INTRODUCTION
The use of computed tomography (CT) has increased exponentially since its introduction into the clinical setting in 1971.1 This growth comes as a consequence of numerous technological advances, namely multi-detector capabilities, which have seen CT move to the forefront of medical imaging.2 Consequently, the expansion of CT has raised concerns regarding radiation exposure and patient-induced health risks.3 CT contributes to a large portion of the population’s radiation exposure, subjecting patients on average to higher doses than its medical imaging counterparts.4 It is these considerably higher doses that are fuelling concerns regarding the lifetime attributable chance of fatal malignancy, estimated to range from 25 to 33 cases per 100,000 for pelvic, abdominal and chest CT procedures.5
Additionally, concerns exist regarding the dose received by radiosensitive organs, specifically the thyroid, breast, gonads and lens of the eye. These organs are made up of radiosensitive cells and are regarded to have a greater stochastic risk of future malignancy with repeated exposure to ionising radiation.6 It is therefore important that all CT examinations are justified and implement practical and reliable dose reduction techniques.
In the past, lead shielding was the leading dose reduction strategy used in CT examinations.7 However, its use was replaced by bismuth shielding, which provided improved opportunities to reduce dose to superficial organs within the field of view.8 While various studies have proven that lead and bismuth provide equivalent dose reductions9,10,11; bismuth shields are designed for specific superficial organs and have the added benefit of being lightweight and easy to manoeuvre.8
Recently, the use of bismuth shields has sparked debate in relation to issues caused during scans. According to the American Association of Physicists in Medicine (AAPM), these issues relate to the degradation of image quality, unpredictable and unreliable results when combined with automated exposure control (AEC) and wasted radiation.9 The most recent position statement released by the AAPM states that ‘other technologies exist that can provide the same level of anterior dose reduction at equivalent or superior image quality that do not have these disadvantages’.9 These alternative methods include, but are not limited to, organ-based and global tube current modulation and iterative reconstruction techniques, which should be considered and applied when possible.
The purpose of this literature review is to explore current available knowledge in an attempt to determine the most effective technique to reduce dose to radiosensitive organs during CT examinations. The main focus will be placed on evaluating the current clinical use and effectiveness of bismuth shielding. Furthermore, alternative and emerging dose reducing strategies will be investigated in an attempt to help guide contemporary practice.
MATERIALS AND METHODS
A systematic review is a thorough evaluation of the literature and is a key element of evidence-based practice. It involves identifying and selecting relevant studies, appraising their quality and summarising the evidence using explicit methodology, in order to address and provide a non-biased and reliable answer to a formulated question.12 Systematic reviews are most suited in situations where there is an inconsistency in research methodology causing unreliable results or when a body of research exists; however, findings are not well consolidated. The systematic review aims to organise research findings into themes so future research is focused and valid.13 There are various recognised approaches that guide the systematic review process.12,13,14 The guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were implemented for this review.14
Evidence was found by conducting a PubMed and Scopus search to obtain literature regarding the use and effectiveness of bismuth shielding in CT. Key words included: ‘Bismuth shielding’ OR ‘shielding’ AND ‘CT’ OR ‘computed tomography’ AND dose-reduction. The searches were limited to the English language, with a publication date from 2010 onwards.
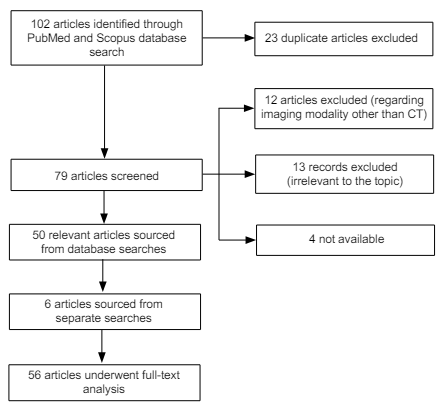
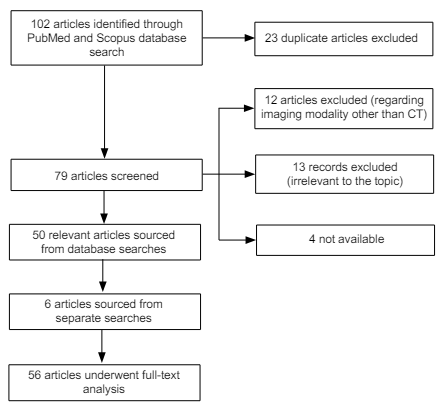
This method resulted in a combined total of 102 articles, which were subsequently subject to a thorough screening process, as per the PRISMA guidelines (Figure 1). Titles and abstracts were carefully assessed according to inclusion and exclusion criteria (Table 1). Twenty-three duplicate articles were removed, as well as 29 articles found to be either completely irrelevant or outside the scope of this review, not available or regarding another medical imaging modality other than CT.15
Figure 1: Flowchart Demonstrating the Screening Process.
| Table 1: Inclusion and Exclusion Criteria. |
|
Inclusion
|
Exclusion
|
● Published between 2010 and present
● English language
● Peer-reviewed
● Reliable source
● Studies assessing the current use and effectiveness of bismuth shielding in CT, including at least one of the following:
○ Dose reduction capabilities
○ Impact on image quality ● Studies discussing alternative and emerging does reduction strategies in CT
● Studies regarding does reduction in CT specifically to radiosensitive organs; particularly the breast, thyroid, gonads and lens of the eye. |
● Published before 2010
● Not accessible
● Articles discussing:
○ Shielding and other does reduction techniques in medical imaging modalities other than CT
○ Does reduction to others beside the patient (e.g., staff)
○ Room shielding
○ Topics completely irrelevant |
Additionally, six publications were included that were outside the scope of this search; sourced from recommendations, separate searches and backtracking of articles. Overall, the study sample included 56 relevant articles that were thoroughly assessed and evaluated, to help provide the answers to the clinical question.
RESULTS
There is a well-established and justifiable need to modulate the radiation exposure to radiosensitive organs.16 For the purpose of this review, four organs: The eye lens, thyroid, breast and gonads, were identified and the effect of bismuth shielding on dose reduction and image quality evaluated.
The image quality parameters discussed in the papers cited in this article include image noise, signal-to-noise ratio, artifacts such as beam hardening. Image noise refers to the random variation of CT numbers and depends on both the quality (beam energy) and quantity (number of photons) of the X-ray beam. Noise has a grainy appearance on images. The signal-to-noise ratio (SNR) on the other hand is a ratio of the true signal (from anatomical structures) to the random quantum mottle (noise).
An artefact is an error on the image that is not related to the anatomy being examined and can mask or mimic clinical characteristics. Two such artefacts that are noted in this paper are:
1. Streak artefacts;
2. Beam hardening artefacts.
While Beam hardening refers to an increase in the mean energy of the X-ray beam as it passes through the patient and appears as shading differences on the image; streak artifacts appear as bright straight lines across the image, and could be caused by the presence of metal in/or on the patients for example. For more details of these artifacts the reader should refer to related articles which will be cited below.
THE EYE LENS
Dose Reduction
CT examinations of the head are among the most frequently performed CT examinations, with a typical radiation dose of 60 mGy.17 Although the eyes are rarely the area of interest during such examinations, they are often incidentally included within the scan region. This is an area of concern as the eye lens is one of the most radiosensitive organs in the human body.17-24 According to the International Commission on Radiological Protection (ICRP), the radiation dose threshold for detectable lens opacities resulting in the formation of cataracts is 0.5 Gy.18,19 Therefore it is prudent that dose reduction strategies are implemented.
There are several studies in the literature that evaluate bismuth shielding as a dose reduction method.17-25 Where as all studies report a reduction in dose to the eye, the dose savings vary from 20 to 50% depending on the scanner, technique and shield design. Mendes et al23 conducted a study using an acrylic head phantom to evaluate the dose reduction achieved with and without the application of a bismuth shield covering the eyes. The percentage dose reduction achieved was 36%, verifying the dose reduction capabilities of bismuth eye shields.
Additionally, a study by Wang et al17 investigated the effect of increasing the thickness of the bismuth shield. This involved scanning an anthropomorphic head phantom using both a single-layer and double-layer of bismuth shielding. The dose reductions achieved were 26.4% and 42.4%, for the single and double-layered shield, respectively. While this study confirms that multiple layers of bismuth increases dose reduction, image quality is compromised in the process, limiting the acceptable thickness and thus, dose reduction capabilities of the shield.
Since it is not possible on many scanners, the literature suggests that when feasible, excluding the eyes from the primary X-ray beam by tilting the gantry along the supraorbital meatal line is the most effective way to reduce dose to the eye lens.17,18 Studies have reported dose savings of around 80%.18 Concerns have been raised; however, regarding streak artifacts as a result of beam hardening and partial volume artifacts, as well as reconstruction pitfalls.18,26,27
Image Quality
All these shields have proven to provide invaluable dose reductions to the eye lens, their use and effect on image quality remains under debate. Numerous studies have recommended against the use of bismuth shielding due to the presence of streak artifacts extending into the brain, affecting mainly the orbits, inferior frontal lobe and anterior temporal regions.19,24 In some cases, these artifacts have resulted in images unsuited for diagnostic purposes, with repeat scans required.19,21
Furthermore, the application of bismuth causes beam hardening and poor use of information-carrying photons, resulting in increased image noise and inaccurate CT number representation. Several studies have shown a drift in CT numbers between 50 and 65%.25,26,28
There are also many studies that support the use of bismuth, suggesting no significant impact on image quality.19,20,28 Where as these studies agree that streak artifacts disrupt image quality, the majority suggest that by creating a small gap between the eye lens and the shield, artifacts can be reduced to an acceptable diagnostic level.9,17,19,24,26 Our study by Raissaki et al24 reduced artifacts to a negligible level by elevating the shield from the eyes using folded gauzes. Distances of 5, 10 and 20 millimeters were evaluated and found to reduce artifacts resulting in only slight decreases to dose reductions. Dose savings of 32%, 30% and 29% at five, 10 and 20 millimeters, respectively were recorded, compared to the 32% dose reduction following direct placement of the shield.
THYROID
Dose Reduction
According to the ICRP the radiosensitive thyroid gland has a tissue-weighting factor of 0.04, meaning an increased risk of stochastic injury and future malignancy with exposure to ionising radiation.23 Although rarely an organ of interest, the thyroid gland is often incidentally exposed to the primary X-ray beam during neck and thorax CT examinations. Therefore, because of its radiosensitive nature and frequent radiation exposure it is important that the dose to the thyroid is limited.
Catuzzo et al20 conducted a study to investigate the dose reduction capabilities of bismuth thyroid shields. This involved dose measurements calculated using thermoluminescent dosimeters on both phantoms and patients, with and without bismuth shielding. They recorded 32.16% and 30% 10% dose savings on phantoms and patients, respectively. These measurements correspond well with several other studies in the literature that report reductions between 25 and 40%.6,23,30,31
Another study performed by Inkoom et al32 explored the effect of combining bismuth shielding with AEC. The authors examined the effect that bismuth shielding, AEC and a combination of the both had on the dose to four pediatric anthropomorphic phantoms. Dose reductions increased from 25% with bismuth alone, to 62% when combined with AEC. Use of AEC with bismuth must be considered carefully; however, due to unpredictable and unreliable effect on image quality.
Image Quality
As stated earlier, the use of bismuth shielding in CT is associated with the presence of beam hardening and streak artifacts.32 While some studies disprove of the use of bismuth in thyroid CT examinations because of the degradation of image quality caused by such artifacts,30,31 others conclude no quantitative or qualitative impact on image quality.6,21,31
A key issue associated with thyroid shields is the negative impact on CT attenuation values. Our study by Lee et al31 recorded increases in CT numbers in the superficial neck muscles. These results suggest the use of bismuth shields must be carefully considered as they may degrade the diagnostic accuracy of an image.
BREAST
Dose Reduction
Radiation protection of the breasts in female patients during CT examinations is important for two main reasons. Firstly, female glandular breast tissue has increased radiosensitivity, with an associated tissue-weighting factor specified by the ICRP of 0.12.5,19,33 Secondly, the breast is often incidentally exposed to large doses of radiation during CT procedures, even though they are rarely the area of interest.34,35 Although routine chest CT scanning contributes to the majority of breast irradiation, numerous examinations are of concern. For example, CT pulmonary angiography can result in a mean glandular dose between 20-60 mGy, where as the inferior aspect of the breast can receive 10- 20 mGy during abdominal CT.5Therefore because of the breasts overall projected radiosensitivity and high incidence of irradiation, reliable and practical dose reduction techniques must be routinely implemented.
The vast majority of publications relating to the use of bismuth shields in CT confirm its ability to produce considerable dose reductions to the breasts. These studies suggest dose savings ranging from 20 to 60%, depending on patient type, scanner, shield design and protocol used.34-40 Catuzzo et al20 reported a breast dose reduction in female patients during a routine chest CT of 41%, Abadi et al42 recorded a 38.4% reduction during CT angiography scans of a phantom and Small et al43 produced dose savings of 62% during cardiac CT scanning when combining the use of bismuth shielding with ECG-gated tube current modulation. Additionally, there are numerous studies that report dose reductions to the breast of around 30% on paediatric phantoms.22,28,37,47
Image Quality
The widespread use of bismuth breast shielding is limited by many conflicting ideas regarding image quality. There are various studies that advocate the use of bismuth shielding for breast dose reduction suggesting acceptable deterioration in image quality with no impact on interpretability.5,20 One study performed by Einstein et al44 investigated the use of bismuth shields during CT coronary angiography examinations and observed no streak artifacts, whilst a separate study by Colletti5 reported no significant impact on signal-to-noise ratio or image quality.
These findings however, are contrasted against several studies in the literature that are against the use of bismuth breast shields.5,35,46 Several of these studies report significant increases in image noise.5,35,41 Wang et al39 showed image noise in both the heart and lung, with increasing noise closer to the shield, where as the study by Einstein et al44 showed increased noise affecting coronary artery visualisation. Investigators have also reported the presence of undesirable streak and beam hardening artifacts.19,30 Furthermore, evidence exists regarding changes in CT numbers within the heart and lung regions.39,44,46 These studies suggest that such a drift in CT numbers has adverse effects on plaque characterisation and coronary artery calcium scoring.
GONADS
Dose Reduction
The gonads are a radiosensitive organ not commonly targeted during CT imaging; however, they are exposed to radiation as a consequence of their anatomical location.48 Despite this, there is very little research into the use of bismuth shielding to protect the gonads. Sancaktutar et al49 recently performed a study on two hundred male patients. They investigated the dose savings that resulted when using 2 bismuth-lined gloves to protect the scrotum during abdomniopelvic CT examinations. This bismuth testes shield produced dose savings of 90.2%. Additionally, an older study using bismuth shielding on a phantom, resulted in a mean dose reduction of 50.5%.50 Whilst these studies confirm the dose saving capabilities of bismuth, further research is recommended to verify these findings and investigate the effect on image quality
The majority of CT dose reduction research in relation to protecting the gonads from ionising radiation is in relation to ‘out-of-plane’ lead shielding. This refers to the application of conventional lead aprons or custom-designed lead shields, to the pelvic region during CT examinations where the gonads remain outside the scan region. Several studies have investigated such techniques during CT examinations of the chest.29,51 These studies yielded dose savings between 70 and 90%. This technique involves the risk of causing severe artifacts if the lead is placed within the scan plane, the recommendation to protect anatomy lying outside the scan plane from scatter radiation using lead has proven viable.
DISCUSSION
The Argument for Bismuth Shields
Bismuth shields are commercially available, relatively inexpensive, require little training to implement correctly, are lightweight causing minimal discomfort and are simple and convenient to use.20,28,32,52 They function independently and thus can be used on all CT scanners from differing manufactures.35 Furthermore, they are associated with making the patient feel comfortable and confident when being exposed to ionising radiation.16
The primary argument supporting the use of bismuth shields in CT is their unquestionable ability to reduce dose to superficial radiosensitive organs. The literature reveals a consistent agreement regarding their effectiveness, with one study by Akhlaghi et al48 showing that even small thicknesses of bismuth result in significant dose reductions.
Further support for the use of bismuth shields comes from numerous statements from professionals suggesting bismuth shielding has a negligible effect on image quality.20,40,46,48,53 The majority of these reports come from studies that offset the shield from the patient. One study by Inkoom et al32 showed noise reductions of 69%, 87% and 92% when separating the shield from the patient by 1, 2 and 3 cm, respectively, using a cotton spacer. Other studies report that shielding causes negative impacts on image quality, these effects only occur in the superficial tissues, which are rarely the area of interest.16,20,48
Additionally, Samei16 claims that bismuth shielding allows controlled dose and noise manipulation to occur within a limited region of the body and thus allows effective dose reductions to organs not commonly of interest and thus where a tolerable enhancement of noise is permitted at no compromise to the overall diagnostic quality of the image. All of these claims supporting the use of bismuth shielding in CT coincide with the limited evidence in literature reporting a missed diagnosis as a result of bismuth.52
The Argument Against Bismuth Shields
Despite the dose reduction capabilities of bismuth shields, there are numerous studies that discourage their use.5,17,18,29,39,52 According to several publications5,34,54 bismuth shields are costly, time consuming and increase the risk of patient contamination if the shields are used multiple times without appropriate infection control procedures. Furthermore, in reference to the position statement issued by the AAPM, there are three main disadvantages with the use of bismuth shields: Adverse effects on image quality, unpredictable and undesirable results when combined with AEC and wasted radiation.
Bismuth shields are associated with disrupting image quality and CT number accuracy. Significant increases in image noise have been reported in superficial tissues, decreasing with depth into the patient.33,55 Whilst numerous studies have suggested introducing a space between the shield and patient eliminates this effect, one study by McCollough et al43 on the effect of bismuth breast shields, showed an increase in noise within the thorax, even with a 6 cm offset.
Further, effects on image quality result from beam hardening and streak artifacts caused by the attenuation properties of the shield.32,33 In numerous studies, the presence of these artifacts has resulted in a negative impact on the accuracy and quantitative measurement of CT numbers.16,29,52 One study by Goldin et al56 quantitatively analyzed the attenuation effect of bismuth shielding on a solid water phantom during CT chest scans. They reported a drift in CT number of up to 50.6 Hounsfield Units (HU) near the surface of the phantom, with changes decreasing with increasing distance from the shield. This effect could lead to possible mischaracterization and misdiagnosis of a variety of pathologies, strengthening the argument against bismuth shielding, especially when quantitative assessment of CT numbers is critical for diagnosis.
A second concern is associated with the use of bismuth shielding in conjunction with AEC. AEC adaptively modifies the scanners output based on patient attenuation, increasing x-ray flux when encountering an area with higher attenuation.16 As the combination of bismuth shielding and AEC has been reported in various studies to improve dose reductions,2,6,43 the technique is associated with unpredictable and undesirable effects on dose and image quality when used inaccurately.9
The majority of CT scanners use AEC algorithms based on the scout image acquired prior to the CT acquisition.57 If the shield is placed on before the scout then the system will increase the tube current based on increased attenuation from the shield, meaning a possible increase in both organ and total patient dose.16 A study by Colletti et al,5 revealed placing the shield before the scout during a chest CT, increased dose to the central breast by 29% and dose to the total patient by 20%. Additionally, the use of bismuth shields in CT systems where the AEC algorithm is modulated during the CT scan is strongly discouraged as the system continuously increases tube current in response the shield, counteracting its intended benefit.52
Finally, the use of bismuth shielding is considered to be ineffective for use in radiation protection of patients.18,33,57 Bismuth shields attenuate the anteriorly orientated X-ray beam, they also attenuate the posteriorly orientated beam that has already traversed through patient.16,17 This means that the information-carrying photons that have entered posteriorly and have deposited dose in the patient, are attenuated by the shield and are unable to reach the detector to contribute to image formation. DeMaio et al29 reported a loss of data up to 50%.
Alternative Techniques
With so many conflicting ideas concerning the use of bismuth shields, emphasis in current research has been placed on alternative dose reduction strategies that attempt to optimise both dose and image quality during CT procedures. This trend is in line with the current AAPM statement suggesting ‘other technologies exist that can provide the same level of anterior dose reduction at equivalent or superior image quality that do not have these disadvantages’.9The most promising alternative techniques include organ-based tube current modulation (OBTCM), global tube current modulation and iterative reconstruction algorithms.
Organ-Based Tube Current Modulation
This technique involves reducing the tube current during a 120° radial arc over the anterior aspect of the patient, and increasing the tube current within the remaining 240-degree arc. This modulation keeps the overall radiation dose constant while reducing direct exposure to anterior radiosensitive organs.3 One study by Nikupaavo et al6 used OBTCM on phantoms to reduce dose to the lens during head CT and reported 32% dose reductions. Similarly, Kim et al34 reported dose reductions of 20.8% to the superficial breast tissue and 18.8% to the deep portion of the breasts, using OBTCM on female patients undergoing routine chest CT examinations.
Despite these dose saving capabilities however, OBTCM has been shown to increase dose to posteriorly and laterally located structures.58 Research by Hoang et al6 reported dose increases of 29% to the upper lungs and 15-20% to spinal bone marrow, Also noting smaller increases in dose to the posterior brain. With such varying influences in dose, the use of OBTCM must be carefully considered.
Additionally, it is important to consider the image quality effects of OBTCM. The majority of studies report no degradation of image quality,6,29 with one study by Wang et al17 reporting no streak artifacts and no significant impact on image noise or CT numbers. Despite this support however there are several reports identifying an increase in image noise. Nikupaavo et al6 described increases in image noise of 30%, 29% and 12% in the posterior, central and anterior regions of the brain respectively, when using OBTCM during routine head CT scans.
There are also many additional concerns with the use of OBTCM. Kim et al34 raised concerns relating to the influence of patient anatomy, stating that in patients with larger breasts a portion of the breast tissue may fall within the lateral scan region, where an increased tube current would result in an increased amount of dose to the breast. Furthermore, if the patient is positioned off-center than radiosensitive organs could potentially receive more dose from the increased tube current portion of the rotation.40,59 Lai et al59 reported an increase in dose of 18% to the eye lens and 50% to the breast dose when positioning a phantom off-center during CT scans using OBTCM.
Global Tube Current Modulation
This technique involves reducing the tube current over the entire 360-degree rotation, decreasing the radiation dose not only to radiosensitive organs, but also to the entire scan region.5,34 Compared to bismuth shielding, globally reducing the tube current causes equivalent does reductions to radiosensitive organs,17,39,45 with the cost of slight decreases in image quality. This occurs as reducing the tube current inevitably leads to an increase in image noise.57 Numerous studies, such as that performed by Wang et al17 recorded increased noise within the anterior and central areas of the brain, along with minor but significant increases in noise to the posterior regions, when globally reducing the tube current during routine head CT scans. Despite this, reports suggest no streak artifacts or changes in CT numbers.17,34
Additionally, globally reducing the tube current during low-dose CT examinations should be avoided, as further reducing the tube current will increase the risk of producing diagnostically unsuited images.34 Overall, if a slight increase in image noise is acceptable for diagnosis, than globally reducing the tube current is superior to bismuth as it produces similar dose savings with no impact on CT numbers and no additional steps required to position and clean the shield.
Iterative Reconstruction Algorithms
Adaptive statistical iterative reconstruction (ASIR) is an example of one such iterative reconstruction algorithm. It is a complex and computationally demanding method of image reconstruction. It uses recent advanced mathematical models to reduce noise, thereby allowing high quality image acquisition at a lower tube current, thus enabling significant reductions in dose.3,8,37 There have been numerous studies recently aimed at evaluating the effectiveness of ASiR as a dose reduction method. One study by Mathieu and Cody35 used ASiR on a phantom during a routine chest CT and noted dose reductions ranging from 30% to 44%. These results are consistent with similar studies in the literature reporting dose reductions of 32-65%.37
Furthermore, the majority of studies agree in regards to the effects of ASiR on image quality. A study by Nikupaavo et al18 found ASiR reduced noise by approximately 20% and had no significant effects on CT numbers. Additionally, Kim et al60 investigated the effect of combining ASiR with the use of in-plane bismuth shielding and noted both reduced radiation dose and reduced bismuth induced noise increases. In general, ASiR has recently become commercially available and although comes at a financial cost due to software and hardware upgrades, is a promising alternative to the traditional filtered back projection that has the potential to create significant dose savings.37
CONCLUSIONS
This manuscript performed a systematic review of current literature to evaluate the use and effectiveness of bismuth shielding as a dose reduction method in contemporary CT practice. The analysis revealed that since bismuth shielding proves to provide significant dose reductions to radiosensitive organs, conflicting ideas exist regarding its ability to produce consistent diagnostic images. These findings are consistent with the current AAPM statement suggesting that alternative methods such as tube current modulation and iterative reconstruction algorithms can provide equivalent dose savings to radiosensitive organs at superior image quality, without the disadvantages of bismuth shields.
Where as numerous studies exist regarding these alternative methods, further research aimed at assessing their use and effectiveness is required in order to encourage their widespread application. Currently, tube current modulation and iterative techniques are not available on all CT scanners. Although these techniques should be considered and applied when possible, until further research and standardised equipment becomes available in all departments, in-plane bismuth shielding remains a viable option.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.