INTRODUCTION
With the lack of current screening tests for cholangiocarcinoma recommended for routine use and the often-insidious onset of the disease, it is imperative to recognize the symptomatology of the disease and initiate treatment early, as it will impact the quality of life (QoL) and goals of care of the individual involved. During the last 30-years, it appears that the incidence of biliary tract cancers in the United States is increasing.1 This increase may be due in part to increased recognition of the diagnosis of biliary cancer, cases which may previously have been classified as cancer of unknown origin. Gallbladder cancer is more common in women than in men and in some countries, the rates are three times higher for women.2 Its clinical presentation is often variable and the majority of patients develop symptoms at advantage stages. It may present with biliary obstruction and associated symptoms of jaundice, pruritus, clay-colored stools, dark urine or abdominal pain (30-50%), weight loss (30-50%), and fever (up to 20%).3 Some patients are asymptomatic, with the lesions detected incidentally when imaging is obtained as part of the workup of abnormal liver blood tests.4 Due to its lack of specific diagnostic criteria and variability in symptoms, it frequently presents at a late stage.
In this case, 2-years preceding discussed hospital admission, the 67-year-old female patient underwent a routine laparoscopic cholecystectomy. Based on the operative note, there did not seem to be any suspicion of cancer at that time, so the diagnosis of cancer was unexpected. The pathology report revealed poorly differentiated adenocarcinoma and further imaging noted diffuse findings of adenopathy with biopsy confirming metastatic poorly differentiated carcinoma. With her known history of cholangiocarcinoma, she presented acutely to the emergency room with clinical features of optic nerve compression; with left lateral rectus palsy and features of panhypopituitarism. This is significant because the etiology of her symptoms was suspected to be due to pituitary metastasis -which in this group of malignancies is rare.
CASE PRESENTATION
A 67-year-old female with a past medical history of hypertension, hyperlipidemia, type II diabetes (T2D), iron deficiency anemia, osteoarthritis and cholangiocarcinoma after cholecystectomy with bone metastasis presented to the emergency department directly from outpatient oncology office due to hypotension (66/44) measured upon arrival to the office. She had initially presented to the office for routine follow-up of positron emission tomographycomputed tomography (PET-CT) scans. In the emergency department (EM), the patient reported worsening diplopia and fatigue. Physical exam revealed the patient was unable to deviate her left eye outward. After initial resuscitation with crystalloids, the patient was stabilized and further investigation was initiated. Labs indicated anemia (hemoglobin: 8.7 g/dL), thrombocytopenia (92×103/uL), hyponatremia (133) and hyperkalemia.5,6
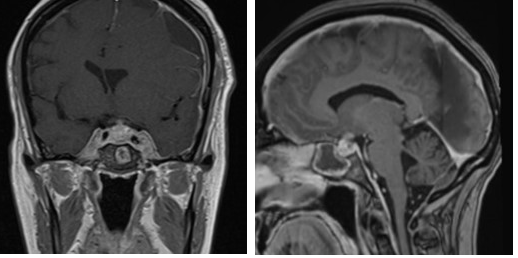
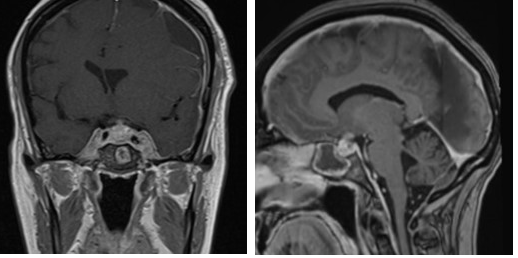
Magnetic resonance imaging (MRI) of the brain noted an abnormally enlarged pituitary gland, with enhancement suspicious for a malignant lesion, measuring 13.3×12.9×12.5 mm. Based on the above findings, endocrinological workup was pursued. Thyroid Stimulating Hormone (TSH), T4, adrenocorticotropic hormone (ACTH), serum AM cortisol, prolactin, insulin-like growth factor 1 (IGF-1), follicle-stimulating hormone (FSH) were ordered. ADH was assessed by urine output and was found to be normal. TSH (0.035 UIμ/mL), T4 (0.29 ng/dL), ACTH (<5.0 pg/mL), AM cortisol (2.9 μg/dL) and prolactin (10.3 ng/mL), FSH (2.9 mlU/mL) were low suggestive of panhypopituitarism. IGF-1 (33 ng/mL) was found to be low with correlating osteopenia but due to active malignancy, was not treated, as it was suspected it would precipitate increased growth of malignant cells as well. The patient was placed on IV hydrocortisone for secondary adrenal insufficiency and IV levothyroxine for central hypothyroidism. The patient’s blood pressure and fatigue improved with the treatment of her secondary adrenal insufficiency and central hypothyroidism.<5.0 pg/mL), AM cortisol (2.9 μg/dL) and prolactin (10.3 ng/mL), FSH (2.9 mlU/mL) were low suggestive of panhypopituitarism. IGF-1 (33 ng/mL) was found to be low with correlating osteopenia but due to active malignancy, was not treated, as it was suspected it would precipitate increased growth of malignant cells as well. The patient was placed on IV hydrocortisone for secondary adrenal insufficiency and IV levothyroxine for central hypothyroidism. The patient’s blood pressure and fatigue improved with the treatment of her secondary adrenal insufficiency and central hypothyroidism.
Another finding on the MRI brain was a new left subdural hematoma over the cerebral hemisphere, which eventually progressed with features of increased intracranial pressure and the patient underwent burr hole drainage, decreasing the hematoma size and midline shift. She was placed on prophylactic anti-epileptic drugs. She was transferred to a tertiary care center for further management and a possible biopsy of the pituitary. The patient ultimately refused further surgical intervention or radiation, including obtaining a biopsy for confirmation of metastatic intracranial mass. As she was awaiting placement, she became hypotensive and hypoxic. The patient lost a pulse and coded twice. The patient was resuscitated, however despite pressor support, the patient was experiencing multi-organ dysfunction. Ultimately, the patient was placed on comfort measures and shortly passed (Figure 1).
Figure 1. MRI Imaging Revealed Abnormal Pituitary Gland and Subdural Hematoma
DISCUSSION
The tumor commonly metastasizes via lymphatic spread to the regional lymph nodes, followed by hematogenous metastasis to the liver, lungs, and peritoneum.6 Distant metastasis is uncommon, and the incidence of brain metastasis was 0.15%, 0.47% and 1.4% in three large case series of cholangiocarcinoma and there have been only eight reported cases in the literature of neuro-ophthalmologic and ocular presentations of cholangiocarcinoma.7 The 5-year survival rate, once cholangiocarcinoma spreads to a distant part of the body is 2%.8 Recognizing physical exam findings such as diplopia and correlating them to hypotension and laboratory findings of hyponatremia, hyperkalemia, and hypothyroidism can direct to the differential diagnosis of panhypopituitarism. Treating panhypopituitarism with co-existing central hypothyroidism can be challenging as the timing of treatment of hypothyroidism is important. Treatment of hypothyroidism with thyroxine can precipitate adrenal crisis in patients who also have adrenal insufficiency, therefore it is recommended to administer the first dose of levothyroxine at least one hour after the initial bolus of hydrocortisone to reduce the risk of thyroid-induced adrenal crisis. Despite these efforts, as the incidence of brain metastasis is so low, it is difficult to predict patient outcomes due to insufficient data. There may be a growing acceptance that tumors should be treated differently according to their location and had the patient decided on biopsy; with the coordination of a multidisciplinary team of radiation and medical oncology, an alternative treatment plan may be discussed. However, as advanced malignancy progresses, discussing and readdressing goals of care during hospital admission transition points is an important task to better facilitate end-of-life care (EoLC).
CONCLUSION
This case emphasizes the clinical diagnosis of adrenal insufficiency and its refractory panhypopituitarism. In spite of being managed appropriately, the patient did not improve and eventually passed away. Goals of care include hemodynamic stability, with aggressive rehydration, repleting critical hormones and close intensive monitoring. Although pituitary metastasis is uncommon in primary cholangiocarcinoma; given physical exam findings of left lateral rectus palsy, metastasis should be considered.
CONSENT
The authors have received written informed consent from the patient.
CONFLICT OF INTEREST
No potential conflict of interest related to this article was reported.