INTRODUCTION
Transurethral resection of the prostate (TURP) has been the gold standard in surgical interventions for Benign Prostatic Hyperplasia (BPH) and the benchmark for which other surgical therapies for BPH have been compared to for several decades. In recent years, minimally invasive techniques have been increasing in popularity. One of the most commonly used minimally invasive techniques is the use of GreenLight (AMS Research Corporation, Minnetonka, MN, USA)1,2 in the surgical management of BPH.
Largely modelled from the field of aviation, the use of simulation has become an integral part of medical training for both learning technical skills and improving communication among teammates.3,4 In resident education, appropriate use of simulators may provide residents with confidence performing a procedure in a controlled setting, which can improve outcomes and reduce variability on live patients. Simulation can shorten the learning curve and has been studied in the training of a wide range of urological procedures.5,6,7
The GreenLight simulator was developed through a University of Minnesota’s Center for Research and Education in Simulation Technologies and American Medical Systems. Introduced in 2011, it reproduces the experience of performing a GreenLight PVP.8,9,10 A study by Herlemann, et al. examined the simulator and demonstrated face, content and construct validity of the GreenLight Sim in a structured curriculum.10 Our study aims to evaluate the GreenLight Sim at two teaching hospitals utilizing a structured curriculum developed for the purpose of resident education.
MATERIALS AND METHODS
This study utilized a structured curriculum to evaluate the GreenLight Laser SimTM V2.0 (AMS Research Corporation, Minnetonka, MN, USA), in its ability to teach safety and efficiency principles to residents. The curriculum was offered to residents at two tertiary care hospitals. Resident training level ranged from Post Graduate Year 1 to Post Graduate Year 6. Residents in PGY 1 and 2 had zero experience with PVP, while residents in years PGY 3 and 4 had performed the PVP procedure less than 5 times. PGY 5 and 6 residents had the most experience with the laser, having performed greater than 20 PVP procedures. Participants were provided a curriculum checklist to follow (Table 1), including anatomy identification, fiber sweep speed, fiber-to-tissue distance and bleeding vessel coagulation. In addition, four different anatomical gland types included 30 g normal gland, median lobe, prominent apex, and a 100 g gland with trilobar hypertrophy.
| Table 1: Curriculum Structure |
|
Instructional Element
|
# Times to complete task |
Objective
|
| SIM Training Modules |
| Module 1 – Anatomy Identification |
1
|
Compete the exercise and obtain SIM score |
| Module 2 – Sweep Speed |
1
|
Compete the exercise and obtain SIM score |
| Module 3 – Tissue Fiber Distance |
1
|
Compete the exercise and obtain SIM score |
| Module 5 – Controlling Bleeders |
1
|
Compete the exercise and obtain SIM score |
| SIM Cases |
| SIM Case: 30 g Normal Gland |
3
|
Take down median lobe and one lateral lobe |
| SIM Case – Median Lobe |
3
|
Take down median lobe |
| SIM Case – Prominent Apex |
3
|
Vaporize apical tissue safely, staying away from sphincter |
| SIM Case – 100 g Trilobar Hypertrophy |
3
|
Create a working channel and take down median lobe |
| Participants were allowed 2 minutes to complete each of the four required SIM training modules and 10 minutes lasing time for each of the four SIM cases. |
Participants were given 2 minutes for each of the four required SIM training modules and 10 minutes lasing time for each of the four SIM cases.
Outcome measures included global scores, sweep speed, average laser distance, and ability to coagulate bleeding vessels were recorded using the scoring system integrated into the GreenLight Laser SimTM software. Statistical analysis was performed with SAS v9.3 (SAS Institute Inc., Cary, NC, USA). This was done with linear mixed effects models which included resident training level and number of trials completed for each outcome. All models were adjusted for repeated measures across residents.
RESULTS
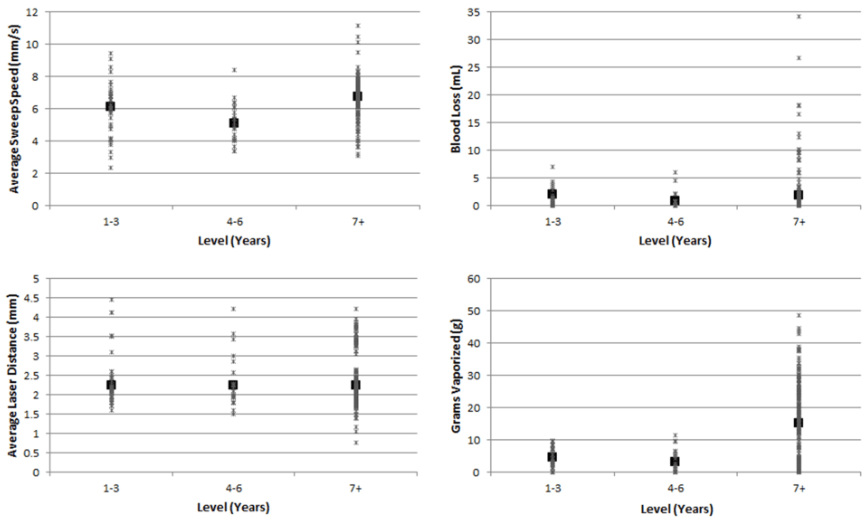
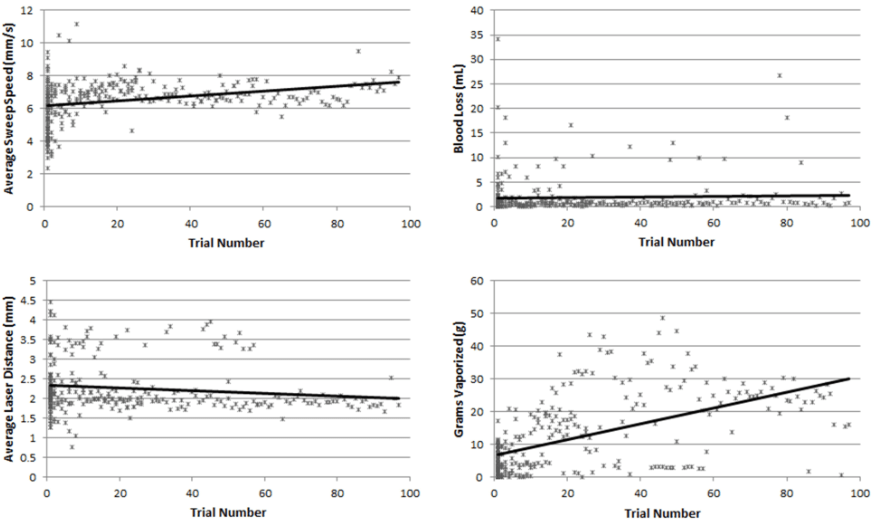
20 residents completed a total of 331 trials on the simulator. The study outcomes of sweep speed, blood loss, laser distance and grams vaporized were evaluated according to resident training level (Figure 1) and the number of trials completed (Figure 2).
Figure 1: Simulator Outcomes in each Training Level Group with Mean
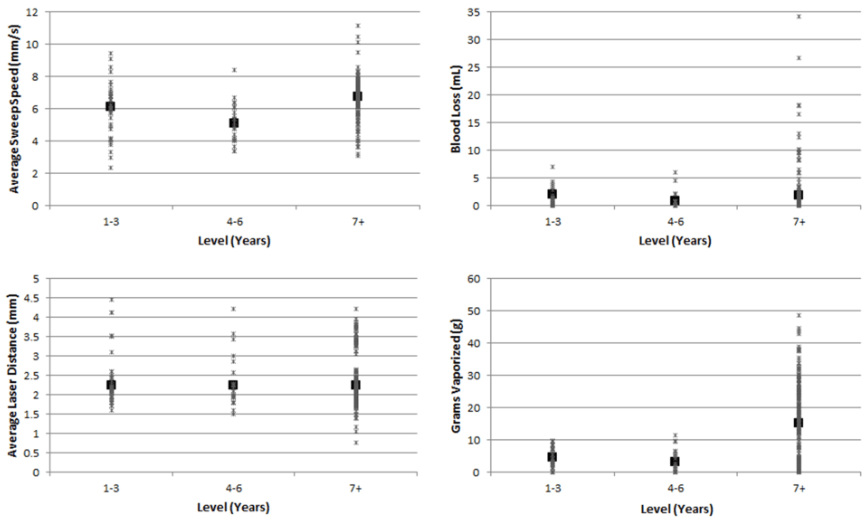
Figure 2: Simulator Outcomes Plotted against Trial Number with Linear Trend Lines
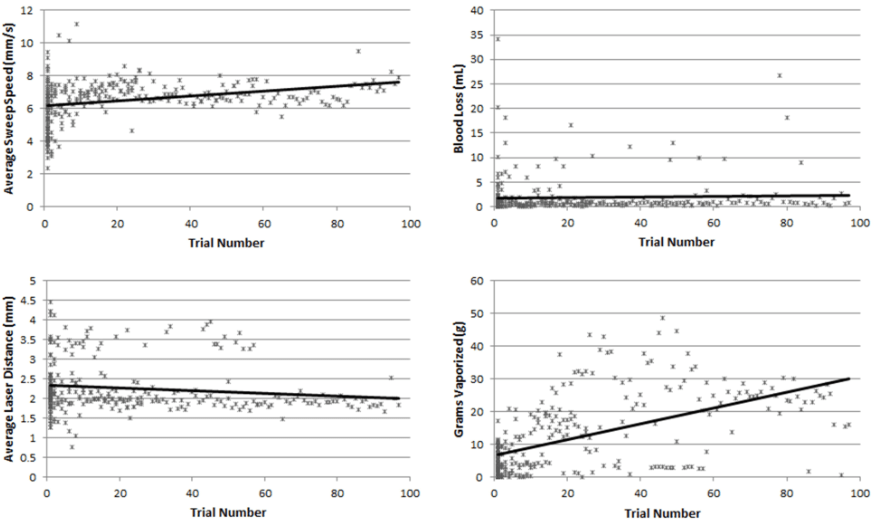
The average sweep speed across all participants was 6.51 mm/sec (Standard Deviation [SD]=1.28 mm/sec). A slight trend towards increased sweep speed was seen with both increased training level and increased number of trials, although these differences did not reach statistical significance in this study. The average blood loss was 1.84 mm/sec (SD=3.86) and this did not appear associated with either training level or number of trials completed. Average laser distance was 2.25 millimeters (SD=0.65 mm) and this did not vary significantly between the different levels of training or number of trials completed. A negative association did exist between laser to tissue distance trial number, estimate=-0.004(95% CI -0.007, -0.001). The average weight of tissue lasered during each of the simulated cases was 12.44 grams (SD=11.43 g). There was a significant increase in efficiency of vaporization with increased use of the simulator as evidenced by a greater amount of tissue vaporized per trial with increased trial number, estimate=0.191 (95% CI 0.144, 0.238). Although increased simulator use increased efficiency, resident training level was not associated with improved vaporization efficiency in this study (Table 2).
| Table 2: Model Coefficients and 95% Confidence Intervals for Simulator Outcomes |
|
Outcome
|
|
Measure
|
Average Sweep Speed |
Blood Loss |
Average Laser Distance |
Grams Vaporized
|
| Year 1-3 |
0.806(-0.288, 1.900)
|
0.335(-1.016, 1.685) |
-0.201(-0.696, 0.293) |
-2.261(-6.786, 2.264)
|
| Year 4-6 |
-0.063(-1.274, 1.148)
|
-0.835(-1.016, 1.685) |
-0.124(-0.679, 0.431) |
-3.517(-8.895, 1.861)
|
| Year 7+ |
ref. |
ref. |
ref. |
ref. |
| # of Trials |
-0.003(-0.003, -0.008)
|
0.00(-0.011, 0.027) |
-0.004(-0.007, -0.001)* |
0.191(0.144, 0.238)*
|
| *p<0.05 |
DISCUSSION
Our results indicate that the use of the GreenLight simulator in a structured training program can lead to increase in vaporization efficiency. We did not observe significant differences in the other outcome measures tested, which is possibly a reflection of the relatively short learning curve for this technique. (Figure 2) A study by Woods, et al. suggested that 15-20 cases is sufficient for a user to become proficient, while Seki et al. demonstrated that there was essentially no learning curve for this procedure when performed by two physicians with no previous experience in the use of PVP, although they had received the appropriate training and had over 10 years of experience in performing TURP.2,11 In terms of acquiring expert level proficiency, an additional study estimated that up to 120 cases may be needed to obtain expert level proficiency in the procedure.12
In line with our findings, Aydin, et al. performed a study that included 46 participants who were grouped by level of experience. Twenty-five participants were considered novice, and had no operative or endoscopic experience. Fourteen were intermediate and seven had expert level experience. According to the authors, an average of 75 procedures was required to reach expertise level, and thus participants with experience of less than 75 procedures were considered intermediate. Their study findings were such that they determined knowledge and technical skills taught by the simulator are valid for learning PVP, and should be incorporated for training purposes.13
Although recommendations regarding training for GreenLight PVP have been published based on the experience and expertise of several investigators,14,15 there is a paucity of data on the utility of the GreenLight Sim in resident education and skill acquisition. The International GreenLight User Group has recommended several key measures of proficiency in PVP including adequate background knowledge about the procedure, proper handling of the scope and probe, adequately addressing bleeding vessels, managing intra- and post-operative complications, and catheter management.14 While several studies in the field of robotic surgery have evaluated the use of structured simulator curricula in the training of surgical residents16,17 such studies are not as readily available in the literature for the teaching of PVP to residents.
This study demonstrated increased vaporization efficiency with repeated trials on the Green-Light simulator in a multi institutional cohort of 20 residents. Limitations include the retrospective nature of this study and small sample size limited by the number of residents that were available to participate in the study. Future investigations should include a larger cohort to further evaluate the GreenLight Sim as an educational tool in resident training. Additionally, future studies need to investigate the extent to which skills and efficiency developed on the simulator are carried over to the operating room.
CONCLUSIONS
The GreenLight Simulator was a useful tool to teach several key safety principles important to the PVP procedure. More clinical experience correlated with more efficient vaporization and shorter laser distance, but did not correlate with improved average sweep speed or a reduction in blood loss. The Green Light Simulator was a useful adjunct to teach important safety elements of the PVP procedure.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.