Background
Acute pancreatitis (AP) is a disorder clinically characterized by upper abdominal pain and elevated levels of pancreatic enzymes in the blood.1 After an initial evaluation, up to 10-30% of patients with AP are diagnosed with idiopathic acute pancreatitis.2 Clinical history and conventional diagnostic tests such as blood chemistry, ultrasound (US), computed tomography (CT) scan, magnetic resonance cholangio-pancreatography (MRCP) and endoscopic ultrasonography (EUS) usually discover most causes of the recurrent acute pancreatitis (RAP). Occasionally, the first presentation, in adult patients, with pancreatic cancer (PC) is with RAP.3 We should bear this in mind.
Case Report
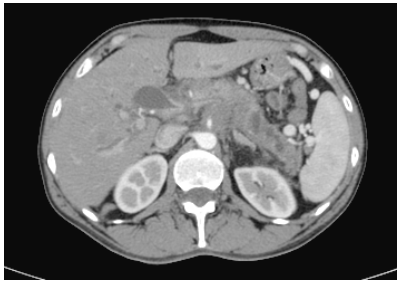
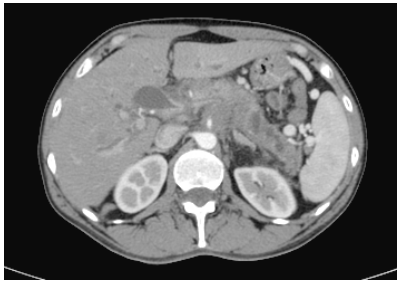
A 48-year-old woman with a smoking habit of 20 cigarettes per day until 2 years ago was admitted to hospital in August 2015. She presented with nausea and epigastric pain radiated to the back. Laboratory analysis showed the following serum results: amylase 3.139 IU, lipase 1.296IU, CRP 144 mg/L. An abdominal US, CT, and MRCP showed oedema of the pancreatic tail (Figure 1). Neither gallbladder stones nor other biliopancreatic alterations were found. The patient was diagnosed with AP and discharged 6 days later. In September, she suffered 2 new episodes of mild acute pancreatitis and a laparoscopic cholecystectomy was performed, in order to avoid later attacks of pancreatitis. At that time, a new CT, abdominal magnetic resonance imaging (MRI) and MRCP didn´t show any changes. In December, a new episode of pancreatitis arose. EUS was performed then but no biliopancreatic pathology was evidenced and, it was decided to do an endoscopic retrograde cholangio-pancreatography (ERCP) with biliary sphincterotomy. After ERCP, on laboratory analysis, the transaminases, amylase, and lipase remained elevated, and there was no clinical improvement. No other analytical alterations like calcium, triglycerides, antinuclear antibodies and serum IgG4 levels were found. It was then decided to treat with oral prednisone with a possible diagnosis of autoimmune pancreatitis with normal IgG4 in mind. Over the following 6 months there was a clinical improvement but after the 7th month, she presented again with lower back pain. At that time, 11 months after the first episode of pancreatitis, a CT showed a non-enhancing mass of 4.5 cm in the body of the pancreas that encompassed the celiac trunk and the superior mesenteric artery with dilatation of the distal main pancreatic duct (Figure 2). A fine-needle aspiration biopsy (FNAB) confirmed an adenocarcinoma and chemotherapy was initiated.
Figure 1. Abdominal Computed Tomography (CT) Scanning with Contrast: Slight Increase in Peri-pancreatic Fat Density in the Pancreatic Tail, Suggestive of Acute Pancreatitis

Figure 2. Abdominal Computed Tomography (CT) Scanning with Contrast 11 Months Later of the First Episode of AP: A Unenhanced Mass of 4.5 cm in the Pancreatic Head-Body Infiltrating the Celiac Trunk and the Superior Mesenteric Artery. Distal Dilatation of the Main Pancreatic Duct is Seen
Discussion
Causes of RAP´s can be classified into mechanical, inherited, metabolic, toxic, drug-induced and miscellaneous.3 Pancreatic cancer (PC) is a rare etiology of AP. The prevalence of PC in individuals presenting with acute pancreatitis range from 0.9 to 3.6 %.4 Few publications have reported some cases of RAP due to pancreatic cancer.4,5,6,7,8,9,10,11 They have tried to clarify the characteristics of this entity to facilitate its early diagnosis (Table 1). Generally, RAP bouts are mild to moderate, requiring a few days of hospitalization. The most common findings on US and CT scan are self-limited oedematous changes within the pancreas.12
| Table 1. Recurrent Acute Pancreatitis (RAP) due to Pancreatic Cancers: Findings in the Main Published Studies |
|
Author
(year)
|
Cases
(n) |
Mean age
(years) |
AP
Severity |
High
CA 19.9 level
(% patients) |
Location |
Months to diagnosis
(Mean) |
| Lin5 |
2 |
52 y |
Mild: 100% |
NA |
Head: 50%
Body-tail: 50% |
5 m
|
|
Mujica6
|
45 |
58 y |
Mild: 89% |
62% |
NA |
8.5 m |
| Minato4 |
18 |
63.7 y |
Mild: 94% |
80% |
Head: 67% |
7 m
|
|
Kimura11
|
7 |
62 y |
NA |
50% |
Head: 57% |
8.5 m
|
| NA: Not available |
We reported a case of pancreatic cancer that presented with recurrent episodes of acute pancreatitis. Occasionally, in adult patients, AP can be the first manifestation of pancreatic cancer. The average time established between the first episode of AP and the detection of PC is around 12 months.13 In our case, it was 11 months. Therefore, after successive episodes of acute pancreatitis with unexplained etiology, it is considered essential to follow-up these patients with EUS and TC for a long period of time for at least 12 months. This recommendation is of utmost importance in patients over the age of 40.
Pancreatic cancer can cause AP by an obstructive mechanism of the main pancreatic duct.12,14 Surprisingly, for several months significant changes in the main pancreatic duct and the pancreatic parenchyma were not observed. In the past, it has been difficult to classify the etiology of this relapsing disease. Unexplained pancreatitis represents a diagnostic challenge, although after different investigations a cause is found in the majority of these patients. However, we must not forget the possibility of pancreatic cancer in adult patients.
CONFLICTS OF INTEREST
All the authors declare no conflicts of interest.