INTRODUCTION
Lymphangioma is a rare benign tumor of the lymphatic system.1 microcystic Lymphangioma are the most common manifestations in the skin. These tumors are usually seen in childrenand exceptionally in adults. They occur most frequently in the neck (75%) and in the axillary region (20%).2 Scrotal localization remains rare. The diagnosis of scrotal lymphangioma is not always easy.
CASE REPORT
A 23-year-old boy with no medical history, in particular no history of trauma of the testicles, reported the appearance of vesicular lesions containing clear fluid in the scrotum evolving over 6-years, responsible for a dragging discomfort. On dermatological examination multiple confluent papules and erythematous nodules, of soft consistency, with non-infiltrated bases, and with a papillomatous aspect like a bunch of grapes were seen. These were adherent to the scrotal skin and independent of both the testicle and cord structures. There were no signs of inflammation (Figure 1).
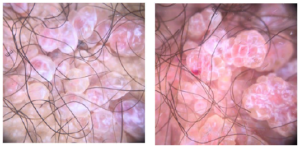
Trans-illumination was negative and the rest of the exam was normal. Dermoscopy showed vesicles grouped in clusters, sometimes clear, sometimes hemorrhagic, separated by white septae (Figure 2). Scrotal ultrasound, showed cystic formations around the scrotum with no abnormalities in the underlying scrotal tissue. There was a modest hydrocele on the right side. No abnormalities of the testicles and epididymis were noted.
A scrotal skin biopsy was performed, confirming the diagnosis of lymphangioma circumscriptum (LC).
Figure 1. Clinical Oppearance of Microcystic Scrotal Lymphangioma

Figure 2. Appearance of the Lagoons and Vesicles Filled with Yellow Liquid, Some are Filled with Blood,Wartty Appearance
DISCUSSION
Lymphangioma circumscriptum (synonym: microcystic lymphangioma) is a benign tumor that develops from the lymphatic system. It may be of congenital origin or acquired and is the most common type of cutaneous lymphangioma. A cervical or axillary localization is seen most frequently and is the most described. But it can be found on all regions of the body. However, a scrotal location is exceptional.1
Lymphangioma circumscriptum can appear on the skin and mucous membrane mainly spontaneously, but also after irradiation, local infections and surgery (e.g. vasectomy).2
The pathogenesis of LC was described by Fox et al3 as “lymphangiectodes” and then in 1889 by Morris, it received the name which is still used today “Lymphangioma circumscriptum”. In 1976 Whimster1 declared that LC results from the collection of lymphatic reservoirs which receive lymph from surrounding tissues but fail to flow into the normal lymphatic system because they are not connected to them; however, they are linked to the superficial lymphatic vessels.
Clinically, it is characterized by multiple translucent vesicles of different sizes, which contain clear lymphatic fluid (lymphorrhea), but they can become hemorrhagic. The vesicles can be grouped together and this sometimes gives a warty appearance to the lesion.4
Dermoscopy shows a lacunar/saccular pattern, due to the presence of lymphatic fluid varying from light brown to purple, resulting from the volume of blood enveloped by pale septae, which show a hypopyon-like, blood sedimentation.5 Another dermoscopic motif consists of colored areas varying from yellowish white to diffuse pink with linear vessels and dots. The presence of a hypopyon – like sediment is a sign recently reported.6
Ultrasound makes it possible to make the diagnosis and determine the extent of the lesions; magnetic resonance imaging (MRI) may also be used. LC usually remains asymptomatic, but can be complicated by secondary bacterial infections or flare-ups if traumatised.
Definitive treatment is necessary for the cosmetic appearances and to avoid the complications of LC. Different treatment methods are available such as radiofrequency ablation, sclerotherapy, ablative lasers and surgical excision of superficial and deep components to prevent recurrence of the lesion which is the most common post-operative complication ranging from 25 to 50% in the first 3-months.5
CONCLUSION
Scrotal LC (or microcystic lymphangioma) is a rare benign tumor. The clinical history is characteristic. The diagnosis, suspected by examination, can be confirmed by imaging and histology. Dermoscopy, which is a non-invasive technique, currently allows the diagnosis to be informed by several dermoscopic signs as described previously.
CONSENT
The authors have received written informed consent from the patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.