1. Honda K, Saraya T, Tamura M, Yokoyama T, Fujiwara M, Goto H. Tumor lysis syndrome and acquired ichthyosis occurring after chemotherapy for lung adenocarcinoma. J Clin Oncol. 2011; 29(35): e859-e860. doi: 10.1200/jco.2011.36.8175
2. Saraya T, Shimura C, Mikura S, et al. Huge mediastinal mass with SVC syndrome accompanying numerous chest wall collateral vessels. Intern Med. 2008; 47(19): 1719-1722. doi: 10.2169/internalmedicine.47.1076
3. Saraya T, Takata S, Fujiwara M. The role of vital signs in predicting cardiac tamponade in asymptomatic patients with malignancy-associated pericardial effusion. Pulm Res Respir Med Open J. 2016; SE(1): S3-S7. doi: 10.17140/PRRMOJ-SE-1-102
4. Nakajima A, Saraya T, Takata S, et al. The saw-tooth sign as a clinical clue for intrathoracic central airway obstruction. BMC Res Notes. 2012; 5: 388. doi: 10.1186/1756-0500-5-388
5. Hirukawa I, Saraya T, Wada S, Takizawa H. Marked enlargement of liver over a short period of time illustration. Pulm Res Respir Med Open J. 2016; 3(1): 1. doi: 10.17140/PRRMOJ-3-123
6. Tamura M, Saraya T, Fujiwara M, et al. High-resolution computed tomography findings for patients with drug-induced pulmonary toxicity, with special reference to hypersensitivity pneumonitis-like patterns in gemcitabine-induced cases. Oncologist. 2013; 18(4): 454-459. doi: 10.1634/theoncologist.2012-0248
7. Koide T, Saraya T, Nakamoto K, et al. A case of imatinib mesylate-induced pneumonitis based on the detection of epithelioid granulomas by video-assisted thoracoscopic surgery biopsy in a patient with chronic myeloid leukemia. Nihon Kokyuki Gakkai Zasshi. 2011; 49(6): 465-471.
8. Yao X, Panichpisal K, Kurtzman N, Nugent K. Cisplatin nephrotoxicity: A review. Am J Med Sci. 2007; 334(2): 115-124. doi: 10.1097/MAJ.0b013e31812dfe1e
9. Toriumi S, Sara-ya T, Tsujimoto N. Renal salt wasting syndrome due to carboplatin in a patient with lung cancer. Pulm Res Respir Med Open J. 2014; 1(1): 9-12. doi: 10.17140/PRRMOJ-1-102
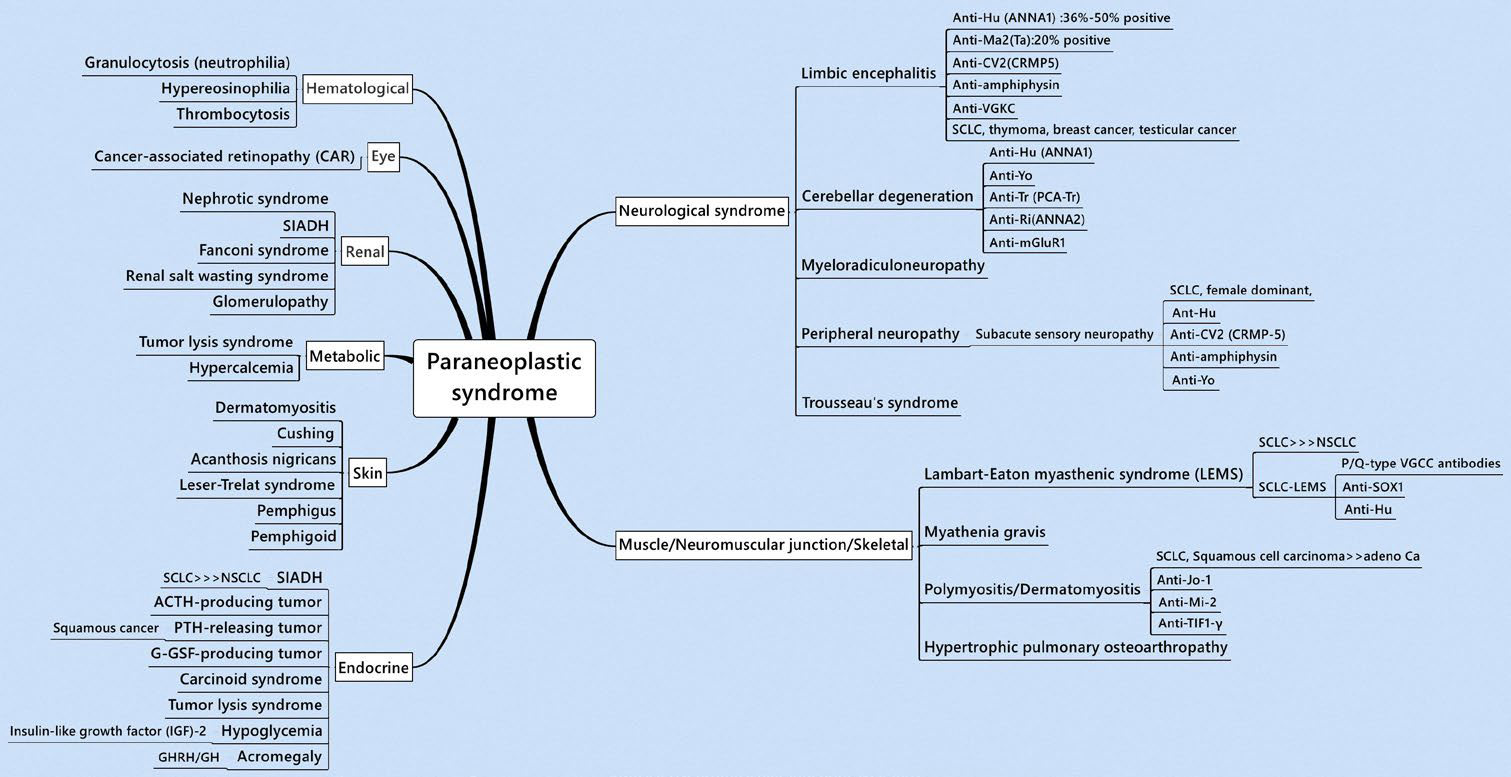
10. Graus F, Dalmau J. Paraneoplastic neurological syndromes. Curr Opin Neurol. 2012; 25(6): 795-801. doi: 10.1186/1750-1172- 2-22
11. Higaki M, Kurai D, Ito A, Saraya T. Evidence for hypohydrosis as clinical clue to diagnosis of Horner’s syndrome. BMJ Case Rep. 2013; 2013. doi: 10.1136/bcr-2013-009732
12. Nishizawa T, Saraya T, Kurai D, et al. Good syndrome occurred in a patient a prolonged time after thymectomy: A case report and literature review of cases in Japan. Journal of General and Family Medicine. 2016; 17(3): 238-243. doi: 10.14442/jgfm.17.3_238
13. Sakamori Y, Kim YH, Okuda C, et al. Two cases of cancer-associated retinopathy combined with small-cell lung cancer. Jpn J Clin Oncol. 2011; 41(5): 669-673. doi: 10.1093/jjco/hyr025
14. Bacchetta J, Juillard L, Cochat P, Droz JP. Paraneoplastic glomerular diseases and malignancies. Crit Rev Oncol Hematol. 2009; 70(1): 39-58. doi: 10.1016/j.critrevonc.2008.08.003
15. Owen CE. Cutaneous manifestations of lung cancer. Semin Oncol. 2016; 43(3): 366-369. doi: 10.1053/j.seminoncol.2016.02.025
16. Higaki M, Ishida M, Nakamoto Y, Saraya T. Horner’s syndrome with a sensation of warmth due to hypohidrosis. Intern Med. 2013; 52(15): 1757-1758. doi: 10.2169/internalmedicine.52.0660
17. Kanaji N, Watanabe N, Kita N, et al. Paraneoplastic syndromes associated with lung cancer. World J Clin Oncol. 2014; 5(3): 197-223. doi: 10.5306/wjco.v5.i3.197
18. Saraya T, Fujiwara M, Shimura C, Goto H. Not paraneoplastic pemphigus but pemphigus vulgaris in a patient with thymoma. BMJ Case Rep. 2015; 2015. doi: 10.1136/bcr-2015-210433
19. Spiro SG, Gould MK, Colice GL, American College of Chest P. Initial evaluation of the patient with lung cancer: Symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd ed). Chest. 2007; 132(Suppl 3): 149S-160S. doi: 10.1378/chest.07-1358
20. Lancaster E, Dalmau J. Neuronal autoantigens–pathogenesis, associated disorders and antibody testing. Nat Rev Neurol. 2012; 8(7): 380390. doi: 10.1038/nrneurol.2012.99
21. Ost DE, Jim Yeung SC, Tanoue LT, Gould MK. Clinical and organizational factors in the initial evaluation of patients with lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(Suppl 5): e121S-e41S. doi: 10.1378/chest.12-2352