1. Beck-Peccoz P, Persani L. Premature ovarian failure. Orpha- net J Rare Dis. 2006; 1: 9. doi: 10.1186/1750-1172-1-9
2. Santoro N. Mechanisms of premature ovarian failure. Ann Endocrinol(Paris).2003;64(2):87-92. doi: AE-04-2003-64-2- 0003-4266-101019-ART06
3. Timmreck LS, Reindollar RH. Contemporary issues in primary amenorrhea. Obstet Gynecol Clin North Am. 2003; 30(2): 287-302. doi: 10.1016/S0889-8545(03)00027-5
4. Jin M, Yu Y, Huang H. An update on primary ovarian insufficiency. Sci China Life Sci. 2012; 55(8): 677-686. doi: 10.1007/s11427-012-4355-2
5. Hernández-Angeles C, Castelo-Branco C. Early menopause: A hazard to a woman’s health. Indian J Med Res. 2016; 143(4): 420-427. doi: 10.4103/0971-5916.184283
6. Kumar M, Pathak D, Venkatesh S, Kriplani A, Ammini AC, Dada R. Chromosomal abnormalities & oxidative stress in women with premature ovarian failure (POF). Indian J Med Res. 2012; 135(1): 92-97. doi: 10.4103/0971-5916.93430
7. Rebar RW, Connolly HV. Clinical features of young women with hypergonadotropic amenorrhea. Fertil Steril. 1990; 53(5): 804-810.
8. Nelson LM. Primary ovarian insufficiency. N Engl J Med. 2009; 360(6): 606-614. doi: 10.1056/NEJMcp0808697
9. Hewlett M, Mahalingaiah S. Update on primary ovarian in- sufficiency. Curr Opin Endocrinol Diabetes Obes. 2015; 22(6): 483-489. doi: 10.1097/MED.0000000000000206
10. Pouresmaeili F, Fazeli Z. Premature ovarian failure: A criti- cal condition in the reproductive potential with various genetic causes. Int J Fertil Steril. 2014; 8(1): 1-12. Website. http://ijfs. ir/journal/article/fulltext/3756.html. Accessed January 27, 2017.
11. Sükür YE, Kıvançlı IB, Ozmen B. Ovarian aging and pre- mature ovarian failure. J Turk Ger Gynecol Assoc. 2014; 15(3): 190-196. doi: 10.5152/jtgga.2014.0022
12. Fenton AJ. Premature ovarian insufficiency: Pathogenesis and management. J Midlife Health. 2015; 6(4): 147-153. doi: 10.4103/0976-7800.172292
13. Research on the menopause in the 1990s. Report of a WHO Scientific Group. World Health Organ Tech Rep Ser. 1996; 866: 1-107.
14. Bakalov VK, Anasti JN, Calis KA, et al. Autoimmune oo- phoritis as a mechanism of follicular dysfunction in women with 46, XX spontaneous premature ovarian failure. Fertil Steril. 2005; 84(4): 958-965.
15. Little DT, Ward HR. Adolescent premature ovarian in- sufficiency following human papillomavirus vaccination: A case series seen in general practice. J Investig Med High Impact Case Rep. 2014; 2(4): 2324709614556129. doi: 10.1177/2324709614556129
16. Taylor AE. Systemic adversities of ovarian failure. J Soc Gynecol Investig. 2001; 8(1): S7-S9. Website. http://journals.sage- pub.com/doi/abs/10.1177/1071557601008001s03. Accessed January 27, 2017.
17. Snowdon DA, Kane RL, Beeson WL, et al. Is early natural menopause a biologic marker of health and aging? Am J Public Health. 1989; 79(6): 709-714. doi: 10.2105/AJPH.79.6.709
18. Goswami D, Conway GS. Premature ovarian failure. Hum Reprod Update. 2005; 11(4): 391-410. doi: 10.1093/humupd/dmi012
19. Maiti GD. Premature ovarian failure: A chronic debilitating condition of womanhood. In: Talwar P, ed. Manual of Cytoge- netics in Reproductive Biology. London, UK: JP Medical Ltd; 2014: 119-120.
20. Zangmo R, Singh N, Sharma JB. Diminished ovarian reserve and premature ovarian failure: A review. IVF Lite. 2016; 3(2): 46-51. doi: 10.4103/2348-2907.192284
21. Luborsky JL, Meyer P, Sowers MF, Gold EB, Santoro N. Premature menopause in a multi-ethnic population study of the menopause transition. Hum Reprod. 2003; 18(1): 199-206. doi: 10.1093/humrep/deg005
22. Skillern A, Rajkovic A. Recent developments in identify- ing genetic determinants of premature ovarian failure. Sex Dev. 2008; 2(4-5): 228-243. doi: 10.1159/000152039
23. Nelson LM, Covington SN, Rebar RW. An update: Sponta- neous premature ovarian failure is not an early menopause. Fer- til Steril. 2005; 83(5): 1327-1332.
24. Sklar CA, Mertens AC, Mitby P, et al. Premature menopause in survivors of childhood cancer: A report from the childhood cancer survivor study. J Natl Cancer Inst. 2006; 98(13): 890- 896. doi: 10.1093/jnci/djj243
25. Panay N, Fenton A. Premature ovarian failure: A grow- ing concern. Climacteric. 2008; 11(1): 1-3. doi: 10.1080/1369 7130701878635
26. Murabito JM, Yang Q, Fox C, Wilson PW, Cupples LA. Her- itability of age at natural menopause in the framingham heart study. J Clin Endocrinol Metab. 2005; 90(6): 3427-3430. doi: 10.1210/jc.2005-0181
27. Picton HM, Harris SE, Muruvi W, Chambers EL. The in vitro growth and maturation of follicles. Reproduction. 2008; 136(6): 703-715. doi: 10.1530/REP-08-0290
28. Shelling AN. Premature ovarian failure. Reproduction. 2010; 140(5): 633-641. doi: 10.1530/REP-09-0567
29. Persani L, Rossetti R, Cacciatore C. Genes involved in hu- man premature ovarian failure. J Mol Endocrinol. 2010; 45(5): 257-279. doi: 10.1677/JME-10-0070
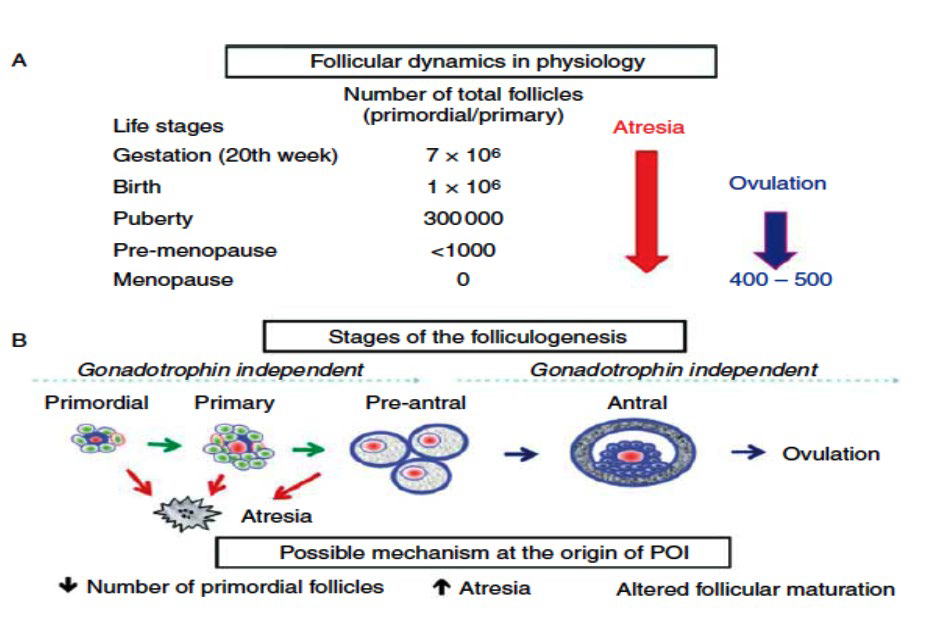
30. Morita Y, Tilly JL. Oocyte apoptosis: Like sand through an hourglass. Dev Biol. 1999; 213(1): 1-17. doi: 10.1006/dbio.1999.9344
31. Sullivan SD, Castrillon DH. Insights into primary ovarian insufficiency through genetically engineered mouse models. Se- min Reprod Med. 2011; 29(4): 283-298. doi: 10.1055/s-0031- 1280914
32. Fortuño C, Labarta E. Genetics of primary ovarian insuf- ficiency: A review. J Assist Reprod Genet. 2014; 31(12): 1573- 1585. doi: 10.1007/s10815-014-0342-9
33. Chapman C, Cree L, Shelling AN. The genetics of prema- ture ovarian failure: Current perspectives. Int J Womens Health. 2015; 7: 799-810. doi: 10.2147/IJWH.S64024
34. Jiao X, Qin C, Li J, et al. Cytogenetic analysis of 531 Chi- nese women with premature ovarian failure. Hum Reprod. 2012; 27(7): 2201-2207. doi: 10.1093/humrep/des104
35. Simpson JL. Genetic and phenotypic heterogeneity in ovar- ian failure: Overview of selected candidate genes. Ann N Y Acad Sci. 2008; 1135: 146-154. doi: 10.1196/annals.1429.019
36. Luisi S, Orlandini C, Regini C, Pizzo A, Vellucci F, Petraglia F. Premature ovarian insufficiency: From pathogenesis to clini- cal management. J Endocrinol Invest. 2015; 38(6): 597-603. doi: 10.1007/s40618-014-0231-1
37. Cox L, Liu JH. Primary ovarian insufficiency: An update. Int J Womens Health. 2014; 6: 235-243. doi: 10.2147/IJWH.S37636
38. Holland CM. 47, XXX in an adolescent with premature ovar- ian failure and autoimmune disease. J Pediatr Adolesc Gynecol. 2001; 14(2): 77-80. doi: 10.1016/S1083-3188(01)00075-4
39. Cordts EB, Christofolini DM, Dos Santos AA, Bianco B, Barbosa CP. Genetic aspects of premature ovarian failure: A literature review. Arch Gynecol Obstet. 2011; 283(3): 635-643. doi: 10.1007/s00404-010-1815-4
40. Tartaglia NR, Howell S, Sutherland A, Wilson R, Wilson L. A review of trisomy X (47,XXX). Orphanet J Rare Dis. 2010; 5: 8. doi: 10.1186/1750-1172-5-8
41. Nolin SL, Brown WT, Glicksman A, et al. Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am J Hum Genet. 2003; 72(2): 454-464. doi: 10.1086/367713
42. American College of Obstetricians and Gynecologists Com- mittee on Genetics. ACOG committee opinion. No. 338: Screening for fragile X syndrome. Obstet Gynecol. 2006; 107(6): 1483- 1485.
43. Ebrahimi M, Akbari Asbagh F. Pathogenesis and causes of premature ovarian failure: an update. Int J Fertil Steril. 2011; 5(2): 54-65. Website. http://ijfs.ir/journal/article/fulltext/2905. html. Accessed January 27, 2017.
44. Hagerman RJ, Hagerman PJ. The fragile X premutation: Into the phenotypic fold. Curr Opin Genet Dev. 2002; 12(3): 278- 283. doi: 10.1016/S0959-437X(02)00299-X
45. Bear MF, Huber KM, Warren ST. The mGluR theory of fragile X mental retardation. Trends Neurosci. 2004; 27(7): 370-377. doi: 10.1016/j.tins.2004.04.009
46. Fiçicioglu C, Yildirim G, Attar R, Kumbak B, Yesildaglar N. The significance of the number of CGG repeats and autoantibod- ies in premature ovarian failure. Reprod Biomed Online. 2010; 20(6): 776-782. doi: 10.1016/j.rbmo.2010.02.011
47. Sullivan AK, Marcus M, Epstein MP, et al. Association of FMR1 repeat size with ovarian dysfunction. Hum Reprod. 2005; 20(2): 402-412. doi: 10.1093/humrep/deh635
48. Wittenberger MD, Hagerman RJ, Sherman SL, et al. The FMR1 premutation and reproduction. Fertil Steril. 2007; 87(3): 456-65. doi: 10.1016/j.fertnstert.2006.09.004
49. Sherman SL. Premature ovarian failure in the fragile X syndrome. Am J Med Genet. 2000; 97(3): 189-194. doi: 10.1002/1096-8628(200023)97:3<189::AID-AJMG1036> 3.0.CO;2-J
50. Hagerman RJ, Leavitt BR, Farzin F, et al. Fragile-X-associated tremor/ataxia syndrome (FXTAS) in females with the FMR1 premutation. Am J Hum Genet. 2004; 74(5): 1051-1056. doi: 10.1086/420700
51. Van Esch H. The fragile X permutation: New insights and- clinical consequences. Eur J Med Genet. 2006; 49(1): 1-8. doi: 10.1016/j.ejmg.2005.11.001
52. Hundscheid RD, Sistermans EA, Thomas CM, et al. Imprint- ing effect in premature ovarian failure confined to paternally inherited fragile X premutations. Am J Hum Genet. 2000; 66(2): 413-418. doi: 10.1086/302774
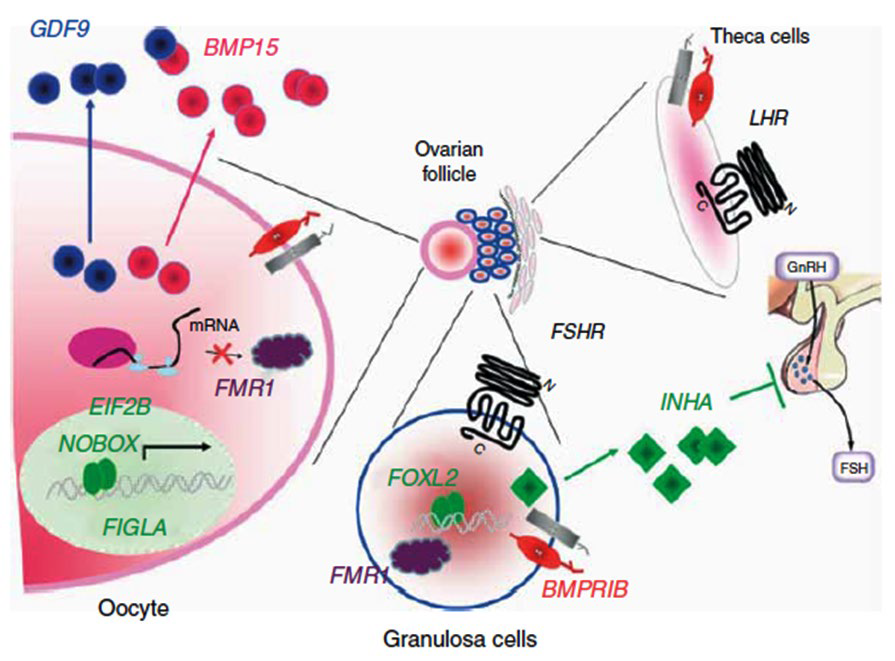
53. McNatty KP, Moore LG, Hudson NL, et al. The oocyte and its role in regulating ovulation rate: A new paradigm in reproductive biology. Reproduction. 2004; 128(4): 379-386. Website. http://www.reproduction-online.org/content/128/4/379.short. Accessed January 27, 2017.
54. Shimasaki S, Moore RK, Otsuka F, Erickson GF. The bone morphogenetic protein system in mammalian reproduction. Endocr Rev. 2004; 25(1): 72-101. doi: 10.1210/er.2003-0007
55. Persani L, Rossetti R, Cacciatore C, Bonomi M. Primary Ovarian Insufficiency: X chromosome defects and autoimmunity. J Autoimmun. 2009; 33(1): 35-41. doi: 10.1016/j. jaut.2009.03.004
56. Di Pasquale E, Beck-Peccoz P, Persani L. Hypergonado- tropic ovarian failure associated with an inherited mutation of human bone morphogenetic protein-15 (BMP15) gene. Am J Hum Genet. 2004; 75(1): 106-111. doi: 10.1086/422103
57. Laissue P, Christin-Maitre S, Touraine P, et al. Mutations and sequence variants in GDF9 and BMP15 in patients with premature ovarian failure. Eur J Endocrinol. 2006; 154(5): 739-744. doi: 10.1530/eje.1.02135
58. Rossetti R, Di Pasquale E, Marozzi A, et al. BMP15 mutations associated with primary ovarian insufficiency cause a defective production of bioactive protein. Hum Mutat. 2009; 30(5): 804-810. doi: 10.1002/humu.20961
59. Wang B, Wen Q, Ni F, et al. Analyses of growth differen- tiation factor 9 (GDF9) and bone morphogenetic protein 15 (BMP15) mutation in chinese women with premature ovarian failure. Clin Endocrinol (Oxf). 2010; 72(1): 135-136. doi: 10.1111/j.1365-2265.2009.03613.x
60. Ohkubo M, Yabu T, Yamashita M, Shimizu A. Molecular cloning of two gonadotropin receptors in mummichog Fundulus heteroclitus and their gene expression during follicular development and maturation. Gen Comp Endocrinol. 2013; 184: 75-86. doi: 10.1016/j.ygcen.2012.12.019
61. Wei S, Chen S, Gong Z, et al. Alarelin active immunization influences expression levels of GnRHR, FSHR and LHR proteins in the ovary and enhances follicular development in ewes. Anim Sci J. 2013; 84(6): 466-475. doi: 10.1111/asj.12030
62. Beau I, Touraine P, Meduri G, et al. A novel phenotype related to partial loss of function mutations of the follicle stimulating hormone receptor. J Clin Invest. 1998; 102(7): 1352-1359. doi: 10.1172/JCI3795
63. Touraine P, Beau I, Gougeon A, et al. New natural inactivating mutations of the follicle-stimulating hormone receptor: Cor- relations between receptor function and phenotype. Mol Endo crinol. 1999; 13(11): 1844-1854. doi: 10.1210/mend.13.11.0370
64. Pakarainen T, Zhang FP, Nurmi L, Poutanen M, Huhtani- emi I. Knockout of luteinizing hormone receptor abolishes the effects of follicle-stimulating hormone on preovulatory matura- tion and ovulation of mouse graafian follicles. Mol Endocrinol. 2005; 19(10): 2591-2602. doi: 10.1210/me.2005-0075
65. De Baere E, Beysen D, Oley C, et al. FOXL2 and BPES: Mutational hotspots, phenotypic variability, and revision of the genotype-phenotype correlation. Am J Hum Genet. 2003; 72(2): 478-487. doi: 10.1086/346118
66. Mu W, Wen H, Li J, He F. Cloning and expression analy- sis of a HSP70 gene from Korean rockfish (Sebastes schlegeli). Fish Shellfish Immunol. 2013; 35(4): 1111-1121. doi: 10.1016/j. fsi.2013.07.022
67. Kohno S, Katsu Y, Urushitani H, Ohta Y, Iguchi T, Guillette LJ Jr. Potential contributions of heat shock proteins to tempera- ture-dependent sex determination in the American alligator. Sex Dev. 2010; 4(1-2): 73-87. doi: 10.1159/000260374
68. Kim H, Chun S, Gu BS, Ku SY, Kim SH, Kim JG. Rela- tionship between inhibin-α gene polymorphisms and premature ovarian failure in Korean women. Menopause. 2011; 18(11): 1232-1236. doi: 10.1097/gme.0b013e31821d6f7e
69. Chand AL, Harrison CA, Shelling AN. Inhibin and prema- ture ovarian failure. Hum Reprod Update. 2010; 16(1): 39-50. doi: 10.1093/humupd/dmp031
70. Rajkovic A, Pangas SA, Ballow D, Suzumori N, Matzuk MM. NOBOX deficiency disrupts early folliculogenesis and oocyte-specific gene expression. Science. 2004; 305(5687): 1157- 1159. doi: 10.1126/science.1099755
71. Qin Y, Shi Y, Zhao Y, Carson SA, Simpson JL, Chen ZJ. Mutation analysis of NOBOX homeodomain in Chinese women with premature ovarian failure. Fertil Steril. 2009; 91(4 Suppl): 1507-1509. doi: 10.1016/j.fertnstert.2008.08.020
72. Wang J, Wang B, Song J, et al. New candidate gene POU5F1 associated with premature ovarian failure in Chinese patients. Reprod Biomed Online. 2011; 22(3): 312-316. doi: 10.1016/j.rbmo.2010.11.008
73. Achermann JC, Ozisik G, Meeks JJ, Jameson JL. Perspective: Genetic causes of human reproductive diseases. J Clin Endocri- nol Metab. 2002, 87(6): 2447-2454. doi: 10.1210/jc.87.6.2447
74. La Marca A, Brozzetti A, Sighinolfi G, Marzotti S, Volpe A, Falorni A. Primary ovarian insufficiency: Autoimmune causes. Curr Opin Obstet Gynecol. 2010; 22(4): 277-282. doi: 10.1097/ GCO.0b013e32833b6c70
75. Silva CA, Yamakami LY, Aikawa NE, Araujo DB, Car- valho JF, Bonfá E. Autoimmune primary ovarian insufficiency. Autoimmun Rev. 2014; 13(4-5): 427-430. doi: 10.1016/j.aut- rev.2014.01.003
76. Tuohy VK, Altuntas CZ. Autoimmunity and premature ovar- ian failure. Curr Opin Obstet Gynecol. 2007; 19(4): 366-369. doi: 10.1097/GCO.0b013e328220e90c
77. Meskhi A, Seif MW. Premature ovarian failure. Curr Opin Obstet Gynecol. 2006; 18(4): 418-426.
78. Rebar RW. Premature ovarian failure. Obstet Gynecol. 2009; 113(6): 1355-1363. doi: 10.1097/AOG.0b013e3181a66843
79. Dragojević-Dikić S, Marisavljević D, Mitrović A, Dikić S, Jovanović T, Janković-Raznatović S. An immunological insight into premature ovarian failure (POF). Autoimmun Rev. 2010; 9(11): 771-774. doi: 10.1016/j.autrev.2010.06.008
80. Panay N, Kalu E. Management of premature ovarian failure. Best Pract Res Clin Obstet Gynaecol. 2009; 23(1): 129-140. doi: 10.1016/j.bpobgyn.2008.10.008
81. Asbagh FA, Ebrahimi M. A case report of spontaneous pregnancy during hormonal replacement therapy for premature ovarian failure. Iran J Reprod Med. 2011; 9(1): 47-49. Website. http://pubmedcentralcanada.ca/pmcc/articles/PMC4212146/. Accessed January 27, 2017.
82. Ebrahimi M, Asbagh FA. The role of autoimmunity in pre- mature ovarian failure. Iran J Reprod Med. 2015; 13(8): 461- 472.
83. Khole V. Does ovarian autoimmunity play a role in the pathophysiology of premature ovarian insufficiency? J Midlife Health. 2010; 1(1): 9-13. doi: 10.4103/0976-7800.66986
84. Forges T, Monnier-Barbarino P, Faure GC, Béné MC. Au- toimmunity and antigenic targets in ovarian pathology. Hum Reprod Update. 2004; 10(2): 163-175. doi: 10.1093/humupd/dmh014
85. Pires ES, Meherji PK, Vaidya RR, Parikh FR, Ghosalkar MN, Khole VV. Specific and sensitive immunoassays detect multiple anti-ovarian antibodies in women with infertility. J Histochem Cytochem. 2007; 55(12): 1181-1190. Website. http:// journals.sagepub.com/doi/abs/10.1369/jhc.7A7259.2007. Accessed January 27, 2017.
86. Poppe K, Glinoer D, Tournaye H, et al. Thyroid autoimmu- nity and female infertility. Verh K Acad Geneeskd Belg. 2006; 68(5-6): 357-377. Website. http://europepmc.org/abstract/med/17313094. Accessed January 27, 2017.
87. Shamilova NN, Marchenko LA, Dolgushina NV, Zaletaev DV, Sukhikh GT. The role of genetic and autoimmune factors in premature ovarian failure. J Assist Reprod Genet. 2013; 30(5): 617-622. doi: 10.1007/s10815-013-9974-4
88. Carsote M, Valea A. Premature ovarian failure of autoim- mune causes. J Gynecol Neonatal Biol. 2015; 1(1): 1-2. Website. http://www.ommegaonline.org/article-details/Premature- ovarian-failure-of-autoimmune-causes/364. Accessed January 27, 2017.
89. Carp HJ, Selmi C, Shoenfeld Y. The autoimmune bases of in- fertility and pregnancy loss. J Autoimmun. 2012; 38(2-3): J266- J274. doi: 10.1016/j.jaut.2011.11.016
90. Cervera R, Balasch J. Bidirectional effects on autoimmunity and reproduction. Hum Reprod Update. 2008; 14(4): 359-366. doi: 10.1093/humupd/dmn013
91. Monnier-Barbarino P, Forges T, Faure GC, Béné MC. Gonadal antibodies interfering with female reproduction. Best Pract Res Clin Endocrinol Metab. 2005; 19(1): 135-148. doi: 10.1016/j.beem.2004.11.011
92. Luborsky J, Pong R. Pregnancy outcome and ovarian anti- bodies in infertility patients undergoing controlled ovarian hyperstimulation. Am J Reprod Immunol. 2000; 44(5): 261-265. doi: 10.1111/j.8755-8920.2000.440502.x
93. Reato G, Morlin L, Chen S, et al. Premature ovarian failure in patients with autoimmune Addison’s disease: Clinical, genetic, and immunological evaluation. J Clin Endocrinol Metab. 2011; 96(8): E1255-E1261. doi: 10.1210/jc.2011-0414
94. Dal Pra C, Chen S, Furmaniak J, et al. Autoantibodies to steroidogenic enzymes in patients with premature ovarian failure with and without Addison’s disease. Eur J Endocrinol. 2003; 148(5): 565-570. doi: 10.1530/eje.0.1480565
95. Chiauzzi VA, Bussmann L, Calvo JC, Sundblad V, Charreau EH. Circulating immunoglobulins that inhibit the binding of follicle-stimulating hormone to its receptor: A putative diagnostic role in resistant ovary syndrome? Clin Endocrinol (Oxf). 2004; 61(1): 46-54. doi: 10.1111/j.1365-2265.2004.02054.x
96. Ryan MM, Jones HR Jr. Myasthenia gravis and premature ovarian failure. Muscle Nerve. 2004; 30(2): 231-233. doi: 10.1002/mus.20067
97. Gobert B, Jolivet-Reynaud C, Dalbon P, et al. An immuno- reactive peptide of the FSH involved in autoimmune infertility. Biochem Biophys Res Commun. 2001; 289(4): 819-824. doi: 10.1006/bbrc.2001.6059
98. Koyama K, Hasegawa A. Premature ovarian failure syn drome may be induced by autoimmune reactions to zona pellucid proteins. J Reprod Endocrinol. 2006; 3: 94-97. Website. http://www.kup.at/journals/abbildungen/gross/6633.html. Accessed January 27, 2017.
99. Luborsky JL, Visintin I, Boyers S, Asari T, Caldwell B, DeCherney A. Ovarian antibodies detected by immobilized an- tigen immunoassay in patients with premature ovarian failure. J Clin Endocrinol Metab. 1990; 70(1): 69-75. doi: 10.1210/jcem- 70-1-69
100. Pasoto SG, Viana VS, Mendonca BB, Yoshinari NH, Bonfa E. Anti-corpus luteum antibody: A novel serological marker for ovarian dysfunction in systemic lupus erythematosus? J Rheumatol. 1999; 26(5): 1087-1093. Website. http://europepmc.org/ abstract/med/10332973. Accessed January 27, 2017.
101. Falorni A, Laureti S, Candeloro P, et al. Steroid-cell autoan- tibodies are preferentially expressed in women with premature ovarian failure who have adrenal autoimmunity. Fertil Steril. 2002; 78(2): 270-279. doi: 10.1016/S0015-0282(02)03205-3
102. Welt CK. Autoimmune oophoritis in the adolescent. Ann N Y Acad Sci. 2008; 1135: 118-122. doi: 10.1196/annals.1429.006
103. Wémeau JL, Proust-Lemoine E, Ryndak A, Vanhove L. Thyroid autoimmunity and polyglandular endocrine syndromes. Hormones (Athens). 2013; 12(1): 39-45. Website. http://www. hormones.gr/pdf/HORMONES2013,39-45.pdf. Accessed January 27, 2017.
104. Abalovich M, Mitelberg L, Allami C, et al. Subclinical hypothyroidism and thyroid autoimmunity in women with infertility. Gynecol Endocrinol. 2007; 23(5): 279-283. doi: 10.1080/09513590701259542
105. Betterle C, Dal Pra C, Mantero F, Zanchetta R. Auto-immune adrenal insufficiency and autoimmune polyendocrine syndromes: Autoantibodies, autoantigens, and their applicability in diagnosis and disease prediction. Endocr Rev. 2002; 23(3): 327- 364. doi: 10.1210/edrv.23.3.0466
106. Euthymiopoulou K, Aletras AJ, Ravazoula P, et al. Anti- ovarian antibodies in primary Sjogren’s syndrome. Rheumatol Int. 2007; 27(12): 1149-1155. doi: 10.1007/s00296-007-0364-z
107. Sklar C. Maintenance of ovarian function and risk of pre- mature menopause related to cancer treatment. J Natl Cancer Inst Monogr. 2005; 34: 25-27. Website. http://citeseerx.ist.psu. edu/viewdoc/download?doi=10.1.1.589.3491&rep=rep1&type =pdf. Accessed January 27, 2017.
108. Rebar RW. Premature ovarian “failure” in the adolescent. Ann N Y Acad Sci. 2008; 1135: 138-145. doi: 10.1196/annals.1429.000
109. Wallace WHB, Thomson AB, Kelsey TW. The radiosensi- tivity of the human oocyte. Hum Reprod. 2003; 18(1): 117-121. doi: 10.1093/humrep/deg016
110. Ash P. The influence of radiation on fertility in man. Br J Radiol. 1980; 53(628): 271-278. doi: 10.1259/0007-1285-53- 628-271
111. Gracia CR, Sammel MD, Freeman E, et al. Impact of cancer therapies on ovarian reserve. Fertil Steril. 2012; 97(1): 134-140. doi: 10.1016/j.fertnstert.2011.10.040
112. Lie Fong S, Laven JS, Hakvoort-Cammel FG, et al. Assessment of ovarian reserve in adult childhood cancer survivors using anti-Müllerian hormone. Hum Reprod. 2009; 24(4): 982- 990. doi: 10.1093/humrep/den487
113. Oktem O, Oktay K. Quantitative assessment of the impact of chemotherapy on ovarian follicle reserve and stromal function. Cancer. 2007; 110(10): 2222-2229. doi: 10.1002/cncr.23071
114. Wallace WH. Oncofertility and preservation of reproductive capacity in children and young adults. Cancer. 2011; 117(10 Suppl): 2301-2310. doi: 10.1002/cncr.26045
115. Fenton A, Panay N. Does routine gynecological surgery contribute to an early menopause? Climacteric. 2012; 15(1): 1-2. doi: 10.3109/13697137.2012.647623
116. Kovacs P, Stangel JJ, Santoro NF, Lieman H. Successful pregnancy after transient ovarian failure following treatment of symptomatic leiomyomata. Fertil Steril. 2002; 77(6): 1292- 1295. doi: 10.1016/S0015-0282(02)03091-1
117. Conway GS. Premature ovarian failure. Br Med Bull. 2000; 56(3): 643-649. doi: 10.1258/0007142001903445
118. Longway M, Matthews CA. Resumption of ovarian function 20 years after chemotherapy-induced ovarian failure: A case report. Fertil Steril. 2009; 92(1): e17-e18. doi: 10.1016/j.fertnstert.2009.02.082
119. Wikström AM, Hovi L, Dunkel L, Saarinen-Pihkala UM. Restoration of ovarian function after chemotherapy for osteosarcoma. Arch Dis Child. 2003; 88(5): 428-431. doi: 10.1136/adc.88.5.428
120. Wang H, Chen H, Qin Y, et al. Risks associated with pre- mature ovarian failure in Han Chinese women. Reprod Biomed Online. 2015; 30(4): 401-407. doi: 10.1016/j.rbmo.2014.12.013
121. Ohl J, Partisani M, Demangeat C, Binder-Foucard F, Nisand I, Lang JM. [Alterations of ovarian reserve tests in Human Im- munodeficiency Virus (HIV)-infected women]. Gynecol Obstet Fertil. 2010; 38(5): 313-317. doi: 10.1016/j.gyobfe.2009.07.019
122. Chang SH, Kim CS, Lee KS, et al. Premenopausal factors influencing premature ovarian failure and early menopause. Maturitas. 2007; 58(1): 19-30. doi: 10.1016/j.maturitas.2007.04.001
123. Di Prospero F, Luzi S, Iacopini Z. Cigarette smoking dam- ages women’s, reproductive life. Reprod Biomed Online. 2004; 8(2): 246-247. doi: 10.1016/S1472-6483(10)60525-1
124. Panay N, Maclaran K, Nicopollous J, Horner E, Domoney C. Findings from the West London Menopause and PMS Centre POF Database. In: Proceedings of the 32nd British Belfast, Northern Ireland, UK: International congress of obstetrics and gynaecology; 2010: 20-23.
125. European Society for Human Reproduction and Embryol- ogy (ESHRE) Guideline Group on POI, Webber L, Davies M, et al. ESHRE Guideline: Management of women with premature ovarian insufficiency. Hum Reprod. 2016; 31(5): 926-937. doi: 10.1093/humrep/dew027
126. Davis SR, Jane F. Sex and perimenopause. Aust Fam Physician. 2011; 40(5): 274-278. Website. http://search.proquest. com/openview/ca481b530410c94899ccd04ec868a360/1?pq- origsite=gscholar&cbl=33668. Accessed January 27, 2017.
127. Smith JA, Vitale S, Reed GF, et al. Dry eye signs and symp- toms in women with premature ovarian failure. Arch Ophthal- mol. 2004; 122(2): 151-156. doi: 10.1001/archopht.122.2.151
128. Knauff EA, Eijkemans MJ, Lambalk CB, et al. Anti-Mulle- rian hormone, inhibin B, and antral follicle count in young women with ovarian failure. J Clin Endocrinol Metab. 2009; 94(3): 786-792. doi: 10.1210/jc.2008-1818
129. Kumar N, Singh AK. Role of Antimüllerian hormone in gy- necology: A review of literature. Int J Infertil Fetal Med. 2015; 6(2): 51-61. doi: 10.5005/jp-journals-10016-1102
130. Cate RL, Mattaliano RJ, Hession C, et al. Isolation of the bovine and human genes for Müllerian inhibiting substance and expression of the human gene in animal cells. Cell. 1986; 45(5): 685-698. doi: 10.1016/0092-8674(86)90783-X
131. Durlinger AL, Gruijters MJ, Kramer P, et al. Anti-Müllerian hormone inhibits initiation of primordial follicle growth in the mouse ovary. Endocrinology. 2002; 143(3): 1076-1084. doi: 10.1210/endo.143.3.8691
132. Durlinger AL, Kramer P, Karels B, et al. Control of primordial follicle recruitment by anti-Müllerian hormone in the mouse ovary. Endocrinology. 1999; 140(12): 5789-5796. doi: 10.1210/ endo.140.12.7204
133. Nardo LG, Christodoulou D, Gould D, Roberts SA, Fitzger- ald CT, Laing I. Anti-Müllerian hormone levels and antral follicle count in women enrolled in in-vitro fertilization cycles: Relationship to lifestyle factors, chronological age and reproductive history. Gynecol Endocrinol. 2007; 23(8): 486-493. doi: 10.1080/09513590701532815
134. van Disseldorp J, Lambalk CB, Kwee J, et al. Comparison of inter- and intra-cycle variability of anti-Mullerian hormone and antral follicle counts. Hum Reprod. 2010; 25(1): 221-227. doi: 10.1093/humrep/dep366
135. Laven JS, Mulders AG, Visser JA, Themmen AP, De Jong FH, Fauser BC. Anti-Müllerian hormone serum concentrations in normoovulatory and anovulatory women of reproductive age. J Clin Endocrinol Metab. 2004; 89(1): 318-323. doi: 10.1210/jc.2003-030932
136. Visser JA, Schipper I, Laven JS, Themmen AP. Anti-Mül- lerian hormone: An ovarian reserve marker in primary ovar- ian insufficiency. Nat Rev Endocrinol. 2012; 8(6): 331-41. doi: 10.1038/nrendo.2011.224
137. Nelson SM. Biomarkers of ovarian response: current and future applications. Fertil Steril. 2013; 99(4): 963-969. doi: 10.1016/j.fertnstert.2012.11.051
138. Committee opinion no. 605: Primary ovarian insufficiency in adolescents and young women. Obstet Gynecol. 2014; 124(1): 193-197. doi: 10.1097/01.aog.0000451757.51964.98
139. Halder A, Fauzdar A, Ghosh M, Kumar A. Serum inhibin B: A direct and precise marker of ovarian function. J Clin Diagn Res. 2007: 1: 131-137. Website. http://www.jcdr.net/back_is- sues.asp?issn=0973-709x&year=2007&month=June&vo- lume=1&issue=3&page=131-137&id=69. Accessed January 27, 2017.
140. De Caro JJ, Dominguez C, Sherman SL. Reproductive health of adolescent girls who carry the FMR1 premutation: Expected phenotype based on current knowledge of fragile X-associated primary ovarian insufficiency. Ann N Y Acad Sci. 2008; 1135: 99-111. doi: 10.1196/annals.1429.029
141. Ben-Nagi J, Panay N. Premature ovarian insufficiency: How to improve reproductive outcome? Climacteric. 2014; 17(3): 242-246. doi: 10.3109/13697137.2013.860115
142. Schmidt KT, Nyboe Andersen A, Greve T, Ernst E, Loft A, Yding Andersen C. Fertility in cancer patients after cryopreser- vation of one ovary. Reprod Biomed Online. 2013; 26(3): 272- 279. doi: 10.1016/j.rbmo.2012.12.001
143. Donnez J, Dolmans MM, Pellicer A, et al. Restoration of ovarian activity and pregnancy after transplantation of cryo- preserved ovarian tissue: A review of 60 cases of reimplantation. Fertil Steril. 2013; 99(6): 1503-1513. doi: 10.1016/j.fertn- stert.2013.03.030
144. Lutjen P, Trounson A, Leeton J, Findlay J, Wood C, Renou P. The establishment and maintenance of pregnancy using in vitro fertilization and embryo donation in a patient with primary ovarian failure. Nature. 1984; 307(5947): 174-175. doi: 10.1038/307174a0
145. Sirola J, Kröger H, Honkanen R, et al. Smoking may impair the bone protective effects of nutritional calcium: A population- based approach. J Bone Miner Res. 2003; 18(6): 1036-1042. doi: 10.1359/jbmr.2003.18.6.1036
146. Banks E, Reeves GK, Beral V,Balk will A,Liu B,Roddam A. Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: Prospective analysis. PLoS Med. 2009; 6(11): e1000181. doi: 10.1371/journal.pmed.1000181
147. Manolagas SC, O’Brien CA, Almeida M. The role of estrogen and androgen receptors in bone health and disease. Nat Rev Endocrinol. 2013; 9(12): 699-712. doi: 10.1038/nren-do.2013.179
148. Bachelot A, Rouxel A, Massin N, et al. POF-GIS Study Group. Phenotyping and genetic studies of 357 consecutive pa- tients presenting with premature ovarian failure. Eur J Endocri- nol. 2009; 161(1): 179-1487. doi: 10.1530/EJE-09-0231
149. Freriks K, Timmermans J, Beerendonk CC, et al. Standard- ized multidisciplinary evaluation yields significant previously undiagnosed morbidity in adult women with turner syndrome. J Clin Endocrinol Metab. 2011; 96(9): E1517-E1526. doi: 10.1210/jc.2011-0346
150. Popat VB, Calis KA, Vanderhoof VH, et al. Bone mineral density in estrogen-deficient young women. J Clin Endocrinol Metab. 2009; 94(7): 2277-2283. doi: 10.1210/jc.2008-1878
151. van der Schouw YT, van der Graaf Y, Steyerberg EW, Ei- jkemans JC, Banga JD. Age at menopause as a risk factor for cardiovascular mortality. Lancet. 1996; 347(9003): 714-718. doi: 10.1016/S0140-6736(96)90075-6
152. Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: A meta-analysis. Menopause. 2006; 13(2): 265-279. doi: 10.1097/01.gme.0000218683.97338.ea
153. Baba Y, Ishikawa S, Amagi Y, Kayaba K, Gotoh T, Kajii E. Premature menopause is associated with increased risk of ce- rebral infarction in Japanese women. Menopause. 2010; 17(3): 506-510. doi: 10.1097/gme.0b013e3181c7dd41
154. Gallagher LG, Davis LB, Ray RM, et al. Reproductive his- tory and mortality from cardiovascular disease among women textile workers in shanghai, china. Int J Epidemiol. 2011; 40(6):1510-1518. doi: 10.1093/ije/dyr134
155. Kalantaridou SN, Naka KK, Papanikolaou E, et al. Impaired endothelial function in young women with premature ovarian failure: normalization with hormone therapy. J Clin Endocrinol Metab. 2004; 89(8): 3907-3913. doi: 10.1210/jc.2004-0015
156. Clarkson TB. Estrogen effects on arteries vary with stage of reproductive life and extent of subclinical atherosclerosis pro- gression. Menopause. 2007; 14(3 Pt 1): 373-384. doi: 10.1097/ GME.0b013e31803c764d
157. RenJ,HintzKK,RougheadZK,etal.Impactofestro- gen replacement on ventricular myocyte contractile function and protein kinase B/Akt activation. Am J Physiol Heart Circ Physiol. 2003; 284(5): H1800-H1807. Website. https://pubag. nal.usda.gov/pubag/article.xhtml?id=46686. Accessed January 27, 2017.
158. Sumino H, Ichikawa S, Itoh H, et al. Hormone replacement therapy decreases insulin resistance and lipid metabolism in Japanese postmenopausal women with impaired and normal glucose tolerance. Horm Res. 2003; 60(3): 134-142. doi: 10.1159/000072525
159. Rocca WA, Shuster LT, Grossardt BR, et al. Long-term effects of bilateral oophorectomy on brain aging: Unanswered questions from the mayo clinic cohort study of oophorectomy and aging. Womens Health (Lond). 2009; 5(1): 39-48. doi: 10.2217/17455057.5.1.39
160. Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: Long- term health consequences. Maturitas. 2010; 65(2): 161. doi: 10.1016/j.maturitas.2009.08.003
161. King RB. Subfecundity and anxiety in a nationally rep-resentative sample. Soc Sci Med. 2003; 56(4): 739-751. doi: 10.1016/S0277-9536(02)00069-2
162. Slade P, Emery J, Lieberman BA. A prospective, longitudinal study of emotions and relationships in in-vitro fertilization treatment. Hum Reprod. 1997; 12(1): 183-190. doi: 10.1093/humrep/12.1.183
163. Graziottin A, Basson R. Sexual dysfunction in women with premature menopause. Menopause. 2004; 11(6 Pt 2): 766-777. doi: 10.1097/01.gme.0000139926.02689.a1
164. NIH State-of-the-Science Conference Statement on management of menopause-related symptoms. NIH Consens State Sci Statements. 2005; 22(1): 1-38.
165. Nicholas CR, Haston KM, Grewall AK, Longacre TA, Reijo Pera RA. Transplantation directs oocyte maturation from embryonic stem cells and provides a therapeutic strategy for fe- male infertility. Hum Mol Genet. 2009; 18(22): 4376-4389. doi: 10.1093/hmg/ddp393
166. Dan S, Haibo L, Hong L. Pathogenesis and stem cell ther- apy for premature ovarian failure. OA Stem Cells. 2014; 2(1): 4. Website. http://ifctp.org/download/Embryonic%20Stem%20 Cells/ESC%20for%20Fertility/Pathogenesis%20and%20 stem%20cell%20therapy%20for%20premature%20ovarian.pdf. Accessed January 27, 2017.
167. Hayashi K, Saitou M. Generation of eggs from mouse embryonic stem cells and induced pluripotent stem cells. Nat Pro toc. 2013; 8(8): 1513-1524. doi: 10.1038/nprot.2013.090
168. Kilic S, Pinarli F, Ozogul C, Tasdemir N, Naz Sarac G, Delibasi T. Protection from cyclophosphamide-induced ovar- ian damage with bone marrow-derived mesenchymal stem cells during puberty. Gynecol Endocrinol. 2014; 30(2): 135-140. doi: 10.3109/09513590.2013.860127
169. Tipnis S, Viswanathan C, Majumdar AS. Immunosuppressive properties of human umbilical cord-derived mesenchymal stem cells: Role of B7-H1 and IDO. Immunol Cell Biol. 2010; 88(8): 795-806. doi: 10.1038/icb.2010.47
170. Varma MJ, Breuls RG, Schouten TE, et al. Phenotypical and functional characterization of freshly isolated adipose tissue-derived stem cells. Stem Cells Dev. 2007; 16(1): 91-104. doi: 10.1089/scd.2006.0026
171. Lee HJ, Selesniemi K, Niikura Y, et al. Bone marrow trans- plantation generates immature oocytes and rescues long-term fertility in a preclinical mouse model of chemotherapy-induced premature ovarian failure. J Clin Oncol. 2007; 25(22): 3198- 3204. doi: 10.1200/JCO.2006.10.3028
172. White YA, Woods DC, Takai Y, Ishihara O, Seki H, Tilly JL. Oocyte formation by mitotically active germ cells purified from ovaries of reproductive-age women. Nat Med. 2012; 18(3): 413-421. doi: 10.1038/nm.2669