INTRODUCTION
Prostate cancer (CaPR) is the most common genitourinary cancer in men and the second leading cause of cancer death after lung cancer.1 Cutaneous metastases (MTSc) of internal cancers are rare, ranging from 0.6% to 10%.2,3 The most frequent sites of metastasis (MTS) are bones and lymphatics, being rare in the liver and lung.4 A literature review reveals 35 English case reports of MTSc from CaPR.5,6 We present a CaPRMTSc case.
CASE REPORT
A 60-year-old man, with medical history of diabetes, ex-smoker was presented and diagnosed with prostate cancer (Gleason Score 5+5) in 2016, with baseline prostate-specific antigen (PSA) 14 ng/ml. Complete androgen blockade was performed with luteinizing-releasing hormone (LHRH) analog and antiandrogen and prostate radiotherapy due to localized oncological pathology through staging studies. At 9-months, he presented a biochemical relapse, the restaging computerized tomography (CT) scan showed multiple intercavo aortic and bilateral iliacs lymphadenopathies, and a hypodense image in the sacral bone, which may correspond to secondary disease. The bone scintigraphy showed hyperuptake in the sacral bone. Chemotherapy (CTX) was performed with Docetaxel (18 sessions) with good biochemical and clinical response, with decrease in lymph node images and decrease in the size of the sacral lesion in the first 3-months. Eight-months after the start of CTX, bone progression was evidenced in the ribs, sternum and cranial calotte, as well as liver and lung metastases with a rise in PSA to 20 ng/ml. It was decided to start enzalutamide therapy continuing with androgen blockade.
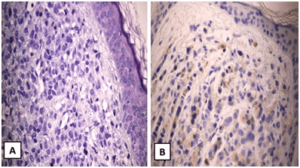
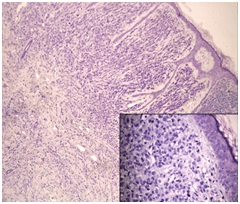
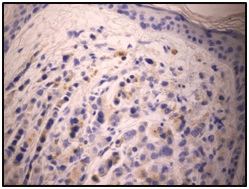
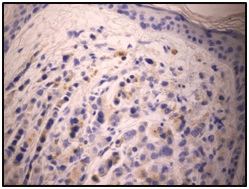
Four-months later, the patient was consulted for 2-month evolution nodular, violaceous, raised, non-pruritic formations, on an erythematous base in the right inguinal region and suprapubis (Figure 1). Lesions were evaluated by dermatology department and punch biopsy was decided. Histopathological results revealed epidermis with atrophy, dermis with infiltration by medium-sized cells, with a high nucleo-cytoplasmic ratio, anisocariosis and few cytoplasms with imprecise limits. Immunohistochemistry was performed and showed positive staining for PSA, concluding in lesions compatible with metastasis of acinar carcinoma of the prostate (Figures 2, 3 and 4).
Figure 1. Nodular Formations on an Erythematous Base in the Right Inguinal Region and Suprapubic

Figure 2. (A) Hematoxylin and Eosin (H&E) Examination of Skin Punch Biopsy 400x.
(B) Prostate Specific Immunohistochemical Staining at 400x(visualization: cytoplasmic)
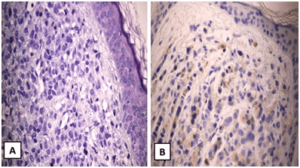
Figure 3. Hematoxylin and Eosin (H&E) Examination of the Skin Punch Biopsy 100x. Inset Image Shows the Same Sample at 400x
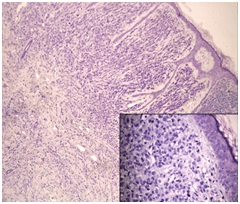
Figure 4. Prostate Specific Immunohistochemical Staining of the Same Skin Sample at 400x (visualization: cytoplasmic)
Chemotherapy was started, receiving 2 cycles of cabacitaxel without evidence of clinical response. The patient died 4-months after detection of the MTSc.
DISCUSSION AND CONCLUSION
CaPRMTSc is an infrequent entity and less than 100 cases were reported in the literature until 2016. An incidence of 0.09% of MTS in CAPR skin is recorded, which can increase taking into account the refractoriness and final stage of pathology.7,8,9,10
In recent years, case reports of skin involvement has increased. This could be due to both the relative increase in the elderly, the world’s population and the development of new treatments for CaPR that extend the survival rate.8
CaPR can metastasize through four different mechanisms: local spread of the disease, implantation through a surgical scar, lymphatic spread, and hematogenous spread.9
Cutaneous involvement has a poor prognosis as in other malignancies. It is considered an advanced disease marker with an average survival of 6-months.4,8,11,12 Therefore, a skin extension should be suspected when appearing new skin lesions in a patient with an aggressive oncological diagnosis.
When skin involvement appears, they are usually nodular lesions that involve the supra pubic region, anterior aspect of the thigh, inguinal region, and few reports of facial, neck, chest and umbilical region involvement.8,10,13,14
In the literature review, Pistone et al15 shows a patient with a history of prostate cancer who develops two tumors in chest and neck, after eight years of the diagnosis of the neoplasm, which were compatible with skin metastases. On the other hand, Rodriguez-Lojo et al14 presents two cases of cutaneous metastases of the prostate, of which only one of them appeared in the skin of the chest as subcutaneous infiltration after eleven-years. In both cases, the presentation time of the metastasis was different from ours, which was 2-years possibly due to the tumor undifferentiation, however, according to our case, the patients died within a few months of the diagnosis of skin metastasis.
Unlike our report, Champoñan-Relaiza et al16 presented a case of skin lesions in the chest and neck without a previous diagnosis of prostate cancer. When performing a skin biopsy, positive cell staining was shown for specific prostate antigen.
In our case, it is an aggressive, undifferentiated CaPR, which was evidenced by the Gleason Score (5+5), with early refractoriness to the established treatments.
Prostate specific antigen and prostate specific acid phosphatase (PSAP) are sensitive and specific immunoreactives for CaPR, however in certain cases they can be negative due to the great undifferentiation that the tumor could present.9,13,17 Thus, immunohistochemistry become essential for diagnosis in these cases.
To conclude, urologists and dermatologists should bear consider a differential diagnosis when examining nodular lesions or skin rash in oncological patients, knowing that it may represent as the first manifestation of an oncological disease and are largely associated to a bleak forecast.
CONSENT
The authors have received written informed consent from the
patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.