INTRODUCTION
With the recent trend of obesity, strategies for implementing a nasal ventilation mask, as standard therapy for deep sedation are becoming increasingly important. The prevalence of obesity has doubled since 1980, and the Centers for Disease Control and Prevention report that more than two-thirds of U.S. adults older than 20-years of age are overweight and 35.7% are obese (BMI 30-40).1 Obese patients are at a further increased risk for hypoxemia during deep sedation due to a reduced functional residual capacity, increased oxygen consumption, and excess fat deposition within the lateral pharyngeal walls that results in a smaller than normal pharyngeal volume.2 The prevalence of obstructive sleep apnea (OSA) is estimated to be approximately 25%, and as high as 45% in obese patients, and the prevalence of OSA and its consequences are likely to increase in light of the current obesity epidemic.3
With increasing utilization of outpatient and minimally invasive procedures, moderate to deep sedation is becoming a more commonly used method of anesthesia.4 The ASA Committee of Standards and Practice Parameters recommends providing every patient with a continuous course of passive supplemental oxygen and continuously monitoring oxygenation and ventilation during moderate or deep sedation procedures.5 Unfortunately, recent prospective randomized controlled trials (RCTs) reported up to 54% of all patients experience severe hypoxemia secondary to sedation-related upper airway obstruction (UAO) and respiratory depression.1 The incidence is exacerbated by obesity and obstructive sleep apnea as independent risk factors with odds ratios 2-9 times that of normal weight patients.6,7
Although passive oxygenating devices have the ability to provide higher concentrations of oxygen, they are incapable of generating positive pressure, which is required in order to maintain airway patency and provide ventilatory support in the event of UAO and respiratory depression respectively.8 Pulse oximetry is a reliable indicator of oxygenation, but has limitations due to the averaging of values causing a delay in registering fluctuations as well as its inability to measure the patient’s ventilation status. Therefore, ventilation is best monitored using continuous waveform end-tidal CO2. Generally it reveals sedation-induced respiratory depression prior to desaturation on pulse oximetry.2 Thus, one can argue that end-tidal CO2 (ETCO2) is of greater importance in the setting of moderate and deep sedation. Although many passive oxygenating devices are equipped with CO2 monitoring, recent prospective RCTs have not shown an improvement in the incidence of severe hypoxemia despite the continuous monitoring ETCO2.8,9 Recently, high-flow nasal cannula (HFNC) has been used during moderate and deep sedation to improve oxygenation, however, ETCO2 can not be monitored with HFNC due the high flow of O2 causing dilution.10 Mitigating the risk for apnea and hypoxia with pharmacologic sedation while avoiding airway instrumentation requires a noninvasive device that provides adequate oxygenation and ventilatory support, protects airway patency, and allows for accurate ETCO2 monitoring.
A sealed nasal ventilation mask, the SuperNO2VATM (Vyaire Medical, Mettawa, IL, USA), meets these criteria by providing supplemental oxygen, and when connected to either an anesthesia circuit or hyperinflation bag generates positive pressure while allowing for ETCO2 sampling. The device maintains upper airway patency and ventilatory support, while delivering a high FiO2 at titratable positive pressures. Its ability to generate positive pressures to overcome UAO and airway collapse can reduce the need for endotracheal intubation and its associated complications. Furthermore, the ability to monitor ETCO2 provides timely detection of apnea, even at high-flow rates, due to it being a nearly closed system. We present this nasal ventilation mask as a new option for airway management because of its ability to maintain airway patency and provide sufficient oxygenation during procedural deep sedation in high-risk patients.
Description
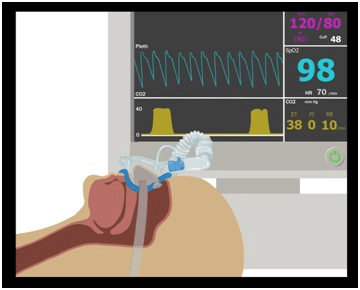
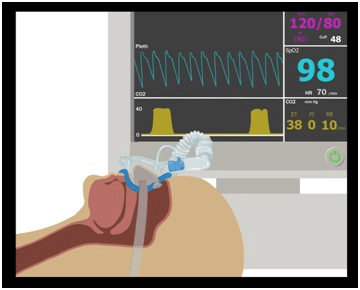
Ten (10) patients (5 men and 5 women; mean age 52) undergoing deep sedation procedures with propofol using the SuperNO2VATM nasal ventilation mask were reported from four different institutions. Nine of the 10 patients were obese with a BMI≥34.4, and all patients were at high-risk for or diagnosed with Obstructive sleep apnea (OSA). Patient history and basic demographic data were collected and their averages were calculated (Table 1). Standard ASA monitors were reported to be used on all patients. Standard practice for the use of the SuperNO2VATM device at these institutions is to secure it to the patient’s nose (Figure 1), connect it to either a hyperinflation bag or anesthesia circuit, set the oxygen fresh gas flow to 10 liters per minute, completely close the adjustable pressure limiting (APL) valve on the hyperinflation or set the anesthesia machine’s APL valve to 10 cm H2O and place the patient’s head in neutral position with their mouth closed. All patients received deep sedation by an anesthesia care team. Sedation-related complications that were reviewed and analyzed included hypoxemia (SpO2<90% for greater than 15 seconds), number of procedure interruptions or early procedure termination, and the use of a nasal airway (Table 2).
| Table 1. Demographics and Observations17,18,19,20 |
|
Case
|
n |
Age |
Gender |
BMI or Weight |
PMHx |
Procedure
|
Lowest SpO2 during the case
|
|
1
|
1 |
50 |
M |
47.2
|
Morbid obesity, OSA, HTN, HLD, HFpEF, asthma |
TEE for Electrocardioversion |
99.0%
|
|
2-7
|
6 |
28-69 (40) |
3 M, 3F |
104-180 (138) kg
|
Obesity, OSA(4 of the 6) |
EGD |
99.8%
|
|
8
|
1 |
56 |
F |
21.6
|
Crohn’s disease, HTN, asthma |
SVT Ablation |
100.0%
|
|
9
|
1 |
46 |
F |
34.4
|
Obesity, IDDM, PVD, CAD s/p MI, HTN, AF, ESRD |
AV Fistula Revision |
98.0%
|
|
10
|
1 |
69 |
M |
36.1
|
Morbid obesity, OSA, CAD s/p MI, PVD, NIDDM, Hypothyroidism |
AV Fistula Formation |
98.0%
|
Figure 1: Nasal CPAP Mask SuperNO2VATM in Use with ETCO2 Attached During Sedation
| Table 2. Observed Complications During the Cases |
| Complications |
n=10 (avg) |
| Lowest SpO2 |
98.0-100% (99.0%) |
| Incidence of hypoxemia |
0/10 (0%) |
| Procedure interruption/termination |
0/10 (0%) |
| Tracheal intubation |
0/10 (0%) |
Case 1
Patient is a 50 year-old morbidly obese (BMI 47.2) male with multiple comorbidities (Table 1) who presented for transesophageal echocardiography (TEE) and electrical cardioversion for persistent atrial fibrillation (AF). The patient was oxygenated with nasal cannula (NC) and sedated with titrated boluses of propofol. Five minutes into the TEE, the patient experienced upper airway obstruction (UAO) and desaturation to <85%. An OPA was inserted and the patient was ventilated with a bag-valve-mask. Secure placement of the SuperNO2VATM led to immediate mitigation of the airway obstruction and returned the oxygen saturation to 99%. Despite a successful TEE, cardioversion to normal sinus rhythm failed. The SuperNO2VATM was used when the patient returned for a second attempt cardioversion the next day. The patient was successfully cardioverted with no hypoxemic events.
Case 2-7
Six consecutive morbidly obese patients (3 male, 3 female) underwent upper endoscopic gastroduodenoscopy for pre-bariatric screening with deep sedation using the SuperNO2VATM. The average age and weight of the patients was 40 years and 138 kg respectively. Four of the patients had documented OSA with home-CPAP use. An anesthesiologist or certified registered nurse anesthetist (CRNA) managed the deep sedation with an appropriately dosed sedative. No hypoxemic events occurred and the average lowest SpO2 was 99.8%.
Case 8
Patient is a 56-year-old female who presented for repeat ablation for recurrent supraventricular tachycardia (SVT). After her first ablation attempt, she required an overnight CPAP. Due to her high risk for UAO with sedation, the SuperNO2VATM was incorporated into the anesthetic plan. The SuperNO2VATM was lightly secured to the patient’s face and oxygen flow was set to 10 L/min. Airway obstruction occurred upon initiation of a propofol infusion. By tightening the mask and creating a seal, the positive pressure generated immediately relieved the obstruction. No other adverse events occurred and oxygen saturation remained at 100% thereafter.
Case 9
A 46-year-old obese (BMI 34.4) female patient with multiple comorbidities (Table 1) presented for an AV fistula revision for dialysis graft. UAO occurred two months prior during AV fistula surgery with monitored anesthesia care (MAC), and an oral and nasopharyngeal airway was placed. One year prior, a tracheostomy was placed for prolonged mechanical ventilation. Due to her history of airway management, the pre-anesthetic plan included placement of the SuperNO2VATM prior to sedation with propofol. Oxygen saturation was maintained at 98-100% with positive capnography throughout the procedure and UAO did not occur.
Case 10
Patient is a 69-year-old morbidly obese male (BMI 36.1) with multiple comorbidities (Table 1) who presented for AV fistula formation for dialysis. The SuperNO2VATM was placed on the patient prior to procedural sedation. Deep sedation was maintained for 3-4 hours with titrated doses of propofol. Positive ETCO2 was monitored and oxygen saturation was maintained at 98-100% without incidence of UAO and hypoxemia.
DISCUSSION
This case series demonstrates the use of the SuperNO2VATM nasal ventilation mask connected to either an anesthesia circuit or hyperinflation bag as a noninvasive technique to maintain patient oxygenation and ventilation during deep sedation. All 10 patients underwent procedures requiring deep sedation with propofol, and each patient was at high-risk for severe hypoxemia secondary to sedation-related UAO and respiratory depression. Nine of the 10 patients were obese with a BMI≥34.4 (Table 1), and all patients were at risk for or diagnosed with OSA. With the SuperNO2VATM securely placed, 0/10 patients experienced UAO and the lowest oxygen saturation was 98.0%. Airway patency was maintained in all 10 patients and the procedures were performed without interruptions. Table 2 summarizes the total number of complications. The results from this case series indicate that the use of a nasal ventilation mask connected to either an anesthesia circuit or hyperinflation bag is a safe and effective noninvasive ventilation technique to maintain airway patency and ventilation in patients at risk for airway obstruction and respiratory depression during deep sedation.
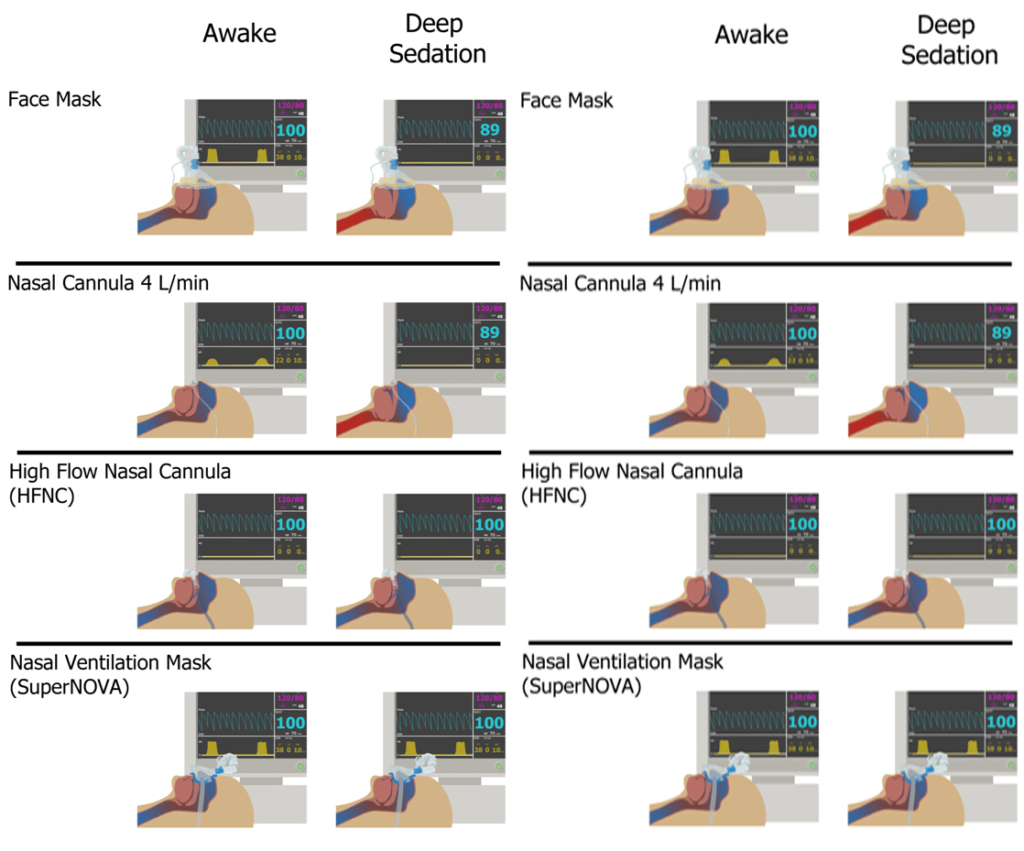
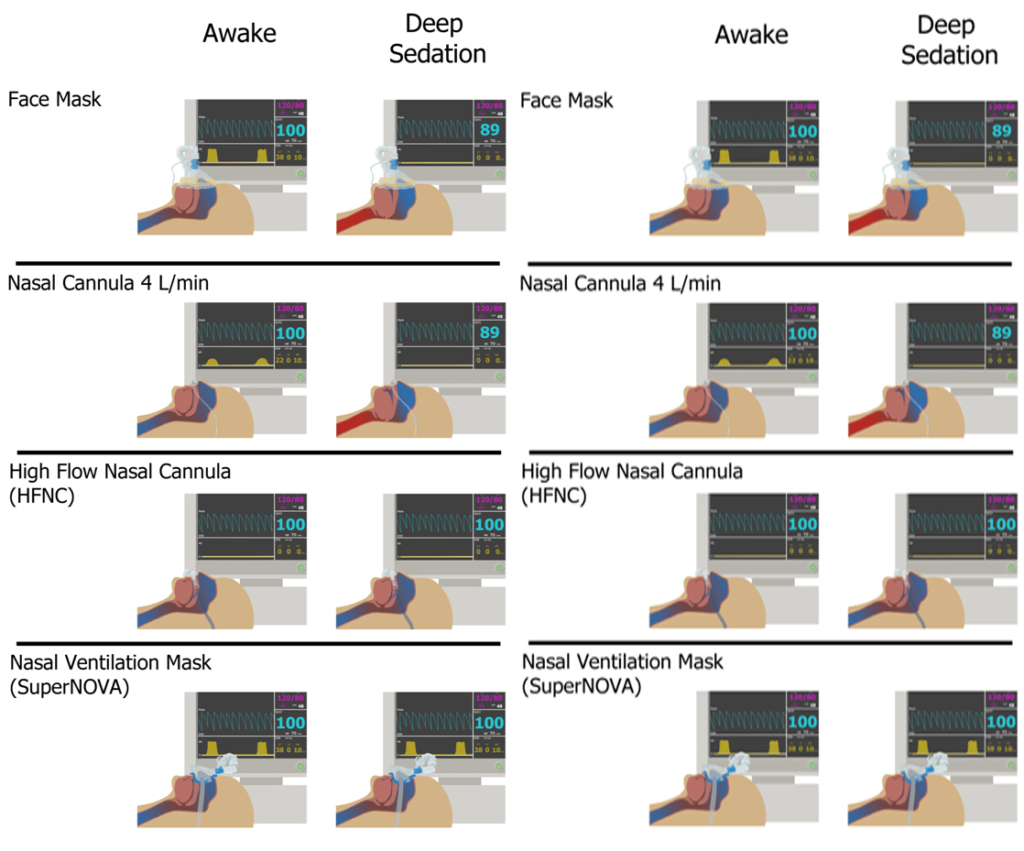
In today’s practice, anesthesiologists and nurse anesthetists depend on passive oxygenating devices to provide adequate oxygenation and ETCO2 monitoring to ensure ventilation in patients under moderate and deep sedation. However, these devices are incapable of establishing a patent airway in the event of UAO, occurring in up to 54% of all sedated patients.3 HFNC has been supported in literature for relieving airway obstruction, though its utility is limited by a lack of ETCO2 monitoring.11 The direct measurement of exhaled CO2 is essential for the early detection of airway obstruction, and its absence should not be considered inconsequential. For this reason, the interest for advanced respiratory monitoring during deep sedation, particularly capnography, is emerging. A nasal ventilation mask that creates a seal, generates continuous positive pressure when connected to either an anesthesia circuit or hyperinflation bag, and monitors ETCO2 presents as a novel, noninvasive approach for ensuring adequate oxygenation and ventilation in any patient at risk for airway obstruction and respiratory depression. For a conceptual comparison of the clinical use and limitations of these devices see Figure 2.
Figure 2: Comparison of Face Mask, Nasal Cannula, High Flow Nasal Cannula and Nasal CPAP mask SuperNO2VATM as Used in Patients when Awake and Undergoing Procedural Sedation. Note the Differences in Upper Airway Support and Ability to Capture ETCO2 Monitoring
Non-invasive ventilation has grown in popularity in recent decades and has become well-established in the management of acute respiratory failure. Non-invasive techniques avoid complications associated with tracheal intubation in mechanically ventilated patients.12 The replacement of invasive ventilation in conditions where a non-invasive approach is more appropriate has decreased rates of airway trauma, aspiration, intubation, and overall mortality.13 The safety and efficacy of noninvasive ventilation during procedural deep sedation is not well known and further studies are needed to clarify its impact on intubation and mortality rates.14 Therefore if airway obstruction occurs in this setting, tracheal intubation is seen as an appropriate option, especially since the non-invasive devices available aren’t designed to rescue an airway. The results from this case series may suggest that implementation of a nasal ventilation mask, such as the SuperNO2VATM, in patients requiring deep sedation has the potential to prevent unnecessary tracheal intubation and its related complications.
To further report on the significance of the SuperNO2VATM, we must discuss why nasal ventilation may be superior to nasal-oral ventilation. First, a nasal ventilation mask allows unobstructed access to the oral cavity for intraoral procedures in contrast to a traditional full face mask. Second, the solid and immobile structures surrounding the nasal cavity permit a better seal for generating positive pressures, when compared to the soft tissue and mobile structures surrounding the oral cavity. Furthermore, understanding the anatomy involved in airway obstruction will support the favorability of nasal ventilation. Studies have shown that the source for airway obstruction in most patients during deep sedation is the tongue falling against the soft palate which falls against the retropharyngeal wall.15 Applying positive pressure to the oral cavity via a traditional face mask will force the tongue back into the airway, contributing to the obstruction. In contrast, the positive pressure generated from a nasal ventilation mask will force the tongue and soft palate forward off the retropharyngeal wall, aiding to alleviate the obstruction. A previous study using MRI demonstrated that a nasal CPAP can double pharyngeal volume and serve as a pneumatic splint to alleviate airway obstruction.16 These are some of the reasons why a nasal ventilation mask is preferred.
This case series suggests a role for nasal ventilation mask in the setting of procedural deep sedation during the procedures discussed. However, the nasal ventilation mask may be applicable to other clinical settings. The advantages illustrated by the cases discussed suggest that nasal continuous positive airway pressure (CPAP) may be efficacious in the operating room, post-anesthesia care unit (PACU), intensive care unit (ICU), or emergency room. Studies that demonstrate the use of the SuperNO2VATM in the operating room during the process of securing a difficult airway, or attaching the SuperNO2VATM to a hyperinflation bag for transport to the PACU have already been reported.21 The observations of this case series are encouraging, and suggest that a pressurized nasal ventilation mask may be a preferable alternative to improve oxygenation and ventilation in high-risk patients during deep sedation. These observations are promising, yet randomized clinical trials are needed to demonstrate the superiority of a nasal ventilation mask in preventing hypoxia during moderate and deep procedural sedation.
CONSENT FOR PUBLICATION
Consent for publication was obtained from all the patients described in this case series.
FINANCIAL DISCLOSURES
Drs. Foley and Feinleib both report that they are on the medical advisory board of Vyaire Inc. for which they receive compensation.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.