INTRODUCTION
Child abuse is a major global social concern. The number of child abuse cases handled by child consultation centers in Japan in 2015 was 103,260, a number that has been increasing each year. It has been reported that newborn babies account for 60% of all children who die as a result of abuse in Japan.1 Ninety percent of mothers who committed abuse reported that they had an unplanned pregnancy, and 80% reported that they did not receive the Maternal and Child Health Handbook. The Maternal and Child Health Handbook consists of records of pregnancy, delivery, child development and immunization, as well as child growth charts. Studies have found that acceptance of the pregnancy influences child abuse. Relevant organizations must, therefore, respond immediately to cases of child abuse. “Sukoyaka Oyako 21, second plan” is a national Japanese plan to improve the health of mothers and children that began in 2015.2 It suggests that preventing child abuse should begin during pregnancy.
In addition, it is clear that postpartum depression and anxiety are causes of child abuse.3,4,5 Pregnancy or childbirth can trigger depression in some women. According to the research of Cadzow et al, on antepartum and postpartum mental health, weak attachment bonding between the fetus and mother during pregnancy was associated with postpartum depression and anxiety.6 Furthermore, Sugishita et al found that postpartum depression decreased when attachment to the fetus was higher during the antepartum period.7 The application of theoretical knowledge of bonding during pregnancy suggests the possibility of decreasing postpartum depression.
This study aimed to verify the hypothesis that postpartum depression decreases when bonding is promoted during pregnancy.
MATERIALS AND METHODS
Study Design
This was an interventional quasi experimental study. It investigated depression and fetal/neonatal and maternal bonding during both the antepartum and postpartum periods.
Study Setting
The study was conducted at a general hospital located in Nagoya, Japan. The participants were divided into either a control (odd months) or intervention group (even months) based on the expected date of childbirth. Mothers in the intervention group started an intervention program that included listening to “fetal music” and writing a “fetal diary”, while mothers in the control group did not receive additional instructions beyond the mothers’ class. ‘Fetal music’ was a relaxing music composed of string instrument (music boxes) that lasted for about 30 minutes of gentle box music. In the fetal diary, there are provisions for space where mother could write about her fetal movements and her feelings (Figure 1). In the intervention group, participants listened to fetal music 2-3 times daily and wrote in a fetal diary every day.
Figure 1. Fetal Diary for Documentation of Fetal Movements and Mother’s Feelings
Both groups and both periods were screened for depression using the Edinburgh Postnatal Depression Scale (EPDS) and mothers’ attachment to the fetus/neonate was evaluated using the Mother-to-Infant Bonding Scale (MIBS) and the Prenatal Attachment Inventory (PAI)/Maternal Attachment Inventory (MAI) before and after delivery. Pregnant women were surveyed twice, once during an antepartum medical checkup and once during a postpartum medical checkup at 1 month after childbirth.
Participants
The participants were pregnant women who were in the hospital for regular term pregnancy medical prenatal checkup and participate in the mother’s class. Exclusion criteria were: pregnant women who had psychiatric disorder that needed treatment, those who did not consent and participants who gave birth in a different hospital.
Data Collection and Management
Measurements of depression and attachment:
EPDS: EPDS is a self-reported questionnaire composed of 10 items scored on a four-point Likert scale (0-3) designed to assess antepartum and postpartum depression.8 It does not include items related to physical symptoms because depression is not thought to be affected by physical symptoms in the postpartum period. The Japanese version of the EPDS uses a cutoff score of,9 with scores of 9 points or more indicating suspected depression after delivery 9. Therefore, in this study, EPDS scores were categorized as ≥9 points and ≤8 points.
MIBS: MIBS was developed by Kumar and Marks,10 and was translated into Japanese by Yamashita.9 MIBS is a self-reported questionnaire composed of 10 items on a four-point Likert scale. A high MIBS score indicates worse mother-to-infant bonding. If the MIBS score is zero, mothers do not have any bonding disorders.11 MIBS evaluates two factors, “lack of affection” and “anger and rejection”. “Anger and rejection” is used as a direct risk factor for child abuse.12
PAI/MAI: Prenatal Attachment Inventory (PAI) measures a mother’s attachment to the fetus and is scored on a four-point Likert scale (1-4). This questionnaire also measures a mother’s feelings and actions towards the fetus. Maternal Attachment Inventory (MAI) measures a mother’s attachment to the neonate and is scored on a four-point Likert scale (1-4). This questionnaire also measures a mother’s feelings and actions toward the newborn baby.13,14
Postpartum Obstetrics Data
Participants’ obstetrics data were collected from their postpartum medical records. Data were collected on; gestational in weeks at delivery, mode of delivery, duration of labor, vital signs immediately after delivery (i.e., temperature, pulse, blood pressure), baby’s weight and its vital signs, umbilical blood pH, and breast-feeding rate in the postpartum one month.
Data Analyses
SPSS Statistics 23 for Windows was used to analyze the variables. Antepartum and postpartum scores of EDPS and MIBS were tested using the paired t-test and Fisher’s exact test. The scores for the control group and intervention group were also tested using the paired t-test and Fisher’s exact test. The dependent variables were postpartum EPDS scores and MIBS scores, and the independent variables were each of the obstetrics data. Univariate logistic regression analysis was performed for these variables. The level of statistical significance was set to p<0.05.
Ethical Considerations
This study was approved by the ethics committee of the university (ID No. 14024-3) and the institutional review board of the participating hospital. All participants were given a detailed explanation of the study purpose and the confidentiality of the collected data. The participants were also told that they were free to withdraw their participation at any point. Verbal andWritten informed consent were was obtained from all participants.
RESULTS
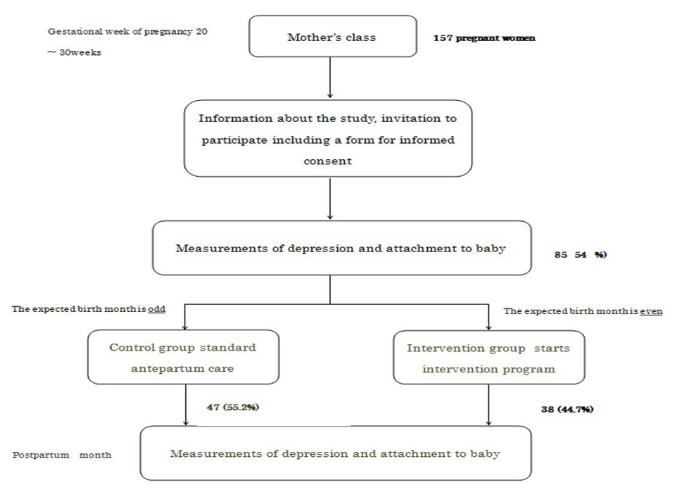
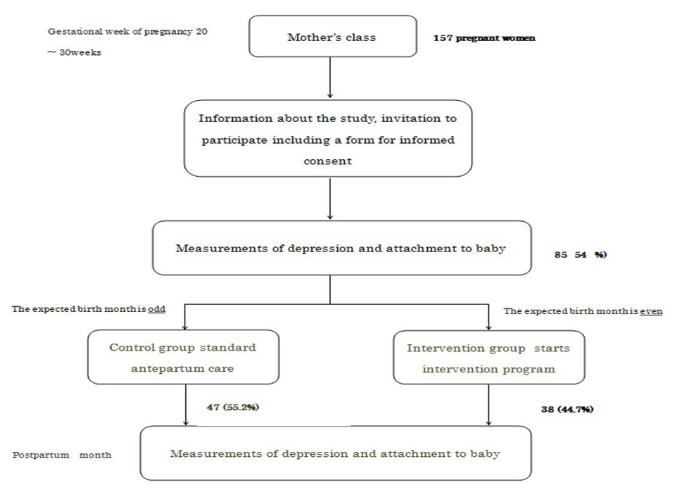
Out of the 157 pregnant women who provided informed consent, valid data was obtained for 85 (54.1%) (control group, n=47; intervention group, n=38) (depicted in Figure 2). The reasons for about half dropout rate were; no time to answer the questionnaire in the mother’s class or that she did not give birth at the study site.
Figure 2. Flow Chart of the Participant’s Enrollment
Antepartum and Postpartum Depressive State and Bonding Disorder
Table 1 shows the combined characteristics of intervention and controls. The mean gestational week of pregnancy was 21±5.7 weeks. Antepartum depressive state (EPDS score of 9 points or more) was present in 18.6%, while postpartum depressive state was present in 20.4%. The mean EPDS scores in the antepartum and postpartum periods in control were 4.6±4.2 points and 6.2±4.7 points, respectively. Furthermore, the mean EPDS scores in the antepartum and postpartum periods in intervention group were 5.7±3.6 points and 5.5±2.9 points, respectively. The mean±standard deviation MIBS scores in the antepartum and postpartum periods in control were 3.0±2.2 points and 2.6±2.1 points, respectively. In addition, the MIBS scores in the antepartum and postpartum periods in intervention group were 2.9±2.2 points and 2.1±2.1 points, respectively. The average PAI score during pregnancy in control group were 50.6±8.3 points and the postpartum MAI score were 87±12.4 points. Also, the average PAI score during pregnancy in intervention group were 55.2±14.9 points and the postpartum MAI score were 90±24 points.
| Table 1. Relationship between antepartum and Postpartum in Depressive State and Bonding Disorder |
|
Antepartum
|
Postpartum |
|
Control (n=47) |
Intervention (n=38) |
Control (n=47) |
Intervention (n=38)
|
|
EPDS
|
4.6±4.2 |
5.7±3.6 |
6.2±4.7 |
5.5±2.9 |
| MIBS |
3±2.2 |
2.9±2.2 |
2.6±2.1 |
2.1±2.1
|
|
PAI/MAI
|
50.6±8.3 |
55.2±14.9 |
87± 12.4 |
90±10.8 |
| Maternal Anxiety |
|
|
123±15 |
109±24
|
| Paire t-test *p<0.05 **p<0.001 |
There were significant differences in depressive state as assessed by the EPDS between the antepartum and postpartum periods in the control group. However, depressive state assessed by EPDS was higher postpartum than antepartum (p=0.05).
The Intervention Group Showed No Difference in Depression
Between the Antepartum Period and Postpartum Period
There were no significant differences in mothers’ attachment as assessed by MIBS between the control group and intervention group in the antepartum period. However, there were significant differences in MIBS score between the two groups in the postpartum than antepartum period being lower in the former group. The MIBS score of the control group was not different between antepartum and postpartum period. However, the MIBS scores of the intervention group were significantly lower in the postpartum period compared to antepartum period (p=0.001) (Table 1).
There was no difference between PAI and MAI in the both periods
Obstetrics Data
All participants in both the control and intervention groups delivered at full term. More than half had normal vaginal delivery.
There were differences in mothers’ pulse immediately after delivery between the control and intervention groups (p=0.05). The mother’s pulse immediately after delivery was lower in the intervention group than in the control group. Also, there were differences in umbilical blood pH between the control and intervention groups (p=0.05) (Table 2). There were no differences between the control and intervention groups in other obstetrics data.
| Table 2. Obstetrics Date of Participants |
|
Control (n=47)
|
Intervention (n=38)
|
| Gestational week at the delivery (days) |
274±8.7
|
275±10.9
|
| Mode of delivery normal vaginal delivery |
57.1%
|
61.5%
|
| Duration of labor (minutes) |
586±410
|
834±503
|
| Vital signs of immediately after delivery |
| Temperature (°C) |
37.0±0.4
|
37.2±0.6
|
| Pulse (time) |
82.9±11
|
74.9±9.4
|
| Maximal BP (mmHg) |
105±25
|
105.1±8
|
| Minimal BP (mmHg) |
64.6±12
|
62.9±9.4
|
| Baby’s Weight (lb) |
6±11.7
|
6±1.17
|
| Umbilical blood pH |
7.26±0.1
|
7.34±0.1
|
| Vital signs of immediately after birth |
| Temperature (°C) |
36.9±0.3
|
37±0.6
|
| Pulse (time) |
137.1±15
|
138.5±9.7
|
| Respiration (time) |
48.6±7.4
|
48.5±5.3
|
| Breast feeding only |
64.2%
|
84.6%
|
|
Paired t-test *p<0.05
|
DISCUSSION
The average number of gestational weeks of the participants in this study was 21±5.7 weeks. Since the second trimester is a stable period of pregnancy, it is a good time for a mother to physically and psychologically adapt to pregnancy. Also, it is a period when both primiparas and multiparas become aware of fetal movement. Therefore, it is believed that this was a psychologically appropriate time of pregnancy to conduct the present study.
About 19% of the participants were found in a depressive state in the antepartum period, which was slightly higher than the approximately 15% cited in previous studies.15,16,17 It is possible that depression during pregnancy may be increasing, and health care providers must pay attention to the fact that about 20% of women may be suffering from depression even during what might appear as a relatively uneventful pregnancy. Similarly, it was found that 20% of the participants were in a depressive state in the postpartum period; however, this result was consistent with the findings of previous studies.15 Thus, since the rate of postpartum depressive state was average, the sample of this study did not have high proportion of postpartum depression. Therefore, there was no problem to judge intervention effect MIBS scores between the control and intervention groups were not significantly different during pregnancy. The intervention group showed a greater reduction in mothers’ negative feelings towards the baby in the postpartum period compared to the antepartum period than the control group. Therefore, it is we believed that the intervention program was effective.
Pregnant women in the intervention group had a perception of their fetus by writing a “fetal diary”, listening to “fetal music”, and thinking about their fetus. It is reported that pregnant women begin to develop a mother-child relationship by perceiving their fetuses. However, it has also been found that once the baby is born and the mother can hold and nurse them, the mother’s negative feelings toward the baby reduce.5
It is reported that antepartum and postpartum depression are related and that postpartum depression is more common.15,18 There was almost no change in depressive state between the antepartum and postpartum periods in the intervention group, and EPDS scores increased significantly only in the control group. It is thought that performing an intervention program such as the one in the present study allows pregnant women to begin playing the role of mother by imagining her fetus, thereby influencing the process of psychologically becoming a mother. Nurturing during pregnancy period increases a mother’s awareness and attachment to the fetus.19 It is believed that increasing mothers’ awareness and attachment to the fetus and playing the role of mother during pregnancy may have contributed to maternal mental health in the postpartum period. In addition, attachment to the fetus becomes motivation for healthy behavior during pregnancy and facilitates a woman’s role as a mother.
Robertson et al20 examined the antenatal risk factors for postpartum depression and found that anxiety and depression were more likely when there were obstetric complications. In the intervention group in the present study, pulse immediately after delivery and umbilical blood pH were significantly lower than those in the control group. Although this may have contributed to lower rate of depression in the intervention group, further investigation is necessary to clarify the effectiveness of the intervention program in lowering depression.
CONCLUSION
This study supports the hypothesis that postpartum depression decreases when maternal and fetal bonding is promoted during pregnancy. We therefore recommend promoting ways/therapies to increase the maternal and fetal bonding.
LIMITATION OF STUDY
The limitations of this study were that the small number of participants. Furthermore, this being a hospital-based study, the findings cannot be generalized.
ACKNOWLEDGEMENTS
We are grateful to all the participants in this study. This study was supported by a Grant in-Aid for Young Scientists (B) (Grant No.24792507) from Japan Society for the Promotion of Science (JSPS) in Japan.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.