INTRODUCTION
Subcoracoid impingement (SCI) is known to be caused by the narrow space between the coracoid and the lesser tuberosity which in turn causes impingement of the subscapularis and the biceps tendon with movements requiring forward flexion, internal rotation, and horizontal adduction.1,2,3 It has been recognized as an etiology of anterior shoulder pain for over a century. Many studies addressed the topic and have emphasized SCI to be relatively common, yet often unrecognized and underreported.4,5,6 An accurate diagnosis is critical for selecting an effective treatment among a wide range of options starting from conservative management to open and arthroscopic coracoplasty.7 Despite numerous studies on the topic, no standard imaging diagnostic criteria have yet been established.
Plain radiography, computed tomography (CT), and magnetic resonance imaging (MRI) have been used to evaluate coracohumeral distance (CHD).8,9,10,11 However, standard CT and MRI allow only static evaluation of the subcoracoid space and are not practical for bilateral evaluation. Diagnostic ultrasound is a well-established tool for the evaluation of rotator cuff condition and guiding therapeutic injections. We report the use of ultrasound (US) and MRI to measure CHD in patients with SCI with the hypothesis that patients with SCI will have narrower CHD.
MATERIALS AND METHODS
A total of 373 patients who were diagnosed with impingement syndrome clinically and radiographically at an outpatient clinic at a single institute between May 2014 and Feburary 2015 were identified. The inclusion criteria were the symptom duration of more than 3 months, no abnormalities on plain radiography, no rotator cuff tear on MRI, normal contralateral shoulder, and compliance and willingness to undergo all required sonography and tests. The exclusion criteria were stiffness or instability of the shoulder, previous surgery, and inflammatory condition of shoulder including infection or calcific tendinitis.
Finally, 150 patients in total were found to meet the inclusion criteria. All patients had visual analogue scale (VAS) score checked at initial presentation and underwent a physical examination, MRI, and bilateral sonography. Depending on their clinical findings, the subjects were divided into two groups: SCI with subacromial impingement (SAI) group (SCI group) and SAI only group (SAI group).
SCI group had clinical features of SAI and clinical findings suggesting the diagnosis of SCI, which consisted of the typical history of anterior shoulder pain, tenderness at the coracoid process, and a positive coracoid impingement sign, and positive coracoid impingement test. Coracoid impingement sign was considered positive when a patient reported anterior shoulder pain when the arm was in forward elevation, internal rotation, and adduction.12 The coracoid impingement test was performed by a diagnostic injection of lidocaine 2 mL (2%) and triamcinolone 1 mL (40 mg/ml) in to the subcoracoid recess with ultrasound guidance. The test was considered positive if the pain was reduced by more than 30% at VAS and the physical examination was negative after two weeks.
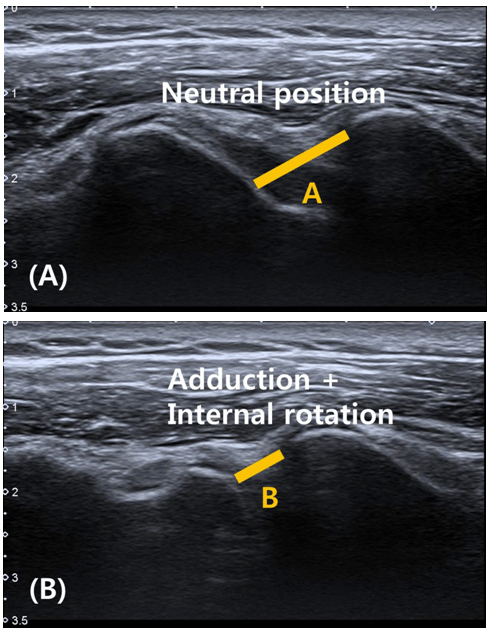
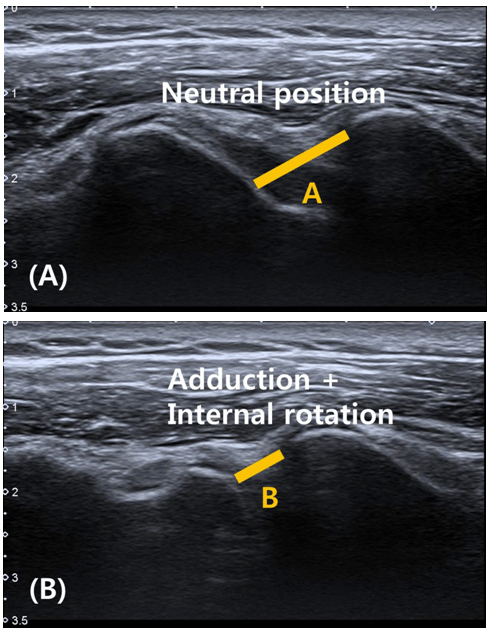
CHD was measured on MRI (1.5-T cylinder shaped, Inter Achieva; Philips, The Netherlands), which was taken with the subject’s arm in neutral position. CHD was defined by the greatest subcoracoid narrowing from coracoid cortical margin to the humeral cortical margin as suggested by Giaoli et al8 (Figure 1). CHD was also measured on screen during the bilateral shoulder sonography with the arm adducted and in a neutral position. CHD was measured coronally using a multifrequency linear array ultrasound transducer with a peak frequency of 13 MHz (Toshiba Medical Systems, Tochigi, Japan) twice the symptomatic shoulder and once on the asymptomatic shoulder in each subject. The same sequence of measurements was taken with the arm adducted and internally rotated to a point when the cortical margin of the lesser tuberosity was closest to the coracoid tip (Figure 1). After the measurements with sonography, the relative ratio of distance difference (RRDD), defined as the percentage of the distance difference in the neutral position and internal rotation compared with the distance in the neutral position, was also calculated. This method was used to standardize the relative distance difference in internal rotation to the individually different CHD (Figure 2).
Figure 1: Coracohumeral Distance (CHD) which was defined as the Greatest Subcoracoid Narrowing from Coracoid Cortical Margin to the Humeral Cortical Margin was measured on MRI Axial View

Figure 2: (A) CHD was measured Coronally with the Arm Adducted and in Neutral Position from the Cortical Margin of the Lesser Tuberosity to the Cortical Margin of the Coracoid Tip. B) The Same Measurements was taken with the Arm Adducted and Internally Rotated to a Point when the Lesser Tuberosity was Closest to the Coracoid tip. Relative Ratio of Distance Difference (RRDD) is defined as the Percentage of the Distance Difference in Neutral and in Internal Rotation Compared with Distance in Neutral. (RRDD=(A-B)/A 100).
SPSS software (version 18.0 for Windows; SPSS Chicago, IL, USA) was used for statistical analyses. Student’s t-test was used to compare the CHD between SCI and SAI groups and other variables. The nonparametric data were evaluated with χ2 test. The significance was defined as p<0.05.
RESULTS
In total 39 (26%) subjects showed all the clinical features of SCI, including positive coracoid impingement test (SCI group) and 111 (74%) had only SAI symptoms (SAI group). There was no significant difference among the side of involvement, mean age, sex distribution, VAS score at initial presentation, and the duration of symptoms (Table 1). The intraclass correlation coefficients for the intraobserver reliability of sonographic CHD measurements in the neutral position and internal rotation were in the excellent rage with 0.84 and 0.82, respectively. In all subjects, there was no significant difference in the mean CHD between the involved and uninvolved shoulder in neutral (p=0.58) or internal rotation (p=0.50). No significant difference in the mean CHD in neutral position was seen between the measurements on MRI and ultrasound (p=0.87) (Table 2).
| Table 1: Demographic Data and Comparison of Clinical Presentation between SCI and SAI Group. |
|
SCI group |
SAI group |
p-value |
| Number (total 124) |
39 (26%) |
111 (74%) |
– |
| Affected side |
|
|
0.52 |
| Dominant |
28 |
75 |
|
| Non-dominant |
11 |
36 |
|
| Age (years) |
|
|
0.99 |
| Range |
32-70 |
26-71 |
|
| Mean |
54.1 |
51.9 |
|
| Sex distribution |
|
|
0.40 |
| Male |
20 |
60 |
|
| Female |
19 |
51 |
|
| Symptom duration (months)* |
8.1± 6.0 |
7.7 ± 6.5 |
0.42 |
| VAS (at rest)* |
1.7 ± 1.8 |
1.6 ± 1.1 |
0.57 |
| VAS (at ROM)* |
6.0 ± 1.0 |
6.3 ± 0.9 |
0.82 |
| *Mean±SD |
| Table 2: Comparison of CHD in Neutral Position between MRI and Ultrasonogrphy (US). |
|
MRI. |
US |
p-value |
95% confidence interval |
| CHD* |
0.93±0.19 |
0.94±0.21 |
0.87 |
-0.15, 0.17 |
| *Mean±SD |
The difference in the mean CHD in internal rotation between the SCI (0.48±0.15) and SAI groups (0.51±0.22) on ultrasound did not show significant difference (p=0.11). There was no significant difference between the two groups regarding the measurement difference in neutral position and internal rotation (p=0.90). However, the RRDD, which was used to standardize the amount of CHD difference in neutral position and internal rotation to the different CHD’s among individuals, was 50.3%±9.3% in SCI group and 35.7%±9.9% in SAI group and differed significantly (p=0.01) (Table 3).
| Table 3: Comparison of CHD between SCI and SAI Group. |
|
SCI group
(n=28)
|
SAI group
(n=96) |
p-value |
| CHD on MRI (cm) |
0.91±0.16 |
0.92±0.19 |
0.85 |
| CHD on ultrasonography |
|
|
|
| Neutral |
0.92±0.25 |
0.94±0.37 |
0.49 |
| Internal rotation (IR) |
0.48±0.15 |
0.51±0.22 |
0.11 |
| Neutral-IR difference |
0.44±0.21 |
0.43±0.29 |
0.90 |
| RRDD (%)* |
50.31±9.30 |
35.72±9.91 |
0.01† |
Mean±SD
*Relative ratio of distance difference
†p<0.05 |
DISCUSSION
This study hypothesized that patients with SCI will have narrower CHD. We used dynamic ultrasonography, measuring CHD in two positions, and showed that although there was a significant difference in RRDD between the two groups, the absolute CHD in the neutral position or in the internal rotation did not differ significantly between the two groups. This implies that the individualized difference in coracohumeral interval during the internal rotation, which is one of the key motions to elicit SCI, may be associated with the symptoms. The relation between the coracoid and the humerus has been studied extensively over the past two decades.
Most authors agree that the diagnosis of SCI is mainly clinical. Gerber et al2 described SCI as a dull anterior shoulder pain aggravated by forward flexion and internal rotation. A physical examination of affected patients shows tenderness at the coracoid tip and reproduction of pain with the arm internally rotated at 90° abduction or adducted with 90° of shoulder flexion. Many studies have reported subcoracoid stenosis to be relatively common, but often unrecognized and underreported.4,5 Isolated SCI is very uncommon and its incidence has been reported to be 2.8-19%.3,13,14 In order to overcome the low number of subjects, we enrolled patients with SAI without rotator cuff tear or stiffness and divided them into two groups depending on whether they had SCI. In our study, the incidence of SCI was found to be 26% in the patients with SAI.
Many studies have reported promising results for the treatment of SCI with the advent of arthroscopic coracoplasty7,15; however, determining proper candidates for such surgery has become crucial. Although, there are many studies investigating the relation between the coracoid and the humerus, the role of imaging in the diagnosis of SCI is still controversial. Standard radiographs may show far laterally projecting coracoid process in the anteroposterior view or in the supraspinatus outlet view. Kragh et al16 identified a chevron-shaped coracoacromial outlet in the patients with primary SCI. There may also be sex-based differences in the average coracohumeral interval, with females having a space measuring 3 mm or smaller than that in males.8 Bonutti et al17 described abnormal CHD to be less than 11 mm on MRIs in the patient with shoulder pain. Richards et al18 reported narrowed CHD in patients having tears of the subscapularis. They found an average CHD of 10 mm in the patients without rotator cuff pathology and a decreased distance of 5 mm in the patients with subscapularis tears. MRI examination was found to be 5.3% sensitive but 97% specific for SCI.8
Several studies have shown that coracohumeral interval decreases with shoulder position. Gerber et al10 used CT to evaluate coracohumeral interval in healthy patients. They found that the average value of 8.7 mm decreases to 6.8 mm with forward flexion. Friedman et al11 used dynamic MRI to evaluate coracohumeral interval, and asymptomatic volunteers showed coracohumeral interval of 11 mm in maximum internal rotation, whereas symptomatic patients showed 5.5 mm. However, these techniques are not widely available and cumbersome and also are not a cost-effective diagnostic option.
Ultrasonography is an easily available, dependable method to evaluate the relation between the coracoid and humerus and diagnose SCI. In addition, the dynamic real-time evaluation of the subcoracoid recess thereby overcoming static evaluation obtained by CT or MRI as well as concomitant usage of the treatment by delivering injections to the affected sites makes sonography more beneficial.
Ultrasonography for the diagnosis of SCI has been reported only in one study in the literature, showing a narrowed CHD in patients with clinically diagnosed SCI (n=8).19 However, the sonographic measurements were done statically in a single position on a small number of patients without comparison with MRI.
To the best of our knowledge, no study has examined so far SCI dynamically with ultrasonography. We ruled out other possible shoulder pathologies with MRI and also compared CHD in the neutral position.
However, this study had several limitations. The SCI and SAI groups were not matched for age, sex, or BMI. We have not taken into account of the soft tissue thickening on the anteroinferior aspect of the coracoid tip representing the fibrous falx as demonstrated by Dumontier et al,3 which can be a potential source of impingement. We grouped patients according to their findings during clinical examination. However, the clinical examination is subjective by nature, and the validity of subcoracoid physical tests has not yet been reported. Although, the effectiveness of the steroid mixed with local anesthetic injection confirmed the accuracy of our clinical diagnosis of SCI, but it may as well alleviate the symptoms related to other shoulder pathologies and confuse the diagnosis. Future studies are warranted to prove the reliability and validity of our procedure.
CONCLUSION
Although, the SCI group and the SAI group were not matched for age, sex, or BMI, no significant difference in CHD was seen between the SCI and SAI groups. RRDD value was greater in SCI group suggesting that individualized CHD in flexion and the internal rotation should be taken into account when assessing patients with SCI.
ACKNOWLEDGEMENTS
The research was performed at Inje University Seoul Paik Hospital, Seoul, South Korea.
CONFLICTS OF INTEREST
All authors declare no conflicts of interest.
FUNDING
Supported by outside funding or grant(s) from: None.