INTRODUCTION
Although renocolic fistula is a rare pathology, it is the most common of renoalimentary fistulas. This pathology continues to decrease in frequency in the last 50 years due to early and better management of renal diseases. A variety of etiologies of renocolic fistulas with their mechanisms have been reported. Tuberculosis (TB) used to be the most frequent etiology of all renocolic fistulas but this is no more as treatment medications for tuberculosis and the global campaign towards its eradication have been seriously implemented worldwide.
It is already known that tuberculosis can be an underlying cause for renocolic fistulas. However, the English literature has very few reported cases on this subject. We herein report a renocolic fistula in a 75-year-old Moroccan male diagnosed on a computed tomography (CT) scan. A biopsy of a suspected mass on the CT scan was performed during colonoscopy allowing a histopathological confirmation of TB being the underlying cause of this affection.
This presentation adds a recent case of renocolic fistula secondary to TB to the already existing literature whilst we discuss how to best diagnose and manage this affection.
CASE REPORT
A 75-year-old Moroccan man was admitted in our department for a 2 month history of left low back pain associated with an irritable bowel syndrome, fever and weight loss.
This patient had a medical history of hypertension and ischemic cardiomyopathy under diuretics, β-blockers and low dose aspirin. There was no preceding history of pulmonary tuberculosis.
Physical examinations found the patient in an altered general condition. His blood pressure and body temperature was 160/100 mmHg and 38.5 °C respectively. The patient had a left flank pain and tenderness.
Laboratory test of the patient were as follows: Hemoglobin=8 g/L, white blood cells=12000 /mcL with an 80% neutrophil pre-dominance, C-reactive protein=266 mg/L, Blood urea nitrogen=0.83 g/L, Creatinine=16 mg/L, Urine culture grew Escherichia coli (E.coli).
An abdominal ultrasound showed a left perinephric abscess.
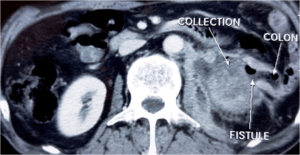
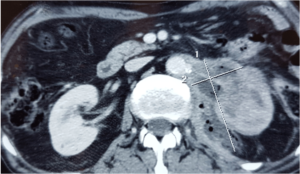
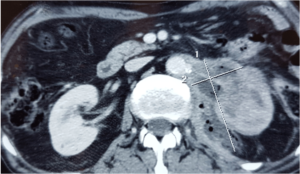
An abdominal CT scan with contrast objectified an enhanced heterogenous solid-cystic mass of the mid and lower portion of the left kidney containing gas bubbles, infiltrating the Psoas major muscle and in direct contact with the left colic flexure suggestive of a renocolic fistula (Figures 1 and 2).
Figure 1: Axial Abdominal Enhanced CT Scan Showing a Left Perinephric Abscess Associated with a Renocolic Fistula.
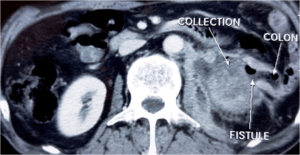
Figure 2: Axial Abdominal Enhanced CT Scan Showng Perinephric Abscess Extending to the Psoas Major Muscle Containing Gas Bubbles.
A colonoscopy was performed to search for lesions and to evaluate a suspected mass revealed on the CT scan. The colonoscopy revealed a totally obstructive and ulcerative mass located at 40 cm from the anus. This mass appeared as an extrinsic process that had invaded the colon. Biopsies of the mass were performed.
Histopathological examination of the biopsies revealed granulomas composed of multiple epitheliod cells and Langhans giant cells with central caseous necrosis. Diagnosis of TB was established.
An ultrasound guided percutaneous drainage of the perirenal abscess was performed and the patient was put under anti-TB treatment. The patient was programmed for surgery of the fistula but he passed away a week after his admission from septic shock and heart failure.
DISCUSSION
Renocolic fistulas often involve the ascending and descending segments of the colon. This pathology was first described by Hippocrates in 460 B.C.1 Though it is an ancient pathology, it remains rare with a few reported cases in the English literature.
There are various etiologies of renocolic fistulas but these can be categorized as traumatic or spontaneous.2 The colon is rarely the origin for renocolic fistulas3 Spontaneous renocolic fistulas are the most frequent and it’s largely caused by urinary tract tuberculosis and renal calculus.
Urinary tract TB was previously known to be the most frequent etiology4,5 but pyonephrosis secondary to renal calculus has been a predominant etiology in recent years. This can be explained by the availability of medications and efficient management of tuberculosis. Traumatic renocolic fistulas could be iatrogenic or in an event of a severe renal trauma. Iatrogenic causes of renocolic fistulas have reemerged in the last 20 years due to the increased minimal invasive kidney surgeries and percutaneous kidney drainages.6
There is no specific clinical sign to diagnose a renocolic fistula. Flank pain and fever are the most frequent symptoms. Pyuria, fecaluria, pnematuria and fever can be occasionally present.7 Hence, the diagnosis of a renocolic fistula and its underlying cause is largely dependent on radiological imaging. The most useful imaging modalities are CT urography, barium enema, colonoscopy and antegrade or retrograde pyelogram.8,9,10 Each imaging modality has its advantages and disadvantages. The CT scan is by far the best imaging modality to establish the diagnosis of renocolic fistula as in our case. Generally, a couple of these imaging modalities are required to determine the presence of a fistula and its underlying cause.
Surgery is the recommended treatment for renocolic fistula. The affected kidney is often not functioning. Thus, the surgery consists of nephrectomy associated with resection of the involved segment of the colon followed by anastomosis of the healthy colon segments.3,10,11,12 The underlying affection responsible for the fistula must be treated as well. TB was the cause of the renocolic fistula in our case. For this reason, the patient was put on anti-TB medication. The in 2003, Center for Disease Control (CDC) guidelines recommend a nine month regimen which includes Isoniazid, Rifampicin, and Ethambutol, supplemented with Pyrazinamid during the initial 2 months (Z2H9R9E9).13,14,15
CONCLUSION
Although renocolic fistula has been known since ancient times, it is a rare pathology especially in recent times. Tuberculosis was the frequent cause of spontaneous renocolic fistulas. However, there has been a significant decrease in frequency in the last 50 years.
Radiological imaging plays a critical role in the diagnosis of renocolic fistulas as there are no specific symptoms for this pathology. The CT scan is a better diagnostic tool to diagnose renocolic fistulas.
The management of renocolic fistula requires treating the fistula as well as its underlying cause. Hence, in the case of renocolic secondary to tuberculosis, it is recommended to perform surgery consisting of nephrectomy and colon resectionanastomosis. Anti-TB medication must also be administered.
DECLARATIONS
Ethics approval and consent to participate. Not applicable.
ACKNOWLEDGEMENTS
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
No additional file for data and supporting materials.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
TS prepared the manuscript and is the corresponding author OJP, BBS, SA contributed in the review of the articles MS, TMF, EAJE, KA, EFJM, FMH edited the manuscript. All authors read and approved the final manuscript.