CASE STUDY
A 30-year-old female who presented twice to the emergency department separated by 2-weeks with complaints of right flank and suprapubic abdominal pain, dysuria, fevers, nausea, and vomiting. In the initial emergency department encounters she was diagnosed with a urinary tract infection and presumed pyelonephritis and started treatment with ciprofloxacin. She had a resolution of her symptoms over the course of 10 days of treatment; however, upon completing the course of her antibiotics her symptoms reoccurred. Her past medical history is notable for a kidney stone diagnosed 8-years ago at the time of pregnancy. She subsequently endorses approximately 3 urinary tract infections yearly, some with right flank pain, that have been treated with outpatient antibiotics. She reports that her current symptoms are similar to those events, however, her pain is more severe. She denies any family history of kidney stones, and her only other past medical history is mild asthma.
Upon arrival to the emergency department on her second visit she was found to be afebrile and tachycardia at 127-bpm with a normal blood pressure in moderate discomfort.
Physical examination demonstrated suprapubic and severe right-sided costovertebral angle (CVA) tenderness to palpation.
While universal guidelines for management of recurrent urinary tract infections and pyelonephritis are not comprehensive the use of imaging by computed tomography (CT) scan is advocated consistently.2 Etiologies for recurrent pyelonephritis include obstructive process such as kidney stones, Xanthogranulomatous pyelonephritis (XGP) or vesicoureteral reflux. These require specialized treatment and generally will not respond completely to antibiotics. Additionally, antibiotic choices for the emergency medicine physician should be based on the patient prior cultures, co-morbidities, clinical condition and local antibiogram for urinary pathology to name a few factors. Appropriate emergency department management of concomitant conditions, discomfort and dehydration may also be indicated. XGP can present with vague non-pathognomonic symptoms of flank or abdominal pain, fever and anorexia and dysuria. It is frequently associated with anemia, seen in 66-100%, leukocytosis, 61-90%, and in up to 35% of cases pyuria is absent.3-7 Suppuration of kidney tissue results from abnormal macrophage response to infection resulting in necrosis, lipid accumulation, and vascularized granulation tissue formation. This tissue is characterized by lipid-filled macrophages lending it the yellow (Xantho) hue on gross pathology.
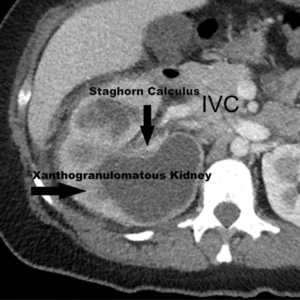
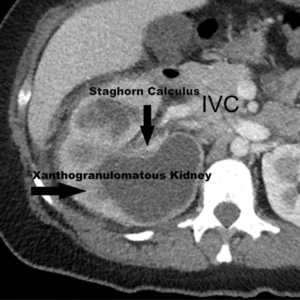
CT is the diagnostic modality, which was delayed in our case, and shows most frequently an enlarged kidney, sometimes with the Bear’s Paw Sign of dilated caliceal spaces, often with poor cortical perfusion and an associated renal stone.6 Differential diagnosis includes renal carcinoma, non-XGP chronic pyelonephritis, and renal tuberculosis. Untreated may lead to invasive spread, fistula formation, and systemic infection.1,5,7-8
In this case, the complete destruction of the kidney resulted in nephrectomy complicated by inflammation of the liver and vena cava. Other known complications of XGP such as inferior vena cava thrombus, septic emboli, abscess, and fistula formation may be avoided with rapid diagnosis and treatment.9-10
A CT scan was obtained upon the patient’s second visit to the emergency room, with the radiology reading of: “diffusely enlarged kidney with multiple low attenuation areas throughout the renal parenchyma. There is a large staghorn calculus. Findings are consistent with XGP (Figure 1).”
Figure 1: Computed Tomography Abdomen and Pelvis.
A subsequent outpatient cystourethroscopy and right retrograde pyelography was attempted but was unsuccessful.
On the first and second emergency department visits the patients WBC count and urinalysis was 17000 and 12000 with bacteria pyuria and no bacteria or pyuria respectively.
A urine culture obtained from the patients first emergency department visit revealed >100,000 colonies/ml of pansensitive Pseudomonas aeruginosa.
The patient was treated in the emergency department with IV fluids for presumed dehydration and pain control. She was started on continuous antibiotics to reduce bacterial load, evaluated by urology who concurred with concern for Xanthogranulomatous pyelonephritis and follow-up with them was arranged 1-week later.
The diagnostic imaging was obtained and the diagnosis of presumed Xanthogranulomatous pyelonephritis was made. She continued on the ciprofloxacin with the resolution of her symptoms as an outpatient. A cystourethroscopy, right retrograde pyelography was attempted 2-weeks after presentation to the emergency room; however, it was unsuccessful due to inability to pass the Pollack catheter passed the renal calculi. The patient remained on antibiotics and after another 2-weeks a right-sided laparoscopic robotic-assisted nephrectomy was performed, which was complicated by inflammation and adhesions to the surrounding structures including the liver and vena cava.
Pathology showed a 10 by 6-centimetre kidney with “multiple cystic spaces filled with yellow pus-like fluid, with tan-white chalky stones (up to 1.5 cm in greatest dimension)” with histology showing a final diagnosis of Xanthogranulomatous pyelonephritis.
Patient recovered well and continued follow-up with urology with yearly ultrasounds to her remaining kidney to assess for development of further nephrolithiasis.
Xanthogranulomatous pyelonephritis is a rare but significant urological disease with significant risk for complications and morbidity and may be preventable with early detection of patients at risk for complicated pyelonephritis. Elements of the pathological process, risk factors such as genetics and smoking have not been fully elucidated in the literature. Thought XGP is highly associated with renal stones, found in 85-100% of the cases. 2/3 of which are staghorn calculi. Female gender 83-91%, obesity, and metabolic syndrome. XGP can present with vague symptoms of flank or abdominal pain and fatigue and is frequently associated with anemia seen in 63-85% and in up to 35% of the cases without pyuria.1,3-11 The disease entity frequently occurs in middle-aged woman but may occur in children where the CT findings are frequently mistaken for malignancy. CT is the diagnostic modality if considered and shows most frequently and enlarged kidney, sometimes with the Bear’s Paw Sign of dilated caliceal spaces, often with poor cortical perfusion6 and an associated renal stone. Differential includes renal carcinoma, non-XGP chronic pyelonephritis and renal tuberculosis. Untreated may lead to invasive spread, fistula formation, and systemic infection. Nephrectomy is the definitive treatment and the definitive diagnosis is made on histological examination.
Given the high morbidity, and the biologically plausible assumption that disease process and complications develop over a long period of time earlier diagnosis and treatment is preferable. However, as our care demonstrated, significant healthcare exposure occurred in this symptomatic patient prior to the diagnostic imaging study. Further investigations should be made in a patient presenting with recurrent pyelonephritis.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.