INTRODUCTION
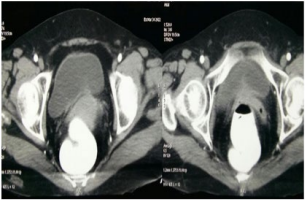
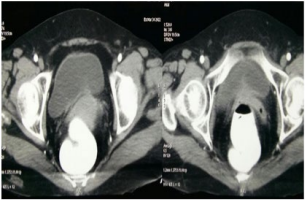
Unlike urethral melanoma, malignant melanoma originating from the urinary bladder is very rare.1,2 Melanoma of the bladder is mostly secondary presentation of patients with widespread metastatic melanoma originating from the skin.3 Exclusion of other melanoma sites is mandatory to confirm primary bladder melanoma. Here, we report a patient who presented with gross hematuria, and after detailed workup, the diagnosis of primary malignant melanoma (PMM) of the bladder was made (Figure 1).
Figure 1. Irregular Enhancing Mucosal Thickening at the Bladder Neck for the Length of 7 mm and Maximum Depth of 1.5 mm
CASE REPORT
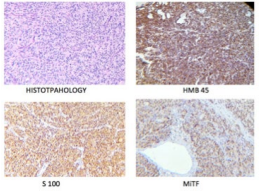
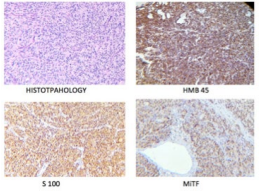
A 55-year-old woman underwent transurethral resection (TUR) of the bladder tumor for gross hematuria for 2-months at private hospital. The resected specimen examination showed histological features of high-grade urothelial carcinoma (Figure 2). Upon microscopic evaluation, the tumour was predominantly composed of atypical urothelial cell arranged in syncytial sheets, nests and diffuse pattern. Tumour cells show moderate to severe pleomorphism, round to oval coarse granular chromatin, prominent nucleoli and moderate amount of cytoplasm. At places, tumor cells are highly atypical with large spindled nuclei and vacuolated cytoplasm, many multinucleated tumor giant cells and bizarre cells seen. Vascular proliferation with areas of hemorrhage and necrosis seen. High mitotic activity noted (>15-20 per 10 hpf). Immunohistochemistry revealed S-100- +ve, MiTF- +ve, HMB45- +ve, Melan A- +ve suggestive of Malignant Melanoma.
Figure 2. Both Superficial and Deep Biopsy Shows Histopathological Features of Malignant Melanoma. IHC Positive for S-100m MiTF and HMB45
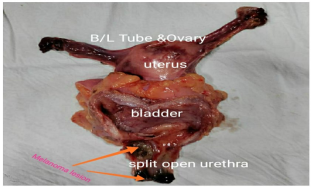
After hospitalisation in our hospital, investigation was undertaken to exclude other primary sites as the source of the melanoma. Careful dermatological examination of the whole body and ophthalmologic evaluations were negative. Contrast enhanced computerized tomography (CECT) of thorax and abdomen revealed irregular enhancing mucosal thickening at the bladder neck of 7 mm and maximum depth of 1.5 mm and adjacent urinary bladder, post-operative reactionary or neoplastic etiology. No evidence of bulky enhancing mass seen in urinary bladder. No evidence of involvement of vagina, cervix or uterus and rest of the abdominal and thoracic organ appeared normal. Therefore, PMM of the bladder was confirmed after extensive history, physical examination, and workup. Three months since her symptoms of hematuria the patient underwent open radical cystectomy with anterior pelvic exenteration with bilateral pelvic lymphnode dissection with ileal conduit (Figure 3). The specimen was sent for analysis.
Figure 3. Labelled Specimen of Anterior Pelvic Exenteration Showing Melanoma Lesion Near Bladder Neck and External Urethral Meatus
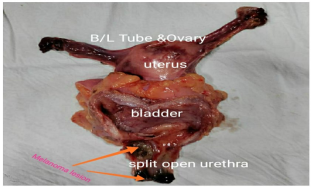
Patient post-operative stay was uneventful. Liquids were allowed on post-operative day (POD-3) and patient started full diet from POD-6 and was discharged on POD-8. Histopathological findings were suggestive of malignant melanoma extending from bladder neck to external urethral meatus with invasion in lamina propria.
DISCUSSION
Primary malignant melanoma is very rare in the genitourinary tract,1 especially in the bladder. Most of the cases present with hematuria and/or dysuria as initial symptom.2 It is most commonly secondary to melanoma occurring at other sites.4 Very few cases of primary melanoma of the urinary bladder have been previously reported.5 A detailed history, examination of the patient’s skin, and evaluation for other visceral primary sites are needed for confirmation of the primary nature of the tumor.
Wheelock was the first to report a primary melanoma of the bladder in 1942, then Su reported one case in 1962, followed by Anichkov et al6 who reported 2 cases of primary bladder melanoma. The primary bladder melanoma is extremely rare, and probably none of those previously reported cases truly arose from the bladder.7
Most of the time bladder melanoma is metastatic. Thorough examination of patient is required to established diagnosis of PMM. Proposed criteria for designating bladder melanoma as a primary lesion: (1) no previous cutaneous lesion; (2) no history of regressed cutaneous malignant melanoma; (3) no evidence of any other visceral primary melanoma; (4) the pattern of recurrence should be consistent with the initial lesion; and (5) the margins of the bladder lesion should contain atypical melanocytes.7 Therapy of choice for localized tumor should be radical surgery, although prognosis is poor.
CONCLUSION
Melanoma of urinary bladder commonly presents secondary to metastatic urinary bladder with primary originating from skin. Radical surgery is treatment option going forward. The prognosis is guarded even after the radical surgery.
Primary or metastatic malignant melanoma of bladder is difficult to differentiate owing to similar histological presentation, similar aggressiveness, advance stage of presentation and its rarity. A careful review of histological features and necessary immunehistochemical staining procedures for S-100 and HMB-45 are very important in achieving a correct diagnosis.
At present, there is no universally accepted treatment modalities, but its poor prognosis is consistent. In conclusion, due to the rarity of PMM of the bladder, evidence regarding etiology, risk factors, histopathological diagnosis, and treatment options remains in question.
FUNDING
None.
CONSENT
The authors have received written informed consent from the patient.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.