1. Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO classification of tumours of the urinary system and male genital organs-part B: Prostate and bladder tumours. Eur Urol. 2016; 70: 106-119, doi: 10.1016/j.eururo.2016.02.028
2. Samaratunga H, Delahunt B. Recently described and unusual variants of urothelial carcinoma of the urinary bladder. Pathology. 2012; 44: 407-418, doi: 10.1097/PAT.0b013e3283560172
3. Lopez-Beltran A, Eble JN, Bostwick D. G. Pleomorphic giant cell carcinoma of the prostate. Arch Pathol Lab Med. 2005; 129(5): 683-685. doi: 10.1043/1543-2165(2005)1292.0.CO;2
4. Kir G, Seneldi, H, Topal CS, Tosun M. Pleomorphic giant cell carcinoma of the prostate: A case report. Virchows Arch. 2015; 467: S277-S277.
5. Parwani AV, Herawi M, Epstein JI. Pleomorphic giant cell adenocarcinoma of the prostate: report of 6 cases. Am J Surg Pathol. 2006; 30: 1254-1259. doi: 10.1097/01.pas.0000209841.77595.4b
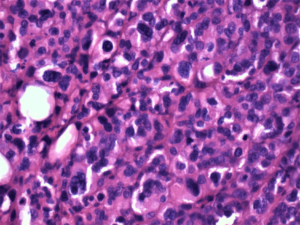
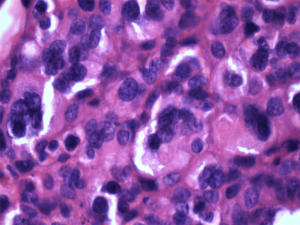
6. Samaratunga H, Delahunt B, Egevad L, Adamson M, Hussey D, Malone G, et al. Pleomorphic giant cell carcinoma of the urinary bladder: An extreme form of tumour de-differentiation. Histopathology. 2016; 68: 533-540. doi: 10.1111/his.12785
7. Akkaya H, Ipekci T, Hoscan MB, Ozdemir H. Pleomorphic giant cell carcinoma of the urinary bladder: Report of two cases. Virchows Arch. 2015; 467: S263-S264.
8. Alexiev BA, Papadimitriou JC, Chai TC, Ramos E, Staats PN, Drachenberg CB, et al. Polyomavirus (BK)-associated pleomorphic giant cell carcinoma of the urinary bladder: A case report. Pathol Res Pract. 2013; 209: 255259. doi: 10.1016/j.prp.2013.01.008
9. Barresi V. HOXB13 is not expressed in pleomorphic giant cell carcinoma of the bladder. Virchows Arch. 2018; 473: 259-260. doi: 10.1007/s00428-018-2394-1
10. Lopez-Beltran A, Blanca A, Montironi R, Cheng L, López JCR. Pleomorphic giant cell carcinoma of the urinary bladder. Human Pathology. 2009; 40: 1461-1466. doi: 10.1016/j.humpath.2009.02.016
11. Amin MB. Histological variants of urothelial carcinoma: diagnostic, therapeutic and prognostic implications. Modern Pathology. 2009; 22: S96. doi: 10.1038/modpathol.2009.26
12. Lopez-Beltran A, Cheng L, Comperat E, Rouprêt M, Blanca A, Menendez CL, et al. Large cell undifferentiated carcinoma of the urinary bladder. Pathology. 2010; 42: 364-368. doi: 10.3109/00313021003767363
13. Lopez-Beltran A, Requena MJ, Cheng L, Montironi R. Pathological variants of invasive bladder cancer according to their suggested clinical significance. B J U Int. 2008; 101: 275-281. doi: 10.1111/j.1464-410X.2007.07271.x
14. Mahmoud-Ahmed AS, Suh JH, Kupelian PA, Klein EA, Peereboom DM, Dreicer R, et al. Brain metastases from bladder carcinoma: Presentation, treatment and survival. J Urol. 2002; 167: 2419-2422. doi: 10.1016/S0022-5347(05)64996-8
15. Chung JH, Lee JY, Pyo JY, Oh YH, Lee SW, Moon HS, et al. Brain and skin metastasis from urothelial carcinoma of the bladder. Korean J Urol. 2013; 54: 66-68. doi: 10.4111/kju.2013.54.1.66
16. Sarmiento JM, Wi MS, Piao Z, Stiner ES. Solitary cerebral metastasis from transitional cell carcinoma after a 14-year remission of urinary bladder cancer treated with gemcitabine: Case report and literature review. Surg Neurol Int. 2012; 3: 82. doi: 10.4103/2152-7806.99172
17. Vaa B, Kohli M, Price KA, Swetz KM. Solitary cystic cerebellar metastasis in a patient with invasive transitional cell carcinoma of the bladder. BMJ Case Reports. 2014; 2014: bcr2013200137. doi: 10.1136/bcr-2013-200137
18. Anderson RS, el-Mahdi AM, Kuban DA, Higgins EM. Brain metastases from transitional cell carcinoma of urinary bladder. Urology. 1992; 39: 17-20. doi: 10.1016/0090-4295(92)90034-t
19. Johnson JD, Young, B. Demographics of brain metastasis. Neurosurg Clin N Am. 1996; 7: 337-344. doi: 10.1016/S1042- 3680(18)30365-6
20. Yang G, Wang Y, Wang Y, Lin S, Sun D. CyberKnife therapy of 24 multiple brain metastases from lung cancer: A case report. Oncol Lett. 20132; 6: 534-536. doi: 10.3892/ol.2013.1383
21. Shinagare AB, Ramaiya NH, Jagannathan JP, Fennessy FM, Taplin M-E, Van den Abbeele AD. Metastatic pattern of bladder cancer: correlation with the characteristics of the primary tumor. AJR Am J Roentgenol. 2011; 196: 117-122. doi: 10.2214/AJR.10.5036
22. Bamias A, Tiliakos I, Karali MD, Dimopoulos MA. Systemic chemotherapy in inoperable or metastatic bladder cancer. Ann Oncol. 2006; 17: 553-561. doi: 10.1093/annonc/mdj079
23. Bellmunt J, de Wit R, Vaughn DJ, Fradet Y, Lee J-L, Fong L, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017; 376: 1015-1026. doi: 10.1056/NEJMoa1613683
24. Winters BR, Wright JL, Holt SK, Dash A, Gore JL, Schade GR. Health related quality of life following radical cystectomy: Comparative analysis from the medicare health outcomes survey. J Urolo. 2018; 199: 669-675. doi: 10.1016/j.juro.2017.08.111
25. Samaratunga H. Pleomorphic giant cell carcinoma of the urinary bladder: A clinicopathological analysis of 13 cases. Mod Pathol. 2015; 28: 255A-256A.