INTRODUCTION
Squamous metaplasia rarely occurs within colorectal polyps. The incidence rate has been reported to be 0.44% in a large study of 5778 colorectal adenomas by Bansal, et al.1 Although several theories have been proposed, the mechanism, etiology and significance of squamous metaplasia in colorectal adenomas remain to be unknown. Some authors suggested the possibility of squamous differentiation to be the precursor lesion for colorectal squamous cell carcinoma.2
To the best of our knowledge there have been about 31 reports of squamous metaplasia in colonic adenomas documented in the literature since 1979.2 We have encountered two additional cases of focal squamous metaplasia arising in a tubular adenoma of rectum and within and intramucosal adenocarcinoma of the sigmoid. To confirm the nature of these nests, immunohistochemistry was performed. In both cases the squamous nests were negative for synaptophysin and chromogranin by immunohistochemistry. Ki67 showed no staining in the area of metaplasia. Although it has been proposed that squamous metaplasia may serve as the precursor lesion in colorectal squamous neoplasms, the importance and significance of squamous metaplasia in colorectal polyps remain to be determined.3 No consent is required to our article publication.
CASE REPORTS
Case 1
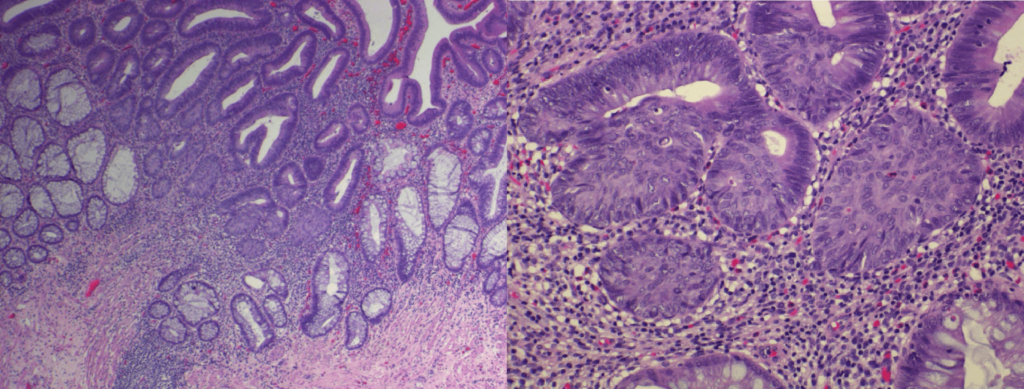
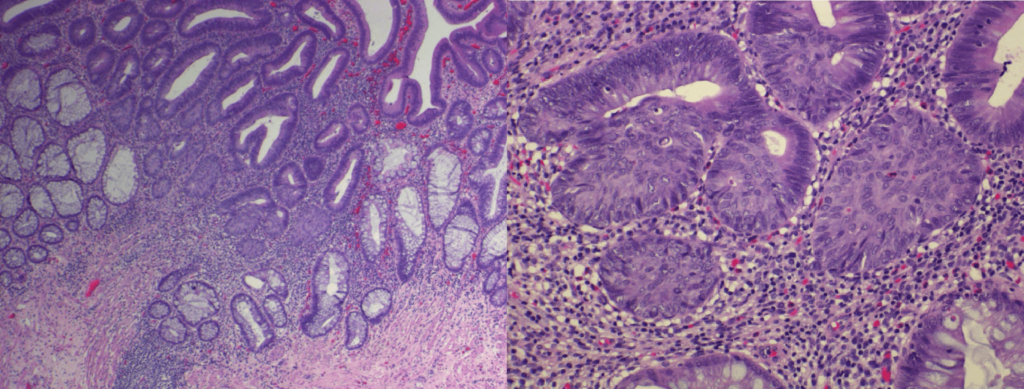
A 68-year-old male with history of multiple colonic polyps underwent follow-up colonoscopy and was found to have a rectal polyp. The polyp was sessile measuring 1.0×0.8×0.7 cm. Histologically, the polyp showed a tubular adenoma with focal benign squamous metaplasia (Figure 1).
Figure 1: Multiple foci of benign squamous metaplasia in a tubular adenoma (10× and 40× magnification, H & E stain)
Case 2
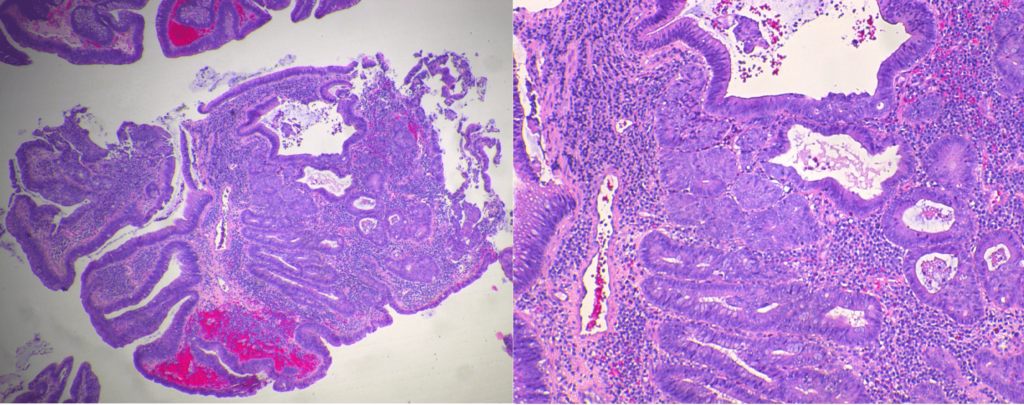
A 50-year-old male underwent his initial screening colonoscopy and was found to have two large polyps in sigmoid colon. The polyps were sessile measuring 1.0×1.0×0.8 cm and 2.8×2.3×2.1 cm. Histologically, the tumor showed intramucosal carcinoma arising from a tubulovillous adenoma with multiple foci of squamous metaplasia (Figure 2).
Figure 2: Multiple foci of squamous metaplasia in a tubulovillous adenoma with
focus of intramucosal carcinoma (10× and 40× magnification, H & E stain)
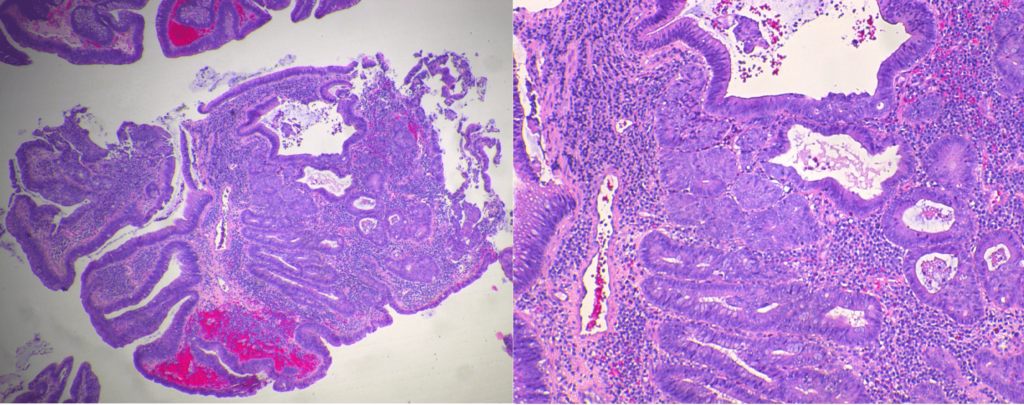
In both cases, the areas of squamous differentiation were discrete nests of immature squamous epithelial cells without identifiable keratin. Intercellular bridges were not identified. In our cases the squamous nests were located at the bases of the adenomatous crypts, but they also occurred in the middle of the proliferation.
DISCUSSION
Metaplasia is defined as a reversible adaptive change in which one differentiated cells type is replaced by another cell type that is better able to tolerate the adverse environment. Squamous metaplasia is the most common type of epithelial metaplasia. Epithelial metaplasia is a two edge sword and in most circumstances represents an undesirable change. In addition, the persistent predisposing influences to metaplasia may initiate malignant transformation in metaplastic epithelium.1 Squamous metaplasia has been rarely reported in neoplastic and non-neoplastic large bowel. The histogenesis and etiology of squamous metaplasia in colorectal adenomas is unclear, however chronic inflammation and mucosal irritation have been suggested as possible associations.4
William, et al. in their study suggested that squamous metaplasia may serve as the precursor lesion to squamous cell carcinoma.2 Primary squamous cell carcinomas of the colorectum are rare with a prevalence of approximately 0.1% among all colorectal carcinomas.5,6,7 The etiology and histogenesis are unknown. Several theories have been proposed with most authors favoring an origin from pluripotent stem cells capable of multidirectional differentiation.7 Some authors have also suggested the possibility of derivation from foci of squamous metaplasia associated with chronic mucosal irritation.6
Interestingly, cases of squamous metaplasia have also been reported in the rectum of patients with inflammatory bowel diseases in whom squamous cell carcinoma was also present in one.8 Although several theories have been proposed to explain squamous metaplasia in colorectal polyps, the importance and significance of squamous metaplasia in colorectal polyps remain to be determined.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interests.