal tunnel is a fibro-osseous space found in the medial aspect of the ankle, posterior to the medial malleolus, bounded by the flexor retinaculum superiorly, and by the medial walls of the distal tibia, talus and calcaneus inferiorly. The tendons of tibialis posterior, flexor digitorum longus and flexor hallucis longus, the posterior tibial nerve, artery and vein run together through the tarsal tunnel.1,2 The tarsal tunnel syndrome can be caused by extrinsic or intrinsic pressure on the posterior tibial nerve or on its terminal branches: the medial plantar nerve, the lateral plantar nerve, the medial calcaneal nerve, the motor branch to the abductor muscle of the fifth toe and/or the inferior calcaneal nerve.1,2 Diagnosis is usually based on physical examination and can be confirmed by electrophysiological evidence. The treatment of the tarsal tunnel syndrome varies depending on the cause that underlies the pathology.
We report a case of a tarsal tunnel syndrome caused by a varicose vascular structures identified by foot MRI.
CASE REPORT
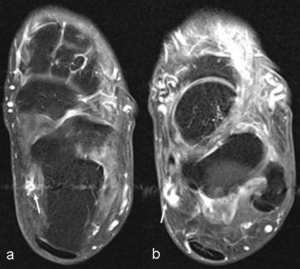
An eighty-year old male came to our attention for a chronic intermittent bilateral plantar numbness affecting him from 5 years. Symptoms were evident especially in the left foot when taking a bath or after a long distance walk. The plantar numbness was not caused by his shoes. On physical examination, the patient showed no muscular atrophy. Flat foot deformity was present bilaterally and a lot of varicose vascular structures in both lower extremities were observed. The patient referred paresthesias and lack of sensation in both lower legs and in foot dorsal and plantar areas. The ranges of motion testing of the cervical and lumbar spines were found to be full and pain free in all directions. The range of motion of the ankles was full and pain free bilaterally. Resisted range of motion testing including resisted dorsiflexion, plantar flexion, inversion, and eversion of the ankle was found to be pain free and of equal strength bilaterally. Neurological testing of the lower extremities was found to be positive for the Tinel sign at the medial malleolus level. Non weight bearing examination of the feet uncovered ‘medium’ and approximately equal plantar longitudinal arch height bilaterally. Toe and heel walking were unremarkable bilaterally. No Hallux deformity was detected. Bilateral weight bearing feet x-rays showed evidence of soft tissue swelling around ankles, suggesting the presence of varicose vascular structures. There was no evidence of bony fusion or other bones deformity in both ankles and feet. Left ankle MRI showed evidence of a lot of varicose vascular structures mainly medical aspect in the lower part of the leg and foot on T1 weighted axial (TR/TE 518/20 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm) and T2* weighted sagittal image (TR/TE 430/14 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm) (Figure 1a and b). One of the varicose vascular structures was suddenly narrow at level of tarsal tunnel. In addition, posterior tibial vein at the tarsal tunnel was dilated on gadolinium enhanced fat suppression T1 weighted axial image (TR/TE 518/20 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm) (Figure 2a) and appeared to continue with the varicose vascular structure (Figure 2b). Deep venous system thrombosis of the left lower leg was uncertain on this MRI. These findings suggested that superficial venous valve insufficiency caused a blood regurgitation and dilatation not only in superficial veins but also in posterior tibial vein and through some communicating branches between superficial vein and posterior tibial vein. The right MRI was not taken at first time. From both the physical examination and the left MRI findings, we diagnosed a tarsal tunnel syndrome caused by a dilatation of the posterior tibial vein and by a compression of the varicose structures around the tarsal tunnel.
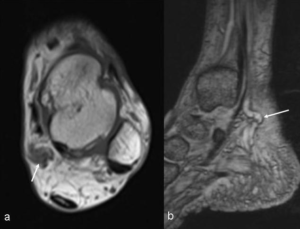
Figure1: Varicose vascular structure at level of tarsal tunnel.
a. T1 weighted axial image (TR/TE 518/20 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm) shows evidence of dilated vessel suggestive of varix at level of the right tarsal tunnel (arrow).
b. T2* weighted sagittal image (TR/TE 430/14 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm)shows dilated superficial vein at posterior aspect of medial malleolus (arrow).
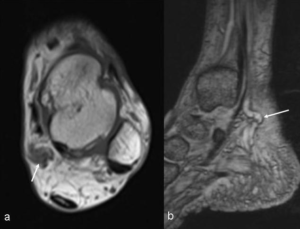
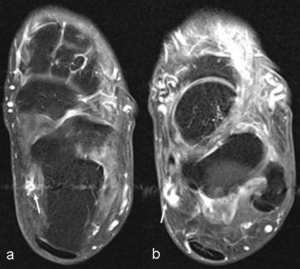
Figure2: The varix and dilated posterior tibial vein at level of tarsal tunnel.
a. Posterior tibial vein (arrow) is dilated and is strongly enhanced on gadolinium enhanced fat suppression T1 weighted axial image (TR/TE 518/20 ms, Thickness 3 mm, gap 03. mm and FOV 160 mm).
b. A varix is present just above of the tarsal tunnel (arrow). This varicose vascular structure is continued to posterior tibial vein on gadolinium enhanced fat suppression T1 weighted axial image.
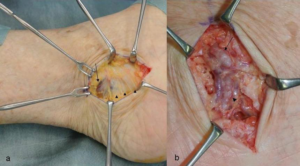
On surgical findings, the dilated posterior tibial vein got tighter under the retinaculum of tarsal tunnel (Figure 3a). Varices formations continued into the posterior tibial vein and were present at both superior and inferior aspect of the retinaculum. A surgical resection of the retinaculum was performed in order to decrease the pressure on the tarsal tunnel (Figure 3b). The patient’s symptoms reduced after surgery. However a few months later, he referred plantar numbness again.
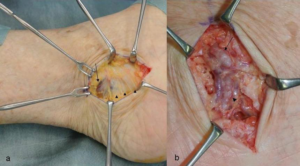
Figure3: Surgical findings of tarsal tunnel.
a. The varix (arrow) just above the tarsal tunnel is demonstrated. Thin superior retinaculum (arrowheads) is visualized.
b. Resection of the superior retinaculum was performed. The varix (arrow) is continued to the posterior tibial vein (arrowhead) under the superior retinaculum through communicating vein. These findings may suggest regurgitation of venous vessels from superficial vein to posterior tibial vein.
DISCUSSION
Various conditions have been suggested to play a role in the etiology and pathogenesis of a posteromedial tarsal tunnel syndrome. This syndrome can be idiopathic (in about 50% of cases) or associated with space occupying lesions including tumors, ganglion cysts from the subtalar joint or tendon sheaths, abnormal or accessory muscle (hypertrophic adductor hallucisor accessory flexor digitorum longus muscle,3,4 lipomas, varicose veins, trauma with bone spicule from an adjacent fracture, foreign bodies, iatrogenic causes such as calcaneal osteotomies with involuntary deep penetration medially, with fixation hardware or scar tissue.3,5
Tarsal tunnel syndrome may also develop in relation to some foot deformities such as valgus /varus deformity, pes planus and tarsal coalition. Systemic diseases such as diabetes, rheumatoid arthritis and peripheral arterial disease can play a role in this syndrome. The main symptoms of tarsal tunnel syndrome are represented by poorly localized paresthesia, dysesthesia and hypoesthesia in the medial and lateral plantar area. Symptoms are typically unilateral and rarely bilateral.6 Tarsal tunnel syndrome caused by varicosity may show characteristic symptoms: Kumai et al7 reported that patients suddenly feel foot pain whenever they soak a foot in hot water. This specific symptom occurs due to dilatation of the varicose vascular structures in the tarsal tunnel. Our patient had the same symptom thus supporting the hypothesis that the tarsal tunnel syndrome was caused by the varicose vascular structures compression.
Sato et al8 reported a frequency of tarsal tunnel syndromes caused by the varicose vascular structures of about 4% and in the literature they represent about 14% of the cases described.9 On the other hand, 43% of Japanese people (48 million people) over 15 years or older, have varicose vascular structures.10,11 Although there are many patients who have had widespread varicose veins, they are rarely complicated with a tarsal tunnel syndrome. It would be because the varicose vascular structures cannot cause a tarsal tunnel syndrome alone if they are not at the tunnel level. Varicose veins are also associated to flat foot and heel valgus: this condition creates a compression of the plantar nerves and can cause a tarsal tunnel syndrome as well. In addition, tarsal tunnel syndrome symptoms might be masked by other symptoms caused by the varicose vascular structures like legs and feet swelling, feet early fatigue, skin alterations and venous ulcers.12,13 We were able to diagnose the tarsal tunnel syndrome, but we should have treated the varicose vascular structures after the surgical resection of the retinaculum, in order to avoid a relapse of the tarsal tunnel syndrome as reported in the literature.13,14 Moreover, even the flatfoot deformity, which can play a role in the pathogenesis of the syndrome, should have been considered in the treatment strategy as well.
We first chose MRI to evaluate the tarsal tunnel syndrome because we initially suspected a space occupying lesions like ganglion cysts, but in this case we should have taken a contrast enhanced CT for the varicose vascular structures.
CONCLUSION
Tarsal tunnel syndrome can be caused by varicose vascular structures and patients who suffer from this syndrome may show characteristic symptoms. If varicose veins are in the tarsal tunnel and if a foot deformity is present a diagnosis of tarsal tunnel syndrome due to varicose vascular structures compression should be considered. In order to make a proper diagnosis, it is mandatory to evaluate the status of the varicose vascular structures at first. Treatment of the varicose vascular structures and correction of eventual foot deformity are recommended in association with a tarsal tunnel decompression.
CONSENT
The patient has provided written permission for publication of the case details.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.