OVERVIEW
Adhesive capsulitis, commonly known as “frozen shoulder,” is a condition in which a person’s shoulder range of motion is drastically limited, usually following immobilization for a variety of reasons. It occurs more often in women than men and is more likely to manifest itself in people with diabetes mellitus. While there is no specific cause/etiology of adhesive capsulitis, it frequently follows immobilization secondary to trauma, infection, or following surgery, including radical mastectomy. It most commonly affects people between the ages of 40-60 and typically has three stages: 1) freezing, where the shoulder is typically injured or infected causing an inflammatory response, and becomes immobilized, 2) frozen, in which both active and passive shoulder range of motion is significantly reduced, and 3) thawing, in which range of motion returns to near normal or to a new normal.1
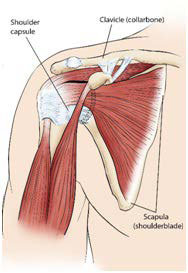
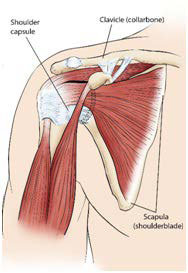
The anatomy of the shoulder, which can accommodate wide ranges of motion, makes it susceptible to injuries and, in turn, may predispose to an aberrant/restrictive articulation. It is a ballin-socket joint in which the head of the humerus (the ball) sits in the glenoid fossa of the scapula (the socket) and is being held in place by several stabilizing muscles and the shoulder capsule, made of fibrous connective tissue that surrounds the glenohumeral joint of the shoulder and prevents dislocation of the glenohumeral joint. When this capsule is injured or infected, the inflammatory process that follows causes extra fibrous tissue to be laid down around this capsule which eventually causes significant restrictions in the glenohumeral joint. Both active and passive range of motion are significantly reduced because the capsule that holds the shoulder in place has become restricted.
Treatment for adhesive capsulitis typically begins with non-steroidal anti-inflammatory drugs (NSAID) medication and physical therapy, primarily range of motion exercises to increase shoulder flexion, abduction, external rotation, and horizontal abduction/adduction. Both passive and active range of motion exercises are performed for best results. This often is a slow procedure and may not be effective. If physical therapy is not successful steroid injections may be tried to break up adhesions, but they may not be effective and may damage other tissues in the process. Another possible treatment is hydrodilatation in which sterile fluid is injected by an interventional radiologist. The concept is that the fluid will stretch the capsule and lead to increased mobility. Again this has less than predictable results. If none of these treatments works, manipulation under anesthesia may be attempted. In this treatment, the patient is placed under general anesthesia and a physician manipulates the shoulder through its full range of motion, tearing the adhesions and helping to improve range of motion. It is typically performed by an orthopedic surgeon or chiropractor with specialized training and, while it is very effective at removing adhesions, it can in some instances lead to fracture of the glenoid fossa, fracture of the humeral head, or tears of the rotator cuff muscles. Finally, arthroscopic surgery is also a common treatment, in which the surgeon will try to make incisions in the capsule to try to increase the range of motion. This, like most of the other treatments, has limited success (Figure 1).2
Figure 1. Frozen Shoulder
Since most of the common treatments have questionable success or significant possible drawbacks, many patients will opt for no treatment or live with the limited restrictions that typical physical therapy offers. Unfortunately, this can mean limitations on activities related to work or to daily activities.
CASE STUDY
A 45-year-old woman was presented with a one-year history of frozen shoulder which developed after she had run into a post with her arm outstretched. She did develop a hematoma following the injury and, when the hematoma resorbed, she was left with frozen shoulder. Diagnostic imaging demonstrated mild arthritis in her acromioclavicular joint, but not enough to limit motion. She had tried acupuncture and physical therapy with some success, but still had significantly reduced passive and active range of motion in her right shoulder. As a right hand dominant emergency physician, frozen shoulder was limiting her ability to do her work and had prevented her from playing tennis for over a year.
She was not interested in surgery or manipulation under anesthesia because of the downtime and questionable outcomes.
Upon initial examination, the patient was physically fit, active, right-handed female of south Asian descent with two children and no significant medical problems aside from the frozen shoulder. She was taking no medication aside from a multivitamin and over the counter pain medicine for her shoulder as needed. Her active right shoulder range of motion was reduced by almost 50% into flexion, extension, abduction, and external rotation and passive range of motion was only slightly better. Shoulder muscle strength was within normal limits when in neutral position, but was reduced notably when the shoulder was abducted, or flexed to 90 degrees. After reviewing imaging studies and examining the patient, it was determined that the anterior and superior portions of the capsule were restricted. There was a discussion regarding the treatment plan, including risks and likely outcomes.
METHODS
Treatment consisted of axial manipulation of the right shoulder, passive range of motion exercises, active release technique (ART) over the anterior capsule and superior capsule, acupuncture with electrical stimulation into the capsule, and at home range of motion and strengthening exercises. ART is a treatment developed by Dr. P. Michael Leahy to help break up fibrous adhesions in muscles and connective tissues to help elite athletes return to peak performance following injuries. It involves putting significant pressure over a tissue while moving it through its range of motion.3 When performed correctly, you can typically see increased range of motion within minutes. It does require a high pain tolerance from the patient, but it is very effective at increasing range of motion. ART has been used to treat many conditions including tennis elbow, plantar fasciitis, and rotator cuff injuries, but never frozen shoulder. Because of the ability to isolate the region of the shoulder capsule that was primarily affected by the adhesions, it made sense to try to break them up with ART. In this treatment, the thumb was used to put deep pressure into the shoulder capsule and used the other hand to move the shoulder through the motions of the shoulder. There was also a patient who actively moves her shoulder in all directions while putting pressure over the superior and anterior portions of the capsule. The electrical acupuncture into the same spots in the capsule was used to prevent reactive inflammation following the ART and to increase regional levels of enkephalins, endorphins, and white blood cells.4 In addition, the patient was advised to perform a standard range of motion exercises for adhesive capsulitis and gave her TheraBands and exercises to perform that would increase her strength into abduction, flexion, and external rotation so, as we increased her range of motion, we would also increase her strength and stability.
RESULTS
Our course of treatment lasted about 4-weeks and included 8 treatments. By the end of our course of treatment her active range of motion had returned to normal with minimal pain at end range of motion. While she had a little weakness in her supraspinatus she was not limited at all in her activities and was able to manage any residual pain with over the counter medication. She was able to flex her right shoulder to 175 degrees, abduct it to 180 degrees, and externally rotate to 85 degrees. Her muscle strength was normal in all ranges of motion and only caused minor pain at the onset of resisted abduction.
CONCLUSION
While ART is not a new concept and is used regularly in the practice of physical therapy and chiropractic, its use here was somewhat novel for the treatment of adhesive capsulitis. It has been shown to decrease pain and increase pain-free range of motion in patients with restrictions due to adhesions in soft tissues. Since a treatment like manipulation under anesthesia is performed to break up those adhesions in the shoulder capsule, it only makes sense that a less invasive process that can break up adhesions would likewise be effective without the risks of general anesthesia or the risks to the bony and muscular tissues of the shoulder that are associated with manipulation under anesthesia. In this case, the results were fast and successful in part due to the use of this technique and the use of acupuncture with electrical stimulation, but also because of the patients adherence to her home exercise protocols. The results of this treatment regimen would strongly suggest/promote additional trials of treatment using only ART to treat adhesive capsulitis and compare that to ART and acupuncture with electrical stimulation.
CONSENT
The authors have received written informed consent from the patient.