INTRODUCTION
Post-pancreatectomy hemorrhage is a frequent adverse event with high morbidity and mortality (3-60%).1 Most bleeding originated from gastro-duodenal artery stump (29%).1,2
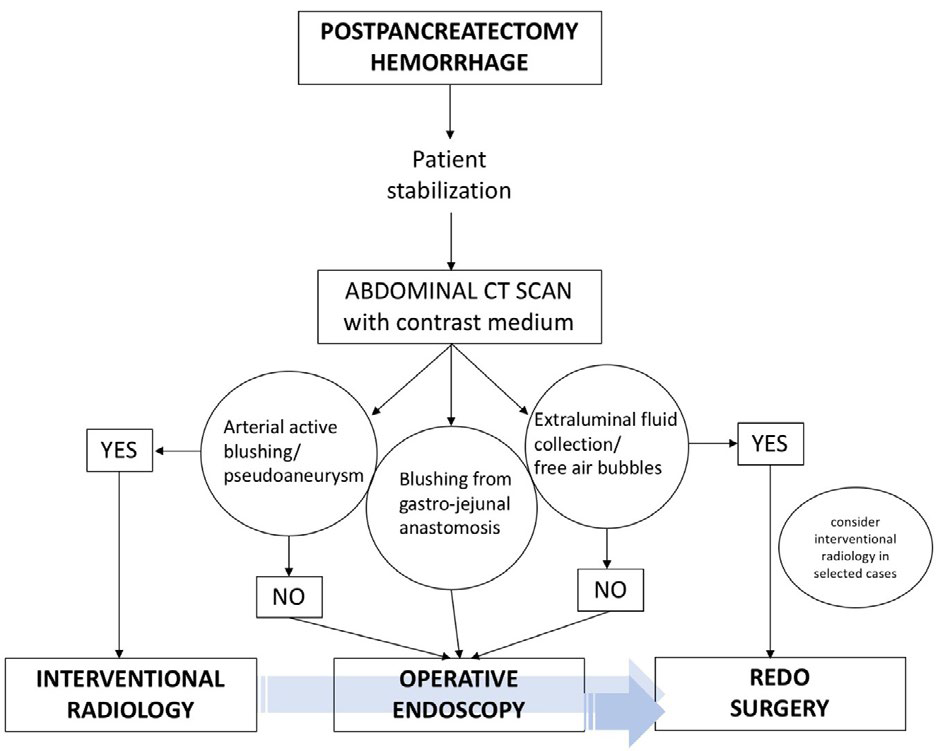
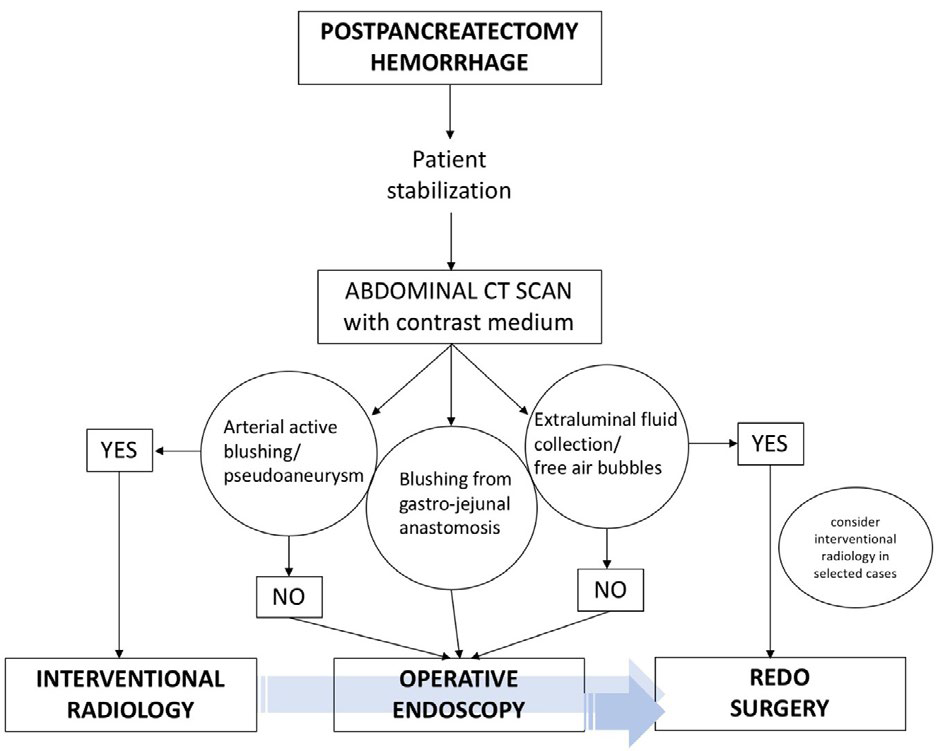
Multidisciplinary approach is involved in the management of this complication including redo surgery, interventional radiology and operative endoscopy.1,2,3
It is crucial to consider that this adverse event can be associated with partial/complete dehiscence of pancreatico-jejunal anastomosis as cause or consequence of bleeding (because it can lead pancreatic juice to damage surrounding vessels or consequence as a result the blood can overtend the bilio-pancreatic jejunal loop).
Assuming that, abdominal computerized tomography (CT) scan is mandatory prior to every kind of treatment to assess the integrity of the anastomoses, eventual active blushing and/or emoperitoneum.4 Mean sensitivity was assessed at 56-67%.2
If it is true that endoscopy can be both diagnostic and therapeutic in more and more surgical complications, it should be avoided to manage bleeding in this setting if any sign of anastomotic dehiscence is present. In this case, the most common cause of bleeding is extraluminal bleeding and endoscopy can only worsen the situation by CO2 /air inflation, washing and pushing the instruments. Moreover, the entity of bleeding does not lead to add any even diagnostic information on the source.
Considering the literature, hemorrhage source was not found in 31% patients during endoscopy.4
Operative endoscopy can play an efficient role in case of bleeding from the gastro-jejunal anastomosis and can diagnose if the bleeding comes from the gastro-jejunal anastomosis or from the bilio-pancreatic jejunal loop. However, literature data reported a 48% success rate and 24% mortality.2
On the other hand, endoscopy seems to be more effective in delayed bleeding with a source control success in 85.7% of cases.5
The role of interventional radiology should be taken in consistent account especially if active blushing is seen at the previous abdominal CT scan.6 According to the available literature, it can be considered the mininvasive treatment of choice in this case. If it fails, considering endoscopy a valid alternative can be a huge mistake in terms of clinical outcomes and timing to redo-surgery. We cannot consider the two methods-endoscopy and radiology inter-schangeable for post-pancreatectomy bleeding because several hemorrages cannot be managed by endoscopy in this cluster of patients.
Redo surgery has still a major role for this complication despite of its high morbidity and mortality, acceptable if we consider the low percentage of recurrences.2,3,4 Furthermore, surgery should be considered as rescue therapy in case of endoscopic or radiological failure and in not hemodynamically stable patients (Figure 1).1
Figure 1. Flowchart Showing the Multidisciplinary Management for Post-pancreatectomy Hemorrhage
CONCLUSION
In conclusion, as resumed in our flowchart, post-pancreatectomy hemorrhage requires efficient and rapid treatments. Preliminary abdominal CT scan is mandatory to guide the correct management; interventional radiology must be considered the most efficient mininvasive treatment; redo surgery has still the main role to save patients’ lives; endoscopy has a diagnostic role and can be reserved to treat the bleeding from gastro-jejunal anastomosis and has only a minor role in other kinds of hemorrhage, only if there are nor extraluminal blood collection not arterial active bleeding from pancreatico-jejunal anastomosis.