INTRODUCTION
Diabetes mellitus is chronic and crucial non-communicable disease (NCV) across the world.1 It may give various influence in social, medical and economic aspects.2 Then, some diabetic standard guidelines were presented for adequate diagnosis and treatment for better glycemic control.2 Chronic complications related to diabetes mellitus include both microvascular and macrovascular influences.1 Among them, a variety of mechanism has been involved in the development and aggravation of macroangiopathy, including vascular damage, neuronal dysfunction, interstitial injury, metabolic damage and others.1
Diabetes mellitus brings more incidence of various diabetic complications of foot.3 Among them, diabetic foot infection (DFI) has been crucial problem for actual diabetic practice. The reason includes persisting infection for long, necessary frequent visits, treatment of antibiotics, daily wound care, sometimes surgical procedures.4
DFI has been one of the macroangiopathy and complication to be necessary for hospitalization.5 It may show complex clinical course, with several exacerbation such as the amputation of lower extremities and economically high health costs.4 When patients have some degree of DFI, the prognosis would be poor from several reports.6 According to a prospective study, the prognosis of DFI showed that foot ulcer healed in 46% at 1-year, 15% of patients were dead and 17% had the amputation of lower extremity.6
For clinical practice and research of diabetes, the topic concerning DFI has been frequently discussed for long.7 Further, physicians majoring on diabetes pay attention to the prevention of DFI for long.7
On the other hand, the basic treatment of diabetes has been adequate diet. In recent years, the transition tendency has been found from the calorie restriction (CR) to low carbohydrate diet (LCD). LCD was formerly started by Bernstein and Atkins in the health and medical fields.8 Clinical effect was reported in comparison with CR and Mediterranean diet.9 After that, lots of comparison reports were found resulting in the predominant efficacy of LCD.10 Then, LCD has been more prevalent in European and North American region.
In Japan, the authors and colleagues have initiated the method of LCD, and developed LCD movement through Japanese LCD Promotion Association (JLCDPA).11 We have continued clinical research on LCD such as the comparison of blood glucose profiles in CR and LCD, Morbus (M) value, continuous glucose monitoring (CGM), meal tolerance test (MTT), elevated ketone bodies in the axis of fetus, placenta, pregnant mother and newborn, and so on.12,13,14 We have proposed three types of LCD meal pattern for everyone to understand LCD well and continue LCD easily. They are petite-, standard-, super-LCDs with 40%, 26%, 12% of carbohydrate ratio included.15,16
As mentioned above, we have continued clinical research on diabetic patients with various problems. Among them, there was a diabetic case who had diabetic foot osteomyelitis (DFO) in the category of DFI, operation of osteotomy and satisfactory effect on LCD. In this article, the impressive and suggestive case would be reported and discussed.
CASE REPORT
Present History
The case was 52-year-old female patient with T2DM for 10-years of duration. She had received the treatment of oral hyperglycemic agents (OHA) without no history of insulin treatment. For last 6-months, she had not treated enough for the diabetic control. During this period, her HbA1c value was persisted around 11-12% for half year. She had an outpatient consultation in January, 2020. At that time, she complained of the decreased sensation of right lower foot. Rapid exam of blood glucose and HbA1c revealed 430 mg/dL and 11.4% in the out clinic.
Physical Examination
Her physicals were as follows: consciousness was alert, the vitals were pulse 76/min, BP 187/90 mmHg, SpO 2 98%, BT 36.8 °C, respiration was normal, body weight 73 kg, stature 148 cm, body mass index (BMI) 33.3 kg/m2, unremarkable of lung, heart, abdomen. Her neurological reflexes of patellar (PTR) and Ankle (ATR) were decreased. There was remarkable change in the right 1st toe, which was a diabetic ulcer to gangrene in moderate to severe degree (DFO). This situation was evaluated to treat as soon as possible for save her life. Then, she was admitted to the hospital for further evaluation and treatment for the hyperglycemia and DFO in the right 1st toe.
Laboratory Test
Laboratory tests on the first visit were performed. The standard peripheral blood and biochemical data were: WBC 12100 /μL, RBC 4.72×106 /μL, Hb 13.0 g/dL, PLT 34.9×104 /μL, C-reactive protein (CRP) 13.5 mg/dL (5+), blood glucose 453 mg/dL, Cpeptide 4.1 ng/mL (0.8-2.5), AST 13U/L, ALT 14 U/L, r-GT 35 U/L, ALP 338 U/L (104-338), LDH 197 U/L (106-211), T-Bil 0.4 mg/dL, CPK 50 U/L (30-200), BUN 15 mg/dL, Creatinine 0.6 mg/dL, Uric acid 5.7 mg/dL, HBs Ag(-), HCV-Ab (-).
Examination on Admission
She received fundamental screening for several tests. Chest X-ray and electrocardiogram (ECG) were negative. Abdominal X-ray was unremarkable. Abdominal CT scan showed fatty liver. X-ray of right foot showed that right 1st proximal phalanx was damaged due to severe degree as osteomyelitis, and 1st metatarsal was unremarkable. Urinalysis showed that glucose (3+), protein (2+), urobilinogen (+). In ophthalmic detail examination, she has vague visual function with bilateral proliferative retinopathy. Her intraocular pressure was RT 23 mmHg, LT 18 mmHg. She showed that RV=0.08 (0.3x-1.25D)=CYL -2.75 DAX 50°, LV=0.1 (0.4x-2.25 D)=CYL -1.25 DAX 90°.
Diagnosis and Problem Lists
According to her medical history, she had not been treated diabetes enough for half year. Such situation has brought her current distress situation. She was diagnosed as the following problem lists. They were #1: Type 2 diabetes mellitus (T2DM), #2: osteomyelitis of 1st proximal phalanx in the right foot (DFO), #3 obesity (BMI 33.3), #4: hypertension, #5, diabetic neuropathy, #6 diabetic proliferative retinopathy, #7 diabetic nephropathy.
Concerning #1 and #3 mentioned above, her long his-tory will be summarized. The body weight was 52 kg at 20-years old (yo) and 64 kg at 24 yo. She kept weight about 50 kg for a while after marriage. After that, she came back to working as a nurse, and gradually increased up to 68 kg at 40 yo and 75 kg at 50 yo. The weight was 73 kg at this first visit (53 yo). Diabetes was pointed out about 10 years ago (43 yo) and has been receiving treatment intermittently since then.
Treatment for DFO
She has diagnosed to have osteomyelitis in the right 1st phalanx. According to the result of the culture from the infected area, detected bacteria was Streptococcus agalactiae (B group) (++). Then, sensitive kind of antibiotics was selected and the case was given cefmetazole sodium (D00911) 2 g per day, and continued. On the 5th day after admission, the data were rather improved with WBC 8800/μL, Hb 12.4 g/dL, CRP 1.5 mg/dL (++).
Nutritional Therapy
As for the nutritional therapy for diabetes, she was on the diabetes meal regimen for modified protocol of regular Japanese standard meal for CR by Japan Diabetes Association (JDA).17 JDA has proposed 50-60% of carbohydrate ratio of total energy per day, but our hospital has modified diabetic meal with 40% of carbohydrate ratio.
The detail of the meal and its calculation methods were as follows: i) stature of the case was 148 cm, then standard body weight becomes 48.2 kg (1.48×1.48×22=48.2), ii) standard calorie per day becomes 1205 kcal/day with (48.2 kg×25 kcal/kg=1205 kcal/day) (25 kcal/kg means sedentary lifestyle in the hospital), iii) the meal per day included 1250 kcal, protein 50 g, fat 48 g, carbohydrate 125 g, NaCl 7 g, water more than 1500 ml.
Insulin Treatment
She has started ACE Self-Assessment Program (ASAP) multiple daily insulin injection (MDI) with four times of insulin per day. She was given 2 kinds of insulin. One is Novo rapid (Novo Nordisk, Bagsværd, Denmark) three times a day just before three meals. Another is insulin Glargine (Eli Lilly and Company, Indiana, USA) at night at 2100 h. These two kinds in brand names were Insulin Aspart by pre-filled pen with 100 units/mL, and Insulin Glargine by BS injection kit FFP with 300 units/mL.
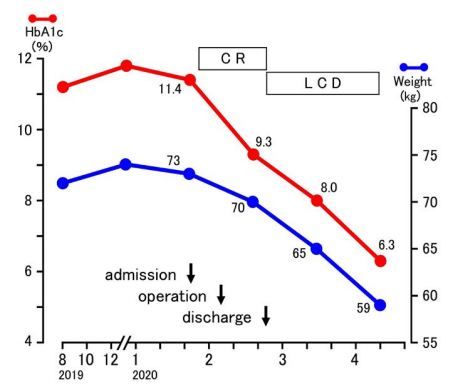
In this case, the control of blood glucose and insulin administration were shown in Table 1. The doses of Novo rapid three times a day were decided by the sliding scale method, according to the pre-prandial blood glucose before three meals. We used two kinds of sliding scale methods, which were middle degree and high degree. Due to 8 levels of blood glucose [<100, 101-, 151-, 201-, 251-, 301-, 351-, 401><mg/dL], the former indicates insulin doses [0, 4, 6, 9, 12, 14, 16, 19 units] and the latter indicates insulin doses [2, 6, 10, 12, 14, 16, 18, 21 units] by insulin aspart. High degree was used from day 4 to day 16 after admission. Table 1 (upper) showed the changes in blood glucose after admission. From admission to the operation, the profile of blood glucose profile during day 1-10 revealed higher values (Table 1, upper). They were almost 200-500 mg/dL and gradually decreased from day 11-17. After the operation, glucose profile decreased rapidly and kept stable situation during day 18-36. Progress Note The general status and DFO were gradually improved. On 17th day from the admission, she received the surgical operation of an amputation at the right toe. The osteotomy was performed between 1st metatarsal and proximal phalanx (Figure 1). The operation was successfully achieved and the progress condition after the operation showed improvement. After the operation, blood glucose showed improvement than before the operation (Table 1, middle). After 18-days of operation, she was discharged from the hospital. LCD without Insulin Just after the discharge, she started LCD. Daily profile of blood glucose without insulin is shown (Table 1, lower). Postprandial blood glucose was checked just after 60-minutes, when the max value of hyperglycemia is usually observed. Without Novo rapid insulin, postprandial glucose 1-hour after meal was stable around 130-160 mg/dL. Her glucose variability persisted satisfactory after discharge on day 1-48 (Table 1, lower). After her blood glucose rapidly dropped, there was no progression of retinopathy. She has no hypoglycemic episode so far, and her visual acuity has been not changed. Further, the degree of the proteinuria has reduced from ++ to +/-. The blood level of ketone bodies were not determined, and will be followed as the meal of LCD continues. Changes in HbA1c and Weight Changes in HbA1c value were observed in the following: 11-12% during August 2019- December 2019, 11.4% in January 2020, 9.3% in February, 8.0% in March, 6.3% in April (Figure 2). Changes in body weight were as follows: 72-74 kg during August 2019-December 2019, 73 kg in January 2020, 70 kg in February, 65 kg in March and 59 kg in April (Figure 2).><100, 101-, 151-, 201-, 251-, 301-, 351-, 401<mg/dL], the former indicates insulin doses [0, 4, 6, 9, 12, 14, 16, 19 units] and the latter indicates insulin doses [2, 6, 10, 12, 14, 16, 18, 21 units] by insulin aspart. High degree was used from day 4 to day 16 after admission.
Figure 1. X-ray of the Bilateral Feet After the Operation

Figure 2. Changes in HbA1c and Weight Associated with Operation and LCD
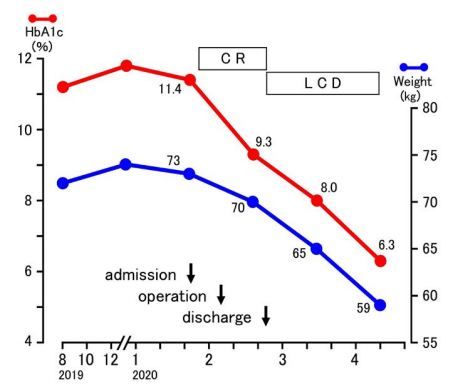
Table 1 (upper) showed the changes in blood glucose after admission. From admission to the operation, the profile of blood glucose profile during day 1-10 revealed higher values (Table 1, upper). They were almost 200-500 mg/dL and gradually decreased from day 11-17. After the operation, glucose profile decreased rapidly and kept stable situation during day 18-36.
Table 1. Changes in Daily Profile of Blood Glucose Before and After the Operation
|
|
Daily Profile of Blood Glucose (mg/dL)
|
|
Aspart Glargine
|
| Month |
Date |
Day |
|
700 h |
1100 h |
1700 h |
2100 h
|
3 times |
once |
|
|
|
|
0 min
|
60 min
|
0 min
|
60 min
|
0 min
|
60 min
|
units/day |
units/day |
|
January |
20
|
1
|
Admission |
|
|
|
|
396
|
|
451
|
|
P
|
|
21
|
2
|
396
|
|
524
|
|
378
|
|
273
|
26
|
6
|
|
22
|
3
|
263
|
|
359
|
|
313
|
|
367
|
32
|
7
|
|
24
|
5
|
196
|
|
343
|
|
251
|
|
234
|
29
|
8
|
|
27
|
8
|
172
|
|
256
|
|
238
|
|
233
|
29
|
9
|
|
30
|
11
|
190
|
|
231
|
|
220
|
|
225
|
28
|
10
|
|
February |
2
|
14
|
161
|
|
202
|
|
140
|
|
242
|
24
|
10
|
|
5
|
17
|
Operation |
202
|
|
239
|
|
167
|
|
129
|
29
|
10
|
|
6
|
18
|
136
|
|
185
|
|
193
|
|
128
|
26
|
10
|
|
7
|
19
|
154
|
|
153
|
|
125
|
|
183
|
26
|
10
|
|
10
|
22
|
185
|
|
155
|
|
137
|
|
144
|
26
|
10
|
|
14
|
26
|
142
|
|
176
|
|
125
|
|
118
|
22
|
10
|
|
18
|
30
|
128
|
|
170
|
|
141
|
|
134
|
22
|
10
|
|
24
|
36
|
159
|
|
102
|
|
127
|
|
105
|
22
|
10
|
|
25
|
1
|
|
126
|
|
150
|
|
130
|
|
131
|
22
|
10
|
|
26
|
2
|
|
132
|
142
|
|
133
|
|
143
|
|
0
|
10
|
|
27
|
3
|
|
110
|
132
|
122
|
138
|
110
|
162
|
154
|
0
|
10
|
|
29
|
5
|
|
117
|
|
119
|
145
|
123
|
158
|
147
|
0
|
8
|
|
2
|
7
|
Discharge |
116
|
151
|
127
|
135
|
162
|
148
|
149
|
0
|
8
|
|
5
|
10
|
106
|
140
|
107
|
144
|
113
|
141
|
113
|
0
|
6
|
|
10
|
15
|
112
|
|
|
150
|
|
154
|
136
|
0
|
6
|
| March |
15
|
20
|
|
132
|
|
207
|
160
|
169
|
166
|
0
|
4
|
|
25
|
25
|
|
142
|
|
164
|
125
|
127
|
120
|
0
|
4
|
|
26
|
31
|
110
|
133
|
|
136
|
|
169
|
149
|
0
|
0
|
|
31
|
36
|
114
|
|
|
166
|
|
116
|
118
|
0
|
0
|
| April |
12
|
48
|
|
133
|
|
118
|
|
114
|
106
|
0
|
0
|
Progress Note
The general status and DFO were gradually improved. On 17th day from the admission, she received the surgical operation of an amputation at the right toe. The osteotomy was performed between 1st metatarsal and proximal phalanx (Figure 1). The operation was successfully achieved and the progress condition after the operation showed improvement. After the operation, blood glucose showed improvement than before the operation (Table 1, middle). After 18-days of operation, she was discharged from the hospital.
LCD without Insulin
Just after the discharge, she started LCD. Daily profile of blood glucose without insulin is shown (Table 1, lower). Postprandial blood glucose was checked just after 60-minutes, when the max value of hyperglycemia is usually observed. Without Novo rapid insulin, postprandial glucose 1-hour after meal was stable around 130-160 mg/dL. Her glucose variability persisted satisfactory after discharge on day 1-48 (Table 1, lower).
After her blood glucose rapidly dropped, there was no progression of retinopathy. She has no hypoglycemic episode so far, and her visual acuity has been not changed. Further, the degree of the
proteinuria has reduced from ++ to +/-. The blood level of ketone bodies were not determined, and will be followed as the meal of LCD continues.
Changes in HbA1c and Weight
Changes in HbA1c value were observed in the following: 11-12% during August 2019- December 2019, 11.4% in January 2020, 9.3% in February, 8.0% in March, 6.3% in April (Figure 2). Changes in body weight were as follows: 72-74 kg during August 2019-December 2019, 73 kg in January 2020, 70 kg in February, 65 kg in March and 59 kg in April (Figure 2).
Current Medication
During the admission, she was provided insulin treatment. After her discharge from the hospital, she discontinued insulin therapy, and started metformin 500 mg a day for diabetes mellitus, and Aimix® Combination Tablets LD or HD (amlodipine 5 or 10 mg, irbesartan 100 mg) a day for hypertension. After discharge, her diabetic and hypertensive condition has been stable without any problems.
DISCUSSION AND CONCLUSION
In this article, a diabetic case was presented who suffered fromDFI and DFO, received the osteotomy of right toe, and showed remarkable improvement of glucose variability by LCD. Discussion would be described from some points of view.
Firstly, the background of the patient was a registered nurse working hard for years. Possible causes related to current serious condition were as follows: i) the work has been irregular due to day shift and night shift, ii) the stress of work was persisted for long, iii) necessary care of her two children at home, iv) general malaise from various stresses physically and psychologically, v) irregular medications with poor compliance or resilience. These factors might become exacerbating influence to the clinical course of this case.
As regard to her diabetic control, hyperglycemia seemed to be continued more than half a year. During that time, she did not have any consciousness disorder due to hyperglycemia, and was able to perform normal nurse duties. The body seemed to be accustomed to long-term hyperglycemia.
The weight was probably maintained about the same level for half a year. There were weakened tendon reflexes, impaired perception, and neuropathy. As to visual acuity, she cannot hold a clear visual field because of the proliferative retinopathy. She has some numbness in hand and foot at the extremities as neuropathy. Proteinuria as nephropathy has also persisted. Consequently, the existence of three types of microangiopathy were bound. On the other hand, detail presence of macroangiopathy would be investigated such as brain, heart, and feet.
Secondly, the case suffered from DFI. There has been some development in the light of DFI. From international necessity of management of DFI, there have been several guidelines. The standard one is from International Working Group on the Diabetic Foot (IWGDF). It has continuously published the guidelines every 4-years since 2004.18 The prevalent edition includes the format of standard content.18 Furthermore, it incorporates necessary information of systematic reviews about the interventions for DFI.19
Recently, new IWGDF Guideline on the diagnosis and treatment of foot infection for diabetic patient was presented in 2019.20,21 It has 7 guidelines, which was structured using the patient-intervention comparison-outcome (PICO) format.22,23 IWGDF has also produced systematic review on DFO.22 In 2019 updated IWGDF guideline is supported by reviews for diagnosis24 and interventions of DFI.25
For current case, Streptococcus was identified in bacterial culture from an infected wound on the foot. There are known studies of this in foot infections for diabetes. In the category of DFI, rather severe DFO is present. Regarding DFO, narrative review was conducted, in which 65 papers were included from 756 related reports.26 Formerly in the pre-antibiotic era, DFO by staphylococcus had 50% of mortality. Recent situation shows usually polymicrobial with gram-negative and positive bacilli can be identified by the modern molecular techniques.26
Regarding the epidemiology for osteomyelitis, DFO shows rarely mono-microbial organism. There are often polymicrobial results, including Staphylococcus aureus (at most 50%), Staphylococcus epidermidis (around 25%), Streptococci (around 30%) and Enterobacteriaceae (at most 40%). These bacteria have been usually detected in DFO.18,27 In contrast, the proportion of the anaerobes has been usually low. Gram negative bacteria usually include Escherichia coli, Klebsiella pneumoniae and Proteus, and Pseudomonas aeruginosa. 18,27
Long-term prospective study was conducted for limb amputation and mortality after the first neuropathic diabetic foot ulcer (DFU).28 Subjects were 2880 patients with neuropathic DFU group (DFU) and diabetic patients without DFU group (nDFU), and followed-up 14-years. For median follow-up 7-years, death rate was 17.4% (n=501) vs 3.1% (n=89).28 The 5-/10-year mortality was 22%/71% with survival of 7.72-years, in DFU group, while 3%/5% with 12.6-years in nDFU group (all showed significant difference). DFU group showed 29.3% of limb amputations. Odd ratio (OR) was 1.31 in DM duration >10-years, 1.47 in nephropathy, 1.85 in minor amputation, 2.96 in major amputation, respectively, which could predict mortality.28
Thirdly, an impressive clinical course was found associated with DFI and/or DFO. After admission, blood glucose control was performed by the sliding scale method. Although the sliding scale method revealed stronger level than usual, the blood glucose level remained high at around 200-500 mg/dL during continuous administration of insulin. Blood glucose control had been resistant, and its cause seemed to be due to strong inflammatory state from foot infection.
After the operation, the daily profile of blood glucose became rapidly stable. Preprandial glucose was 100-200 mg/dL. This process was supposed to be from reduced inflammatory state from DFO. As to the changes in CRP value, it decreased to 13.5 mg/dL (day 1) was decreased to, 1.5 mg/dL (day 6) and 1.5 mg/dL (day 10). There are reports on the extent of CRP increase.
In the clinical diabetic practice, differential diagnosis of osteomyelitis and soft-tissue infection has been clinically important.29 Because the former needs the possibility of more antibiotic administration, operation and amputation. For distinguishing osteomyelitis, optimal cut off values for ESR and CRP were investigated. The threshold of 60 mm/h in ESR showed sensitivity of 74% sensitivity and specificity of 56%. In contrast, threshold of 7.9 mg/dL in CRP had 49% sensitivity and 80% specificity.29
Fourthly, clinical effect of LCD was demonstrated in this case. During her stay in the hospital, she was on CR with 125 g of carbohydrate associated with insulin.30 During this period, her weight reduction was mild. The reason was that both carbohydrate intake and insulin administration were present. On the other hand, after discharge from the hospital, neither intake of sugar nor increase in blood insulin concentration was continued. Therefore, body weight seemed to be decreased rapidly.
After discharge from the hospital, the meal was switched from CR to LCD immediately. During admission, it is difficult to cut staple foods for regular meals. On the other hand, outpatients can delete carbohydrate food completely, while much amount of vegetables and protein can be taken. Therefore, fast-acting Aspart insulin was immediately discontinued, and only metformin 500 mg was
given as oral hyperglycemic agent (OHA). Generally speaking, postprandial blood glucose is highest at 30-60-minutes. This case showed stable blood glucose level 60 min after meal, indicating satisfactory efficacy of LCD.
In this case, the body weight was reduced from 73 kg to 59 kg and HbA1c was reduced from 11.4 to 6.3% in less than 3-months. We have already reported concerning the effect of weight reduction by LCD.31 As a result of LCD for 2699 cases, weight loss of 10% or more was observed in 25.6%, and weight loss of 5% or more was 57.6%, which showed enough clinical effect of LCD. It is effective to teach the LCD method for obese and diabetic patients and to continue LCD. We have developed LCD movement by English papers, books and seminars through JLCDPA. Depending on the situation, petite-, standard-, super-LCD can be applied and treated.16,32
Regarding the limitations of this paper, we report on the surgical treatment of foot infection in diabetic patients (DFI, DFO) and the effect on LCD. For foot infections, soft tissue can be mild and osteomyelitis can be severe. As future work, it may be necessary to examine the severity of infectious diseases, the types of bacteria that cause the infections, the effects of antimicrobial agents, and the response of other biomarkers. With respect to LCDs, it was shown that the increase in postprandial blood glucose was suppressed by LCD. Furthermore, detailed intake of food and postprandial blood glucose should be examined in the future.
In summary, we reported a case of a diabetic patient who underwent surgery for diabetic foot osteomyelitis (DFO) and was able to control blood glucose with LCD. We hope that this report will be useful for the management of diabetic complications and blood glucose control.
ACKNOWLEDGEMENT
None.
FUNDING
None.
CONSENT
The authors have received written informed consent from the patient.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.