INTRODUCTION
Spontaneous rupture of the urinary bladder (SRUB) is a rare and frequently misdiagnosed condition. The aetiology of SRUB is unknown. Unfortunately, SRUB diagnosis and treatment are frequently postponed or overlooked. In the literature, diagnosis is often only made during laparotomy. The recommended course of treatment for SRUB is surgical repair of the bladder.1,2 Our literature review demonstrated; however, that conservative treatment with indwelling catheterisation might also have positive outcomes in some patients. There are few case series of SRUB in the literature. We now acquaint you with a singular incident in a New Zealand hospital in Tauranga.
CASE REPORT
Our case report is a 63-year-old man who admits to alcohol dependence but without any significant prior medical history and not on any regular medications. He visited the emergency room at Tauranga Hospital with acute lower abdominal pain. The lower abdomen pain had started early in the morning and woke him from his sleep. He claims that there were no triggering factors and that the discomfort came on suddenly. He disputed any recent instrumentation or trauma.
Blood tests revealed the following results: Haemoglobin 154 g/L, White Cell Count 11.3×10E9/L, Neutrophils 10.1× 10E9/L, Lymphocytes 0.8×10E9/L, C-Reactive Protein 4.4 mg/L, Creatinine 219 μmol/L, eGFR 27 mL/min (Creatinine 94 μmol/L and eGFR 75 mL/min 3-months prior which are within the normal range) and Amylase 63 U/L with normal liver function tests. Additionally, his venous blood gas revealed a pH of 7.34 and lactate of 1.8 mmol/L.
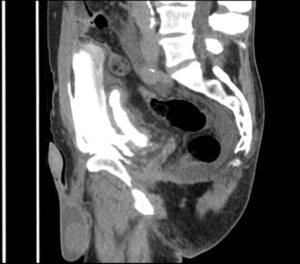
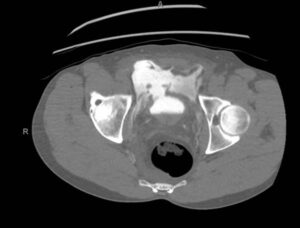
He was worked up for an acute abdomen and referred to the general surgery team, where they examined him for possible ischaemic bowel and performed a contrast CT-scan. The CT-scan revealed a collapsed bladder with surrounding peri vesical extravasation of contrast and retroperitoneal involvement, suggesting a bladder perforation. There were no other solid organ concerns and the prostate had an approximate volume of 37 cc.
Despite ongoing abdominal pain, he remained haemodynamically stable and was initially managed conservatively. An indwelling catheter was inserted (22 F 3-way with 20 mL in the balloon), which drained a significant amount of urine. He was then taken to theatre on June 21 2022, for a cystoscopy plus minilaparotomy. This revealed an anterior bladder wall defect (Figure 1). The edge of the ruptured bladder wall was debrided and sent for histology. The bladder was then closed in layers, and the catheter was left in situ. (Figures 2 and 3).
Figure 1. CT-Scan of the Abdomen on a Sagittal View Revealing Contrast Leak from Ruptured Bladder
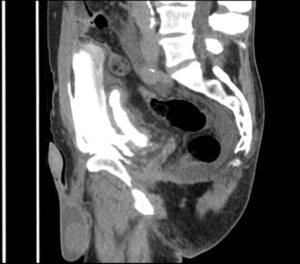
Figure 2. Coronal View of the Bladder with Contrast Extravasation
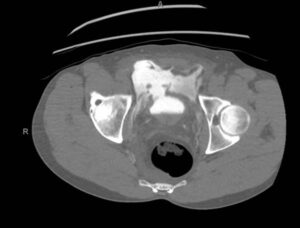
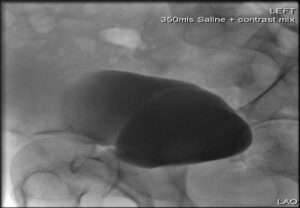
Figure 3. Post-Operative Cystogram in 6-weeks Showing No Contrast Extravasation
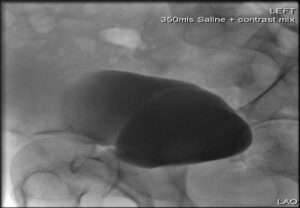
The patient remained as an inpatient for just a day. He had his surgical drain removed as there was minimal output. He had his wound inspected which was satisfactory and had education on wound management, catheter care and physiotherapy. Six-weeks later he was reviewed in the outpatient’s clinic where a post-outpatient cystogram was done, which showed no further leakage of urine and the catheter was safely removed. His final histopathology results of his bladder biopsy came back as “benign bladder mucosa with inflammation”. He was then discharged from the service with no further follow-up.
DISCUSSION
The incidence of spontaneous rupture of the bladder (SRUB), which is very rare, is approximately in every 126,000 individuals.1 Trauma is the most frequent reason for bladder rupture. About 60-65% of bladder rupture cases involve extraperitoneal rupture, while 25% involve intraperitoneal rupture.2,3,4 For a favourable outcome, a precise diagnosis and an appropriate intervention are essential. Only 713 cases from 319 literature pieces were reported in a prior study conducted in China in 2021, and many of the participants were middle-aged men.5
Since blunt force trauma is the primary cause of bladder ruptures, SRUB is regarded as a distinct diagnosis. A weak bladder wall is thought to be the primary cause of SRUB. Several risk factors, including recent endoscopic urological treatments, such as catheterisation, cystoscopy, or more invasive procedures such as TURBT or partial cystectomy, can be blamed for this. 5,6 A bladder diverticulum or a generalised bladder wall thinning in a post-menopausal woman are examples of pre-existing bladder characteristics that weaken the wall. Weakness of the bladder wall can also result from chronic urine retention brought on by benign prostatic hyperplasia (BPH), bladder or urethral calculi, urethral stricture, female bladder outlet obstruction, and female pelvic organ prolapse. Finally, elements that alter the anatomy, such as bladder tumours or stones, can cause inflammation, which causes necrosis and ulceration of the bladder wall.5,6
It is interesting to note that alcohol is cited as a contributing factor, and this patient did admit to consuming alcohol the night before. Heavy drinking has a diuretic impact that causes the bladder to swell to acutely, increasing bladder intraluminal pressure, and inevitably thins the bladder wall. Consuming alcohol will also cause paralysis of the central and peripheral nervous systems and bladder sensorium dysfunction, preventing the bladder’s normal micturition response. Lastly, some researchers postulate that frequent emesis in alcoholics raises intra-abdominal pressure, which can be then transmitted to the weakened bladder wall leading to rupture.7
Patients typically arrive in a variety of non-specific ways. From oliguria, without abdominal pain, to anuria, with severe abdominal pain and signs of excess fluid intra-abdominally. This is particularly seen in this case as he had significant output postcatheterisation. The two basic categories of ruptures are extraperitoneal and intra-peritoneal, and dysuria and abdominal pain are the two most typical symptoms of extra-peritoneal bladder rupture. In contrast, intra-peritoneal rupture is frequently accompanied by abdominal pain, macroscopic haematuria, difficulty urinating, or inability to urinate.8
There are no specific guidelines available on SRUB. However, most literature recommends that early diagnosis and treatment confer a better prognosis. Data shows that most cases were diagnosed intra-operatively as part of their management for acute peritonitis. However, just as in our case a CT cystogram can also be considered if the patient is stable and there is some index of suspicion.9
It is always advised to explore and repair intra-peritoneal bladder rupture surgically due to the significant danger of abdominal sepsis, which can be fatal if untreated. 10,11 On the other hand, extra-peritoneal ruptures that are thought to be minor can be treated without surgery, and this is the advice given in accordance with global standards. Ample urine drainage and antibiotic use are the cornerstones of conservative treatment.10,11
CONCLUSION
Urinary bladder spontaneous rupture is still an uncommon presentation. Patients frequently exhibit vague symptoms, making it easy to ignore them, thereby delaying diagnosis and therapy which could adversely impact outcomes. Bladder rupture should be considered as a differential in patients with an acute abdomen where there is a high index of suspicion due to the existence of potential risk factors. To evaluate whether a case may be treated non-operatively or surgically, preliminary imaging evaluation should be considered in every situation. To conclude, we do hypothesize that this patient had a delayed diagnosis of spontaneous bladder rupture which he feels strongly is related to his alcohol intake. With appropriate surgical intervention the patient made a full recovery.
CONSENT
The authors have received written informed consent from the patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.