INTRODUCTION
Practically, every old simple goiter changes into multi-nodular goiter.1 Extreme thyroid enlargement is mainly produced by multi-nodular goiter and is more commonly mistaken for tumor than any other variety of thyroids illness. Neoplastic alteration may occur in these hyperplastic places which are very tiny and can be missed by pathologists in slides stained with routine methods.2
The incidence of thyroid carcinoma has increased in recent years due to improvement in diagnostic techniques, e.g. an increase in fine needle aspiration cytology (FNAC) and radiology procedures like ultrasound, computed tomography (CT)-scan and magnetic resonance imaging (MRI).1 The thyroid cancer in Pakistan is accountable for 1.2% cases of all cancers.3,4 Earlier information from Pakistan showed PTC to comprise 57-89% of all thyroid malignancies.3,4 Unfortunately, recent data for thyroid malignancies papillary microcarcinoma of thyroid (PMCT) in Pakistan is not available, but most probably the small tumors might have been picked up incidentally in employment health screening or using imaging studies for other medical conditions. Unlike western world the healthcare system in Pakistan does not have a proper thyroid screening program.5,6,7 PMCT is considered to be the most common type of papillary carcinoma in the USA.1,2 The PMCT is defined as a tumor one (1) cm or less, that is generally found incidentally on histopathologic examination after thyroidectomy.8 It is basically discovered by vigilant assessment of removed thyroid specimens.1 The identification of PMCT in thyroid surgical pathology specimens ranges from 1-24% in one series and in 6-36% of autopsy specimens in another study.9,10 PMCT is increasing in all age groups and in the United States it is more common after 45-years.11 This change linking age and frequency have vital prognostic and management options.11
MATERIALS AND METHODS
It is a prospective cross-sectional study carried out in the Histopathology Section of Pathology Laboratory, PMC Peshawar, Pakistan. The demographic details of patients were recorded on a predesigned proforma. Most of the cases belonged to Peshawar, NW Tribal region, and refugee from Afghanistan, mostly these people are affected from bomb blasting and mining, they belong to mountain regions where iodine deficiency is common.12 The specimens were fixed in 10% buffered formalin immediately after thyroidectomy procedure. Sampling technique used was a consecutive convenient method. The duration of the study was from June 2018 to May 2019. All microscopically suspicious areas for PMCT in thyroidectomy specimens received in PMC histopathology laboratory were considered for the study. Ethical approval to conduct the study was obtained from the Board of Advanced Studies and Research (BASR), Riphah International University Islamabad in its 25th Meeting held on 18th October 2018.
Inclusion Criteria
Microscopically suspicious areas for PMCT in thyroidectomy specimen received in PMC Histopathology Laboratory, Varanasi, Uttar Pradesh.
Exclusion Criteria
1. Tru-Cut biopsies.
2. Fine needle aspiration cytology (FNAC) specimens of thyroid.
Recording Data
The observation and results were also recorded in tabulated form to compare percentage of different variables.
Data Analysis
Statistical analysis was performed using the statistical package for social sciences (SPSS) version 22 statistical program. Statistical results are given as mean and standard deviation for continuous variables. Difference between positive and negative status was analyzed for statistical significance by using Fisher’s exact test. Fisher’s exact test is applied where cells have 5 or less counts.13,14,15 Probability value p≤0.05 are considered statistically significant (Tables 1 to 4).
| Table 1. Age Groups |
|
S. No
|
Age Group
|
Frequency
(n=number)
|
Percentage (%)
|
|
1
|
1-20
|
3
|
9.37
|
|
2
|
21-40
|
18
|
56.2
|
|
3
|
41-60
|
9
|
28.12
|
|
4
|
>61
|
2
|
6.25
|
|
Total
|
32
|
100
|
| Above table shows age group distribution in which in the group two and three maximum numbers of specimen recived in our setup. |
| Table 2. Histopathological Diagnosis |
|
Histopathological Diagnosis
|
Frequency
(n=number)
|
Percentage
(%)
|
|
MNG
|
28
|
87.5
|
|
PMCT
|
2
|
6.25
|
|
PTC
|
1
|
3.12
|
|
FA
|
1
|
3.12
|
| Total |
32
|
100
|
| Table 3. Relationship of Age Group with Histopathological Diagnosis |
|
Age Group (Years)
|
Histopathological Diagnosis
|
Frequency (N)
|
Percentage (%)
|
|
1-20
|
MNG
|
2
|
6.25
|
|
FA
|
1
|
3.125
|
|
21-40
|
MNG
|
16
|
50.00
|
|
PMCT
|
1
|
3.125
|
|
41-60
|
MNG
|
8
|
25.00
|
|
PTC
|
1
|
3.125
|
|
PMCT
|
1
|
3.125
|
| Total |
|
32
|
100
|
| Above table shows both PMCT in different age group. |
| Table 4. The Specimen Weight Group was also Crosses Tabbed after Stratification and Results are shown in Table |
|
Specimen Weight Group
|
Specimen Type
|
Frequency (N)
|
Percentage (%)
|
|
0-50
|
MNG
|
2
|
66.7
|
|
PMCT
|
1
|
33.3
|
|
Total
|
3
|
100
|
|
51-100
|
MNG
|
11
|
84.6
|
|
PMCT
|
1
|
7.7
|
|
FA
|
1
|
7.7
|
|
Total
|
13
|
100
|
|
101-150
|
MNG
|
5
|
83.3
|
|
PTC
|
1
|
16.7
|
|
Total
|
6
|
100
|
|
151-200
|
MNG
|
4
|
100
|
|
>201
|
MNG
|
6
|
100
|
| Above table shows both PMCT in MNG specimens in both were smaller MNG accordingly |
Age group: The patients were divided into following age groups:
• 1-20-years
• 21-40-years
• 41-60-years
• 61-years and above
RESULTS
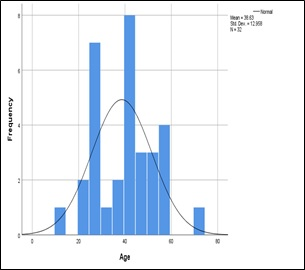
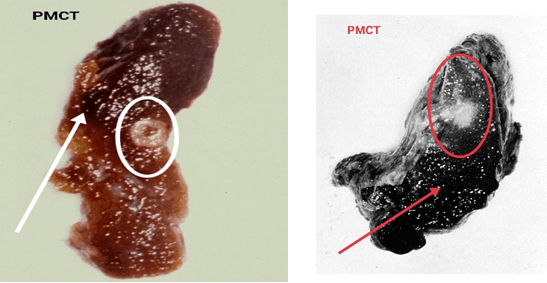
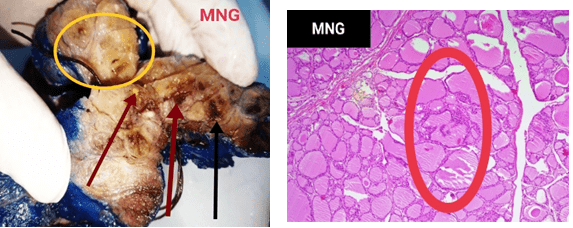
A total number of 72 total/subtotal thyroidectomy specimens were received in the Histopathology Department of PMC, Pakistan from June 2018 to May 2019. Out of these, 32 specimens showing suspicious foci for malignancy on gross/microscopic examination were selected for this study. Results shows maximum numbers MNG in younger population of KP. Both PMCT in different age group in both were in smaller multinodular goiter (MNG) specimens. The mean age in this study was 38.63±12.95-years (Figures 1 to 6).
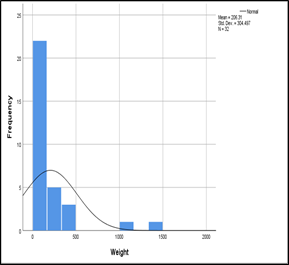
Figure 1. Specimen Weight Distributions
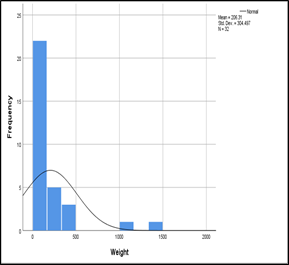
Figure 2. Age Distribution (Histogram)
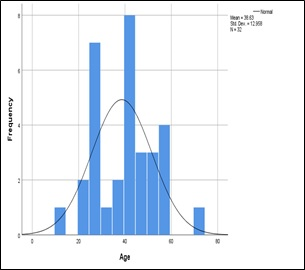
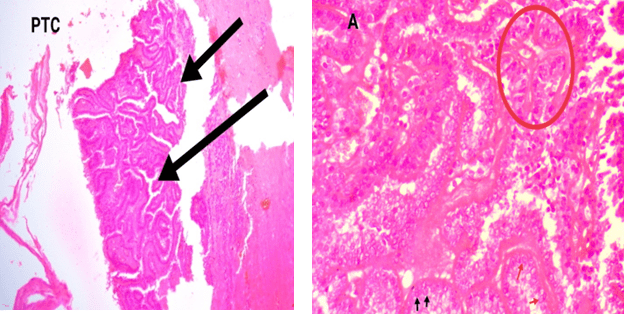
Figure 3. Histology Microscopically PTC Comprised of Papillae Lined by Neoplastic Follicular Epithelium. The Lining
Epithelium Showed Nuclear Atypia, Overlapping, Inclusions and Clear Nuclei (figure-PTC). Figure-A shows
Papillae Encircle (red Arrow) Nuclear Clearing (black arrow) and Chromatin
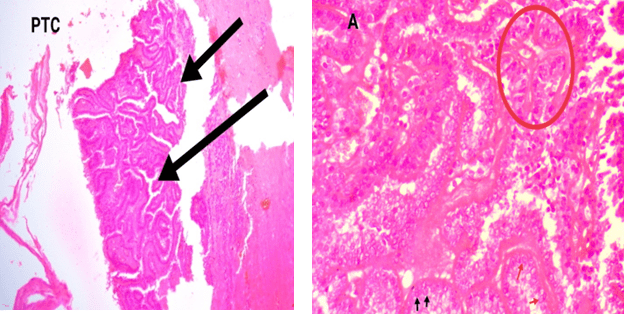
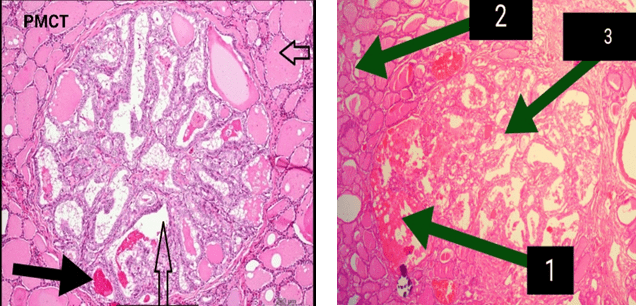
Figure 4. Psammoma Bodies could also be seen Arrow Shows Papillae Surrounded by Normal
Thyroid Tissue. Arrow 1 shows Focal Hemorrhages Arrow 2 Normal Throid Tissue and Arrow 3 Papillae
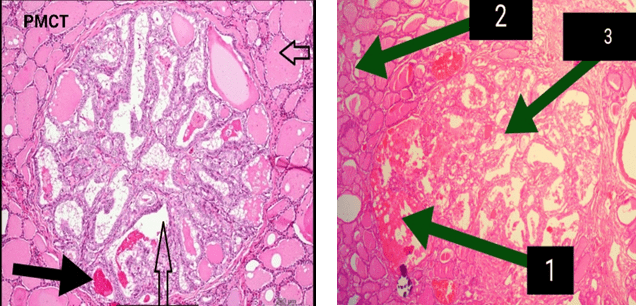
Figure 5. Grossly the Cut Surface of PMCT Showed Firmed White Lesion (encircled) in the Center
Cleaerly Cercumbscribed, and Foci of Hemorrhage (arrow), Fibrosis. No Invasion of the Capsule
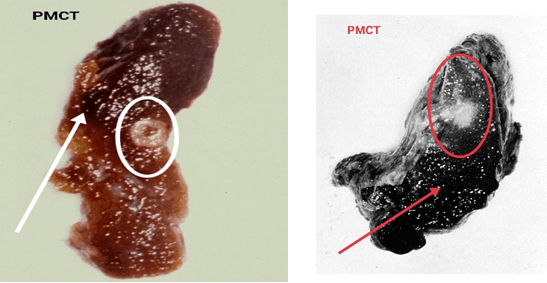
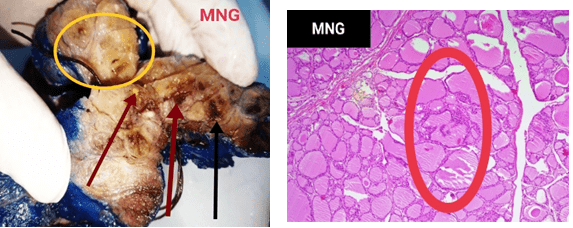
Figure 6. MNG Gross Grossly MNG had a Lobulated Appearance with a Variegated Cut Surface Showing Colloid
Nodules, Cysts and Fibrosis Along with Areas of Hemorrhages (arrow) and Foci of Calcification
DISSCUSSION
Multinodular goitre is an important thyroid dysfunction disorder which is related to hormonal imbalance. It is among the most common endocrine disorders which affects more than half a billion people. This disorder is said to be endemic if it affects more than 10% of a given population in an area. For non-endemic areas the annual incidence is almost 0.1% to 1.5% while prevalence remains to be 4-6%. Elderly females are said to have more cases of MNG thanmales. For endemic goiter, nodules appear early. But for sporadic forms, it appears later in life and the subjects may be unaware of it until late 50s.16 The nodular goiter, particularly multiple nodules involve a sound knowledge for diagnosis. The process involves a good physiological and medical knowledge with anatomical expertise for better surgical excisions considering pathological aspects in mind.17
Our study included MNG 28 (87.5%) cases followed by PMCT 2 (6.25%), papillary thyroid carcinoma (PTC) 1 and (3.12) follicular adenoma 1(3.12%). The results show a predominance of female patients in surgically resected MNGs with a relatively low incidence of neoplastic transformation.18 Our study reported two cases of PMCT and both were from different age groups, one was below 25-years and the other was 48-years.18 Mostly these carcinomas are considered as tumors of old age with a maximum being reported after 50-years. The results of our study are similar to what has been reported worldwide. A study with a considerable number of cases recorded that 65% of PMCT cases presented after the age of 45-years, while the rest i.e., 35% were below this age.9
One of the studies conducted at the National Cancer Institute (USA) evaluated 68,603 cases of PTC in a time period between 1973 and 2006 revealed that the incidence of PTC increased disproportionately in patients older than 45-years.11 The number of PMCT also increased in all age groups and is most common among patients older than 45-years (43%).11 Another study from Finland found the prevalence of PMT as 35.6% among 101 consecutive autopsies performed.19 However, other autopsy studies reported prevalence as low as 1% in a series of 300 autopsies performed.7,20 There are many autopsy series in the literature reporting PMT prevalence in between these two figures.21,22 This variation in the reported numbers of PMCT is probably in part due to different methods, histopathological criterias used in diagnosis and geographic factors. Incidental foci of PMCT found in a large percentage of patients after thyroidectomy for presumably benign thyroid conditions range from 2-24%.23 Our study also has similar prevalence as these studies (6.4%).
Weight of the excised specimen holds much greater importance in the diagnosis of the disease. It has been observed that increase in weight of the excised specimen is directly proportional to the chances of development of malignancies. This study has a high mean of 206.31±304.497 grams which is due to many outliers in the weight of the sample as shown in Figure 1. Because of these outliers it has now become difficult to correlate weight of specimens excised with neoplasms; however, generally it has been observed that heavy weight exhibits much more chances of thyroid malignancy. In a five-year study conducted at Spain on samples of 301 patients it was shown that the regression coefficient was (β=1.02), showing a direct correlation of weight with malignancies of the thyroid.24 A study from Greece for a period of 10-years where 2043 cases underwent thyroid surgeries evaluated the relationship of specimen weight with malignancy, the authors observed an Odds Ratio of 1.6, which means that the odds of complications are six times higher in patients having higher specimen weight.14,15 In both the studies the mean of the specimen weight were less than reported by this study which is due to few very heavy specimens excised in this study, where one specimen reached 1500 grams. All such samples have disturbed the overall mean of the specimen weight. Majority of the samples were in the range of 51-100 grams and both the compared studies have the means of specimen weight in the same range.
Papillary microcarcinoma of thyroid are usually found in small nodules and the tiny suspicious areas can be missed easily during gross examination. Worldwide studies have shown that many PMCTs occur in small nodules which can be potentially malignant. The same was observed in this study where both the cases of PMCT were in small nodules as compared to larger benign goiter. A study evaluating 900 cases of thyroidectomy specimens showed that maximum cases of PMCTs were found in smaller nodules as compared to PTC, which is similar to the results of our study.15
CONCLUSION
In thyroid excisions the weight of the excised specimen holds much great importance in determination/diagnosis of the disease. The risk of malignancy is higher in MNG compare to solitary nodules. The prevalence of PMCT are higher in smaller nodules is compare to PTC. Furthermore, the fact that our both PMCTs occurred in total thyroidectomy specimens cautions us for their prudent assessment both in gross and histopathological levels.
FINANCIAL DISCLOSURE
There are no financial supports.
ADDENDUM
Formalin fixation of fresh thyroidectomy specimen5,6,25,26,27: The specimen was immersed in 10% buffered formalin in an already labeled wide-mouth transparent plastic container after thorough was with tap water. It was then labeled with main laboratory reception ID no. and data entry of the patient.
Processing of specimen conducted at surgical Histopathology lab of Department of Pathology PMC:
The specimen was then transported to histopathology section for: Departmental coding.
Data entry of the patient departmental registry.
Specimen is then shifted to gross specimen station for the following procedure.
Replacement of fresh 10% formalin after thorough wash with tap water and first stage of gross examination and other necessary procedures.
The specimen was kept in formalin for 24 hrs at room temperature for proper fixation. The initial gross examination data was recorded in predesigned proforma. Each thyroidectomy specimen was examined in detail for gross morphology. Representative tissue sections were taken from almost all suspicious areas and at 1cm interval from the specimen according to standard gross guidelines. The specimens were processed in an auto tissue processor for 24 hrs. Paraffin embedded blocks of each tissue was prepared and 4-5 micron thin sections were used for histologic examination after staining with conventional H/E method. Detailed histopathologic examination of each section was carried out and changes were noted on already designed proforma.
Hematoxylin and eosin (H & E) staining of specimens5,6,25,26,27: Following is the method adopted for (H & E):
Removal wax: Two jars of xylol used for this purpose. In the first, the sections were kept for 1 to 2-minutes to dissolve the wax away. Residual wax was removed by transfer of sections to the next jar.1,2,8,9
Hydration: After xylol the sections were passed through graded alcohols. First the sections were kept in absolute alcohol for one minute and then transferred to 90% alcohol for one-minute and last of all in 70% alcohol for the same time.
Staining: Regressive staining method was adopted in which acid alcohol is used for differentiation after keeping the sections in Hematoxylin for 5 to 7-minutes. After differentiation the sections were dipped in ammonia water until a bright blue tingle appeared. Next the sections were kept in eosin for 2 to 4-minutes which was used as a counter stained.
Dehydration: Again graded alcohol was used in the reverse order beginning from 70% to 90% alcohol in which the sections were kept for one to two-minutes and then transferred to absolute alcohol for 2 to 3-minutes.
Clearing: Two changes of xylol were used for 2 to 3-minutes each.
Mounting: A drop of Canada balsam was placed over a cover-slip and portion of the slide containing the section was gently pressed over it so that no air bubbles were trapped.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.