INTRODUCTION
Secondary hypogammaglobulinemia (IgG<600 mg/dL) occurs for a variety of reasons, including due to disease, drugs, or treatment. In particular, in hematological malignancies (chronic lymphocytic leukemia, multiple myeloma, malignant lymphoma, etc.), the frequency of onset of secondary hypogammaglobulinemia is also high, and this is important for the onset of infections. Specifically, malignant lymphoma is a representative hematologic malignancy that is associated with secondary hypogammaglobulinemia due to chemotherapy, including rituximab. Although not abundant, there have been a few reports on malignant lymphomas and hypogammaglobulinemia. Filanovsky et al1 reported that 49% and 11% of 182 malignant lymphoma patients treated with chemotherapy developed hypogammaglobulinemia with immunoglobulin G (IgG) 600 mg/dL or less and with IgG 400 mg/dL or less (severe), respectively. Particular attention was paid to the finding of higher mortality rates due to infections in the low gamma globulin group (32%) than in the normal group (3.6%), and the mortality rate was higher in patients with hypogammaglobulinemia that continued for 6-months or longer than in patients with hypogammaglobulinemia continuing for 6-months or less.1 In addition, Memorial Sloan-Kettering Cancer Center (MSKCC) also reported on hypogammaglobulinemia in patients with malignant lymphomas. The association between the use of rituximab and hypogammaglobulinemia (IgG<600 mg/dL) in malignant lymphomas treated with rituximab between December 1998 and September 2009 was investigated. The study included 211 patients with malignant lymphomas. Although 15% of patients presented with hypogammaglobulinemia prior to treatment, 38.5% of patients who had normal IgG prior to treatment presented with hypogammaglobulinemia after treatment and 72% of patients with IgG within or below normal limits prior to treatment presented with hypogammaglobulinemia after treatment, meaning overall 43% experienced onset.2 Hypogammaglobulinemia in malignant lymphoma increases the risk of complications of infections and is associated with increased mortality from infections and interruption of chemotherapy. In order to improve treatment outcomes for malignant lymphomas, there is a necessity to pay attention to hypogammaglobulinemia. We therefore, investigated the risk of hypogammaglobulinemia and infection in patients with malignant lymphomas at our hospital.
PATIENTS AND METHODS
A retrospectively analysis of data from medical records of patients with malignant lymphomas whose IgG levels were measured and who received rituximab-containing therapy at our hospital between April 2014 and March 2016 was performed. Hypogammaglobulinemia was defined as an IgG value of 600 mg/dL or less, and an IgG value of 400 mg/dL or less was defined as severe hypogammaglobulinemia. To assess the risk of infection, IgG levels and hospitalization for and deaths due to infection were studied in patients hospitalized for infection during this period.
RESULTS
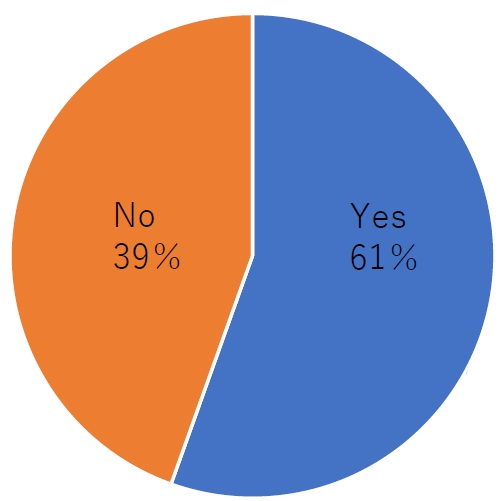
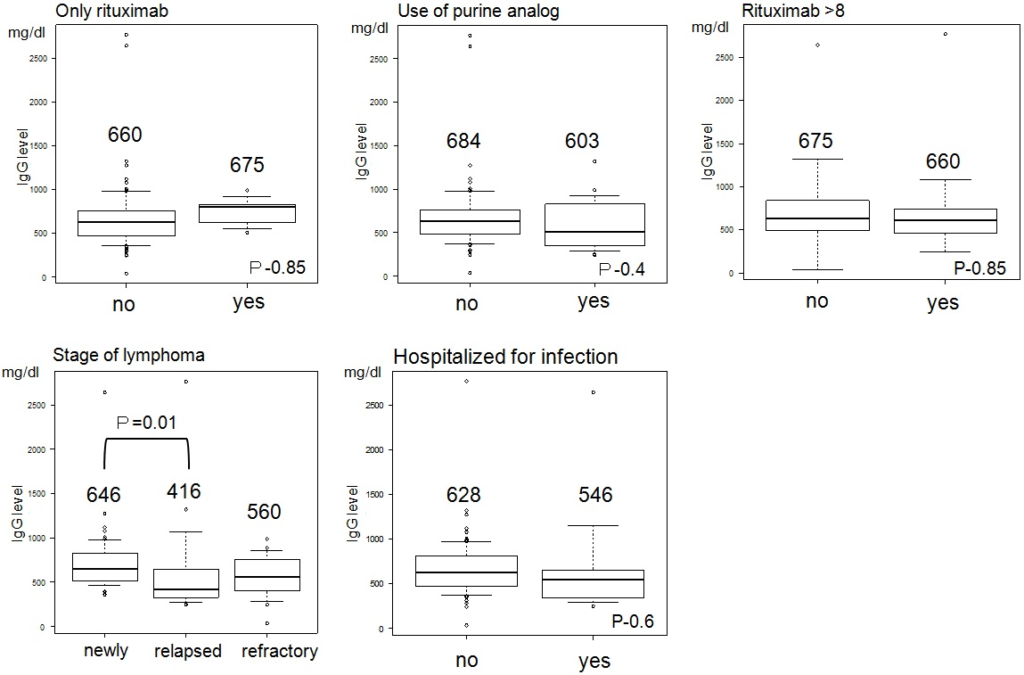
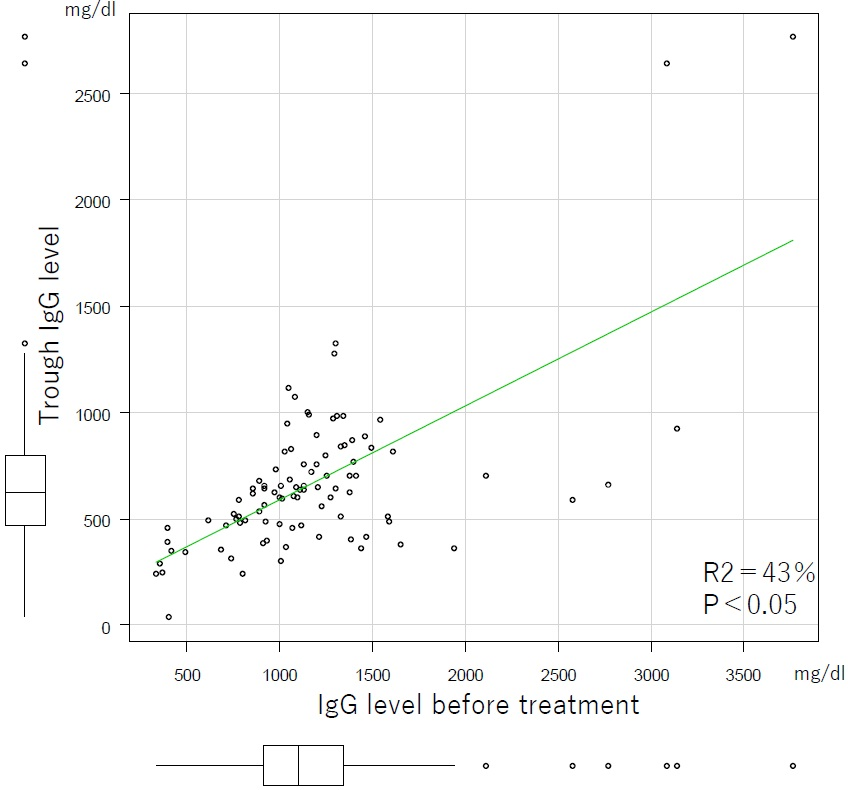
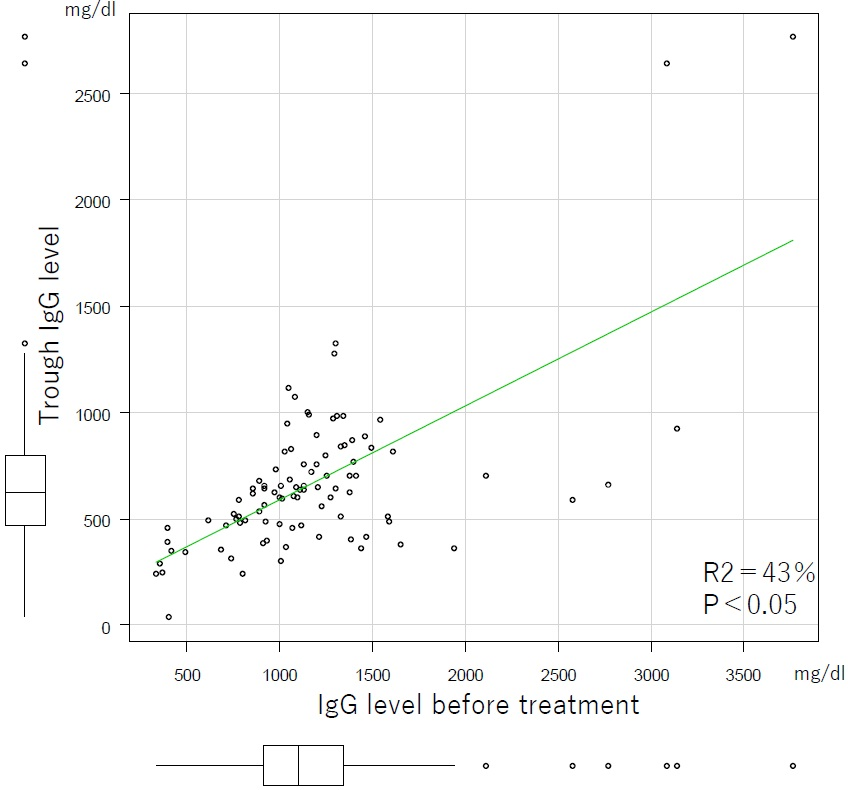
From April 2014 to March 2016, 128 patients with malignant lymphomas received rituximab-containing therapy at our hospital, and 94 (61%) of these patients had IgG levels measured (Figure 1). The 94 patients shown in Table 1 were included in analyses. The histological types were as follows: 30 had follicular lymphoma (FL), 17 had indolent non-Hodgkin’s lymphoma (iNHL), 42 had diffuse large B-cell lymphoma (DLBCL), and 5 had mantle cell lymphoma (MCL). There were 60 patients with primary, 16 with recurrent, and 18 with refractory disease. Eighteen patients used purine analogues. Eight patients (8%) presented with hypogammaglobulinemia prior to treatment. Four of these patients (4%) had severe hypogammaglobulinemia. After treatment, 42 patients (44%) presented with hypogammaglobulinemia and 18 (19%) had severe hypogammaglobulinemia. Nine patients (10%) were hospitalized for infection. Relationships between rituximab monotherapy/combination therapy, use/non-use of purine analogues, 1/2/3 prior regimens, completion/non-completion of 8 or more administrations of rituximab and minimum IgG levels were investigated. The mean values of each item were shown in Figure 2. The risk of infection was assessed based on the relationship between hospitalization for infection and minimum IgG levels. The mean minimum IgG level in patients hospitalized for infection was 546 mg/dL and 628 mg/dL in those not hospitalized (p=0.6) (Figure 2). There was no significant difference in the relationship between hospitalization for infection and hypogammaglobulinemia and severe hypogammaglobulinemia (p=0.383/0.059). And there was a significant difference in the relationship between death from infection and severe hypogammaglobulinemia, but not hypogammaglobulinemia (p=0.00264/0.133). The types of infections were as follows: pneumonia in 5, enteritis in 1, peritonitis in 1, herpes zoster in 1, and infection of unknown etiology in 2 patients. Four patients died, two of whom died from infections, while the other 2 died from underlying malignant disease. In addition, there were 4 patients with mean IgG levels that were 600 mg/dL or less in the 6-months immediately prior to hospitalization (Table 2). Among these 2 (50%) died of infection. Moreover, in terms of minimum IgG levels, a lower IgG value prior to treatment was significantly associated (p<0.05) with a low IgG post-treatment value (Figure 3).
Figure 1. The Monitoring Ratio of IgG Level
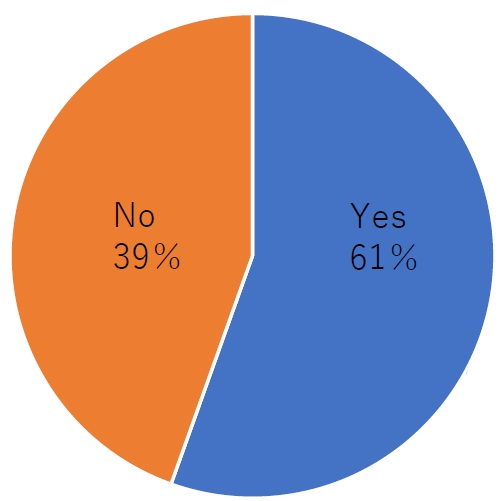
Table 1. Patient Characteristics
|
N
|
94
|
| Age, median(range) |
70(46-87)
|
| Sex |
| Male |
53(56%)
|
| Female |
41(44%)
|
| Lymphoma type |
| FL |
30(32%)
|
| iNHL |
17(18%)
|
| DLBCL |
42(45)
|
| Mantle |
5(5%)
|
| Pre-Treatment |
| low IgG |
8(8%)
|
| Fludarabine-base chemo |
17(18%)
|
| Rituximab cycle>8 |
36(38%)
|
| Prior therapy |
| 1 |
16(17%)
|
| 2 |
18(19%)
|
| Stage |
| Newly |
60(64%)
|
| Relapsed |
16(17%)
|
| Refractomy |
18(19%)
|
| In parentheses indicates Account for a percentage |
Figure 2. IgG Levels in Each Item
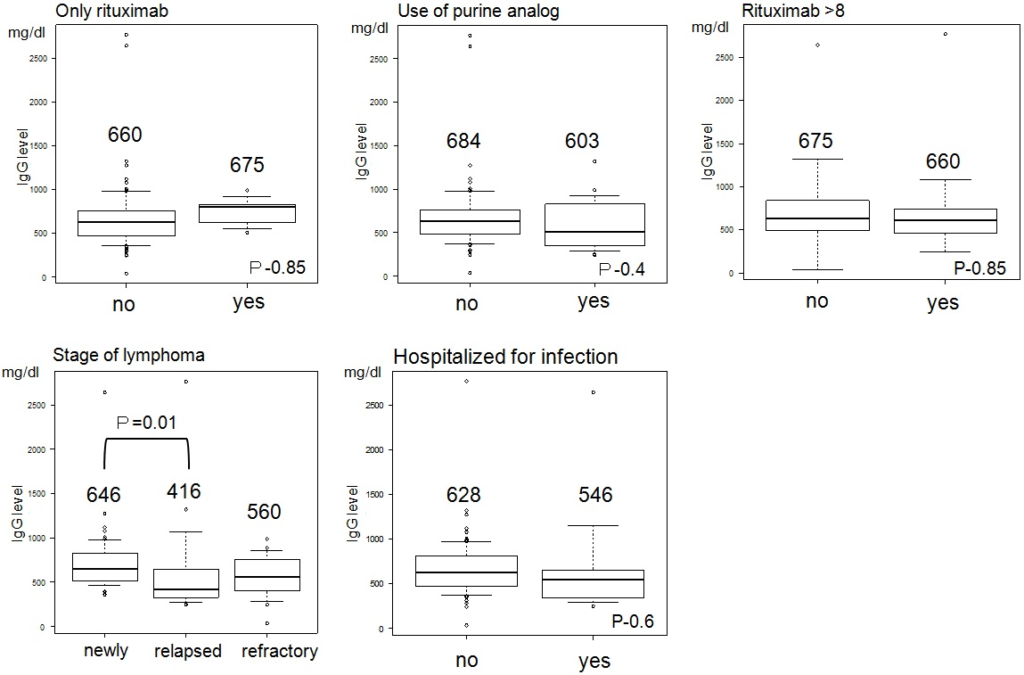
Table 2. Type of Infection and IgG Average
| ID |
Age
|
Type
|
Sex
|
Infection
|
Survival
|
Infection-Related Death
|
IgG Average
|
|
1
|
74
|
SLL
|
F
|
Pneumonia |
Alive
|
|
413
|
|
2
|
63
|
DLBCL
|
F
|
Herpes encephalitis |
Death
|
No
|
288
|
|
3
|
55
|
FL
|
M
|
CMV pneumonia |
Death
|
Yes
|
411
|
|
4
|
75
|
DLBCL+RA
|
F
|
Sepsis |
Alive
|
|
3248
|
|
5
|
79
|
DLBCL
|
F
|
CMV pneumonia |
Death
|
Yes
|
353
|
|
6
|
79
|
FL
|
M
|
Febrile Neutopenia |
Alive
|
|
1202
|
|
7
|
70
|
DLBCL
|
M
|
peritonitis/Febrile Neutopenia |
Alive
|
|
1014*
|
|
8
|
73
|
DLBCL
|
F
|
Cholecystitis |
Death
|
No
|
1902*
|
|
9
|
53
|
DLBCL
|
M
|
Pneumocystis pneumonia |
Alive
|
|
799
|
| *is less than 6 months close to the first visit and hospitalization |
Figure 3. The Relationship between the IgG Level Before Treatment and the Lowest IgG (trough IgG)
DISCUSSION
Rituximab is an antibody that targets CD20 and reduces B-cells. As a consequence, IgG values also decrease. In our study, the rate of hypogammaglobulinemia increased from 8% prior to treatment to 44% after rituximab administration. Monitoring of IgG levels during rituximab administration may be necessary; however, only 61% of the patients had IgG measured at our hospital. Since hypogammaglobulinemia is associated with a risk of infection, monitoring of IgG levels is considered important. In terms of the association between hematologic malignancies and hypogammaglobulinemia, Furst reported the onset of infections in association with chronic lymphocytic leukemia (CLL) and serum IgG levels. The onset of infection reportedly increases in CLL when IgG values are 600 mg/dL or less, and that the onset of severe infections increase with lower IgG values.3 Makatsori also reported on the risks of hypogammaglobulinemia following the administration of rituximab. Twenty-seven percent of patients reportedly developed hypogammaglobulinemia after treatment. Forty-one events of infections were observed, with 10 events of bronchitis/pneumonia and frequent onset of respiratory tract infections.4 Vacca also reported on hypogammaglobulinemia in multiple myeloma. In this report, there was also a frequent onset of upper respiratory tract infection observed.5 These findings suggest that hypogammaglobulinemia is associated with a high risk of respiratory tract infections and that IgG levels should be checked when there are complications of upper respiratory inflammation during chemotherapy. In addition, Filanovsky reported that low gamma globulin levels influenced death from infections in malignant lymphomas.1 In this report, 182 malignant lymphoma patients were analyzed, and the onset of hypogammaglobulinemia was observed in 38%. The mortality rate with infections was 3.6% versus 28.5% in patients with normal versus decreased IgG levels (IgG≤600 mg/dL) and was significantly higher in patients with decreased IgG levels than in those with normal IgG levels. In addition, patients whose hypogammaglobulinemia persisted for 6-months or longer had a higher mortality rate of 19% compared to 6% in those whose hypogammaglobulinemia did not persist, suggesting that the long-term persistence of hypogammaglobulinemia was associated with a higher mortality rate. We investigated infections and deaths in patients hospitalized for infections during this period in this study (Table 2). The types of infection were as follows: 4 patients with pneumonia, 2 patients with febrile neutropenia (FN), and 1 patient each with cholecystitis, encephalitis, septicemia, and peritonitis. Similar to previous reports, there were many patients with pneumonia and other respiratory infections. Severe hypogammaglobulinemia had a dominant difference and increases mortality from infection, but the risk of death from infection is related not only to IgG levels but also to duration. There were 4 (44%) deaths, but 2 (22%) were due to infections in this report. In these 2 patients, the mean IgG level was 382, low-level, during 6-months prior to hospitalization. In patients with mean IgG values of 600 mg/dL or less, 2 (50%) out of 4 died from infections. Caution should be exercised because persistent hypogammaglobulinemia may increase the risk of death from infections. In addition, post-treatment hypogammaglobulinemia increased from 8% to 44%, and thus caution should be exercised and IgG levels monitored after treatment.
CONCLUSION
In this study, rituximab-containing chemotherapy was found to increase the risk of post-treatment hypogammaglobulinemia in patients with malignant lymphomas. Several authors have made similar observations as our study, on the basis of which the Rituximab Consensus Expert Committee recommends pretreatment screening for hypogammaglobulinemia so appropriate caution may be exercised.6 In addition, the persistence of hypogammaglobulinemia was associated with an increased risk of developing infections, and high rates of mortality. The risks associated with hypogammaglobulinemia in malignant lymphomas should be understood and treatment should be administered. There is also a need to consider the indications for prevention, such as with substitution therapy of gamma globulin in the future, and further evaluations are necessary.
IRB APPROVAL
This study has been approved by the Institutional Review Board (IRB).
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.