INTRODUCTION
Sleep is an important biological process that affects both physical and mental health. Modern-day stressors and technology have led to certain behavior patterns that have become an active threat to sleep. The 2021 Philips Global Sleep Survey conducted among 13,000 individuals of ages 18 and above, across 13 countries (South East Asian and European countries, US and Australia), reported that 76% of adults reported having one or more sleep issues; with stress being the most reported hurdle. These sleep challenges were further exacerbated by the pandemic. The survey also pointed out that, 37% of adults experienced insomnia and 62% of adults felt they don’t sleep well.1 A study conducted among 10,220 adolescents (16-19-years) in Norway found that 23.8% reported experiencing insomnia.2 Generation Z (Gen Z) (1997-2013) has been dubbed the generation that never sleeps and only 15% of Gen Z felt that they get enough sleep.3 A survey in the US conducted by the American Academy of Sleep Medicine among 2,010 individuals found that almost 93% of Gen Z stayed up late; because of their phones and social media usage.4
These prolonged periods of low quality and quantity of sleep are related to increased risk of cardiovascular diseases, irritability, low moods, fatigue, suicide risk, lapses in attention, sleepiness during the day, work and car accidents, burnout, obesity, etc.5 To understand sleep disturbances, it is first important to understand circadian cycles. During 24-hours, there are certain physiological (hormone secretions) and behavioral processes, that primarily respond to and are in sync with light and darkness that contribute to our sleep-wake cycle. The suprachiasmatic nucleus of the hypothalamus is the center of the brain that controls this. During darkness there is reduced capability and alertness, increased melatonin secretion, and a dip in core body temperature. Whereas light is associated with alertness, performance, and a rise in body temperature. So, when we work or sleep against these schedules, it leads to circadian dysregulation.6 The article will discuss certain environmental factors and behaviors which have led to circadian dysregulation and the resultant secondary anxieties.
Gen Z who are already grappling with high mental health concerns already lead to sleep disturbances. To add to this, Gen Z will in the near future enter the workforce where always-on culture and shift work will further disrupt sleep cycles. The phenomenon of always-on culture has come about with the advent of heavy technological use in workplaces (mail, messaging), where companies expect employees to be present even after their working hours checking mail and attending calls. The second factor of night shift work also goes against circadian cycles. This had led to Shift Work Sleep Disorder characterized by insomnia, associated with work accidents, moodiness, irritability, etc., and this is especially because daytime sleep does not give the same relaxation as night sleep due to the biological and behavioral aspects associated with light. Daytime sleep is also known to be shorter without deep relaxation.
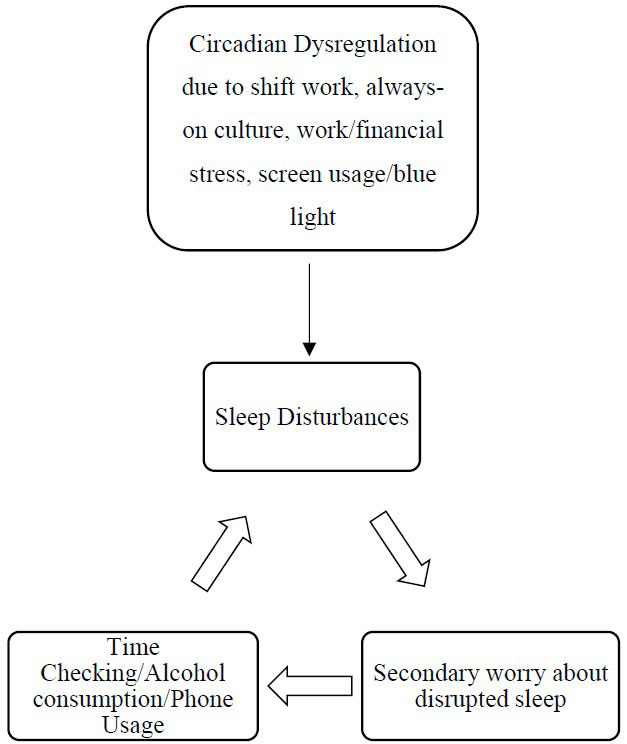
Further, technology and its consequent behaviors, have also led to circadian dysregulation. They are Smart Phone and Social Media usage, television (TV) and light-emitting diode (LED) lights. The addictive nature of social media and blue light emanating from screens lead to sleep phase disruptions. As blue lights from screens and LED lights are associated with melatonin suppression (melatonin produces drowsiness), increased attention, and activation. A lot of the time this leads to students feeling that they are more productive at night, losing out on sleep, and experiencing fatigue and burnout (resulting in less time to replenish mental resources). Other factors triggering sleep disruption are obesity and substance use. Levels of obesity have been on the rise due to complex interactions between biological and environmental (dietary habits, increased deskbound activities, etc.) factors. The causal relationship between sleep and obesity is bi-directional, but many have suggested caution when making definitive statements. Only further research can clarify.6 Regarding substance use, alcohol has only short-term effects on sleep and as a consequence leads to broken sleep, decreased quality of sleep and hangovers. Lastly, with anxiety, stressful events on the rise, rumination, negative automatic thoughts (NATs) (NATs are negative thoughts or self-talk that appear after an event), and intrusive thoughts are increasingly being observed among Gen Z, all of which lead to sleep disruptions. Secondary worry about sleep challenges and time checking through the night further contributes to the exacerbation of sleep disruptions. All this has led to insomnia, broken sleep, decreased quality of sleep, delayed sleep phase syndrome (DSPS), etc (Figure 1)
Figure 1. Representation of Modern-Day Contributors of Sleep Disturbance and the Vicious Cycle of Sleep Disturbance Due to Secondary Anxiety about Sleep and Consequent Behaviors
RECOMMENDATIONS
Combined efforts of systemic changes in workplace and education systems are necessary for effective sleep hygiene. Companies and schools must pay attention to practices that are perpetuating mental health concerns and make changes that can help in offsetting some of the effects of sleep. DSPS is a common occurrence, where delays in sleep phases are far out of what is considered normal. Chronotherapy, which is an amalgam of sleep hygiene, timed light exposure/bright light exposure and chronobiotic medications to adjust the sleep/wake cycle has produced effective results.
Since circadian rhythms are in sync with light/darkness, hence timed light exposure can be helpful. Exposure to bright light during the mornings and limited light exposure and chronobioic medications (melatonin) in the evenings can be helpful. Limited light exposure can include setting screen times for phone/social media, TV, and installing red light emitting lamps that don’t disrupt circadian rhythms can be put on during late evenings. Timed light exposure needs to be tailor-made to each client based on their sleep phases and delays.
Certain routines can also help; having the same sleep/ wake schedule, can be helpful. Winding down half an hour before going to bed, which can include reading books (not mystery books that lead to curiosity and alertness), listening to soothing music preferably without lyrics, taking a bath, aiding in reducing core body temperature, red light exposure and avoiding blue light exposure can tick off biological processes that aid in sleep. Bedroom should only be associated with sleep and not with anything else, meaning avoidance of TV and phones in bedroom. Making sure the room is dark with appropriate temperature, comfortable pillow and mattresses before you enter the room to sleep is also helpful.
Anxiety, worry, stress leads to cortisol production triggering fight, flight that increases alertness and wakefulness. It then becomes important to relax; some of the best methods to use are progressive muscle relaxation and mindfulness followed by setting a concrete time and day to deal with each worry. One can list all the worries and write date and time against each worry. This helps in realizing that worries can be dealt with, which can help in relaxation. Often times bedroom may come to be associated with dread and anxiety in case of prolonged sleep disturbances such as insomnia, coupled with secondary anxiety in the form of Negative Automatic Thoughts, why me thoughts, catastrophizing and their resultant counterintuitive behaviors. For this, it becomes important to seek psychotherapy. It can help in identifying root causes for sleep disturbances along with the perpetuating factors (cognitive and behavioral) and also help in re-framing NATs and other associated cognitive distortions, while aiding in practicing sleep hygiene. The therapeutic approach of Mindfulness based Cognitive Behavior Therapy (M-CBT) can be especially helpful in these matters. Although sleep is affected due to modern day contributions, it is in our power and ability to obtain adequate seep.



Psychology and Cognitive Sciences
Open journal
ISSN 2380-727X
Modern-Day Contributors to Sleep Disturbances in Generation Z: A Look at Chronotherapy and Other Solutions
Aaradhana Reddy*
Aaradhana Reddy, MSc
Counselling Psychologist, Safe Space Counselling, 585/a Road No.32, Jubilee Hills, Hyderabad, TS 500033, India; E-mail: aaradhanaboddureddy@gmail.com
INTRODUCTION
Sleep is an important biological process that affects both physical and mental health. Modern-day stressors and technology have led to certain behavior patterns that have become an active threat to sleep. The 2021 Philips Global Sleep Survey conducted among 13,000 individuals of ages 18 and above, across 13 countries (South East Asian and European countries, US and Australia), reported that 76% of adults reported having one or more sleep issues; with stress being the most reported hurdle. These sleep challenges were further exacerbated by the pandemic. The survey also pointed out that, 37% of adults experienced insomnia and 62% of adults felt they don’t sleep well.1 A study conducted among 10,220 adolescents (16-19-years) in Norway found that 23.8% reported experiencing insomnia.2 Generation Z (Gen Z) (1997-2013) has been dubbed the generation that never sleeps and only 15% of Gen Z felt that they get enough sleep.3 A survey in the US conducted by the American Academy of Sleep Medicine among 2,010 individuals found that almost 93% of Gen Z stayed up late; because of their phones and social media usage.4
These prolonged periods of low quality and quantity of sleep are related to increased risk of cardiovascular diseases, irritability, low moods, fatigue, suicide risk, lapses in attention, sleepiness during the day, work and car accidents, burnout, obesity, etc.5 To understand sleep disturbances, it is first important to understand circadian cycles. During 24-hours, there are certain physiological (hormone secretions) and behavioral processes, that primarily respond to and are in sync with light and darkness that contribute to our sleep-wake cycle. The suprachiasmatic nucleus of the hypothalamus is the center of the brain that controls this. During darkness there is reduced capability and alertness, increased melatonin secretion, and a dip in core body temperature. Whereas light is associated with alertness, performance, and a rise in body temperature. So, when we work or sleep against these schedules, it leads to circadian dysregulation.6 The article will discuss certain environmental factors and behaviors which have led to circadian dysregulation and the resultant secondary anxieties.
Gen Z who are already grappling with high mental health concerns already lead to sleep disturbances. To add to this, Gen Z will in the near future enter the workforce where always-on culture and shift work will further disrupt sleep cycles. The phenomenon of always-on culture has come about with the advent of heavy technological use in workplaces (mail, messaging), where companies expect employees to be present even after their working hours checking mail and attending calls. The second factor of night shift work also goes against circadian cycles. This had led to Shift Work Sleep Disorder characterized by insomnia, associated with work accidents, moodiness, irritability, etc., and this is especially because daytime sleep does not give the same relaxation as night sleep due to the biological and behavioral aspects associated with light. Daytime sleep is also known to be shorter without deep relaxation.
Further, technology and its consequent behaviors, have also led to circadian dysregulation. They are Smart Phone and Social Media usage, television (TV) and light-emitting diode (LED) lights. The addictive nature of social media and blue light emanating from screens lead to sleep phase disruptions. As blue lights from screens and LED lights are associated with melatonin suppression (melatonin produces drowsiness), increased attention, and activation. A lot of the time this leads to students feeling that they are more productive at night, losing out on sleep, and experiencing fatigue and burnout (resulting in less time to replenish mental resources). Other factors triggering sleep disruption are obesity and substance use. Levels of obesity have been on the rise due to complex interactions between biological and environmental (dietary habits, increased deskbound activities, etc.) factors. The causal relationship between sleep and obesity is bi-directional, but many have suggested caution when making definitive statements. Only further research can clarify.6 Regarding substance use, alcohol has only short-term effects on sleep and as a consequence leads to broken sleep, decreased quality of sleep and hangovers. Lastly, with anxiety, stressful events on the rise, rumination, negative automatic thoughts (NATs) (NATs are negative thoughts or self-talk that appear after an event), and intrusive thoughts are increasingly being observed among Gen Z, all of which lead to sleep disruptions. Secondary worry about sleep challenges and time checking through the night further contributes to the exacerbation of sleep disruptions. All this has led to insomnia, broken sleep, decreased quality of sleep, delayed sleep phase syndrome (DSPS), etc (Figure 1)
Figure 1. Representation of Modern-Day Contributors of Sleep Disturbance and the Vicious Cycle of Sleep Disturbance Due to Secondary Anxiety about Sleep and Consequent Behaviors
RECOMMENDATIONS
Combined efforts of systemic changes in workplace and education systems are necessary for effective sleep hygiene. Companies and schools must pay attention to practices that are perpetuating mental health concerns and make changes that can help in offsetting some of the effects of sleep. DSPS is a common occurrence, where delays in sleep phases are far out of what is considered normal. Chronotherapy, which is an amalgam of sleep hygiene, timed light exposure/bright light exposure and chronobiotic medications to adjust the sleep/wake cycle has produced effective results.
Since circadian rhythms are in sync with light/darkness, hence timed light exposure can be helpful. Exposure to bright light during the mornings and limited light exposure and chronobioic medications (melatonin) in the evenings can be helpful. Limited light exposure can include setting screen times for phone/social media, TV, and installing red light emitting lamps that don’t disrupt circadian rhythms can be put on during late evenings. Timed light exposure needs to be tailor-made to each client based on their sleep phases and delays.
Certain routines can also help; having the same sleep/ wake schedule, can be helpful. Winding down half an hour before going to bed, which can include reading books (not mystery books that lead to curiosity and alertness), listening to soothing music preferably without lyrics, taking a bath, aiding in reducing core body temperature, red light exposure and avoiding blue light exposure can tick off biological processes that aid in sleep. Bedroom should only be associated with sleep and not with anything else, meaning avoidance of TV and phones in bedroom. Making sure the room is dark with appropriate temperature, comfortable pillow and mattresses before you enter the room to sleep is also helpful.
Anxiety, worry, stress leads to cortisol production triggering fight, flight that increases alertness and wakefulness. It then becomes important to relax; some of the best methods to use are progressive muscle relaxation and mindfulness followed by setting a concrete time and day to deal with each worry. One can list all the worries and write date and time against each worry. This helps in realizing that worries can be dealt with, which can help in relaxation. Often times bedroom may come to be associated with dread and anxiety in case of prolonged sleep disturbances such as insomnia, coupled with secondary anxiety in the form of Negative Automatic Thoughts, why me thoughts, catastrophizing and their resultant counterintuitive behaviors. For this, it becomes important to seek psychotherapy. It can help in identifying root causes for sleep disturbances along with the perpetuating factors (cognitive and behavioral) and also help in re-framing NATs and other associated cognitive distortions, while aiding in practicing sleep hygiene. The therapeutic approach of Mindfulness based Cognitive Behavior Therapy (M-CBT) can be especially helpful in these matters. Although sleep is affected due to modern day contributions, it is in our power and ability to obtain adequate seep.
1. Philips. Philips global sleep survey shows we want better sleep, but only if it comes easily. Website. https://www.philips.com/a-w/about/news/archive/standard/news/press/2019/20190307-philips-global-sleep-survey-shows-we-want-better-sleep-but-onlyif-it-comes-easily.html. Published March 7, 2019. Accessed March 13, 2023.
2. Donskoy I, Loghmanee D. Insomnia in adolescence. Med Sci (Basel). 2018; 6(3): 72. doi: 10.3390/medsci6030072
3. Hassett A. The Relationship between Sleep Duration and Optimism Levels in Generation Z Students. [honors thesis]. Statesboro, Georgia, USA: Georgia Southern University; 2019.
4. American Academy of Sleep Medicine™. Are you TikTok Tired? 93% of Gen Z admit to staying up past their bedtime due to social media. Website. https://aasm.org/are-you-tiktok-tired-93-of-genz-admit-to-staying-up-past-their-bedtime-due-to-social-media/. Published September 7, 2022. Accesses April 22, 2023.
5. Chattu VK, Manzar D, Kumary S, et al. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2019; 7(1): 1. doi: 10.3390/healthcare7010001
6. Shochat T. Impact of lifestyle and technology developments on sleep. Nat Sci Sleep. 2012; 4: 19-31. doi: 10.2147/NSS.S18891
LATEST ARTICLES
Study on Major Health and Constraints of Backyard and Commercial Poultry Production in Hawassa and Yirgalem Town, Southern Ethiopia
Amanuel P. Beta, Dereje Abera, Legese Belayneh and Isayas A. Kebede
doi.
Unraveling the Mysteries of Type-A Aortic Dissection Using POCUS/Echocardiography
Syeda Rukh*, Sathyanarayana Machani and Milind Awale
doi.
Do they Play or Flirt? ‘Pawsitive’ Correlations of Castration Status and Social Behaviour of Male Dogs (Canis lupus familiaris): Video Analyses and Questionnaires
Carina A. Kolkmeyer* and Udo Gansloßer
doi.
Assessment of Hygienic Practice, Isolation and Antimicrobial Susceptibility Test of E. coli from Honey Bees Farms in and Around Haramaya University and Haramaya Woreda, Ethiopia
Ahmedyasin M. Aliyi*, Adem Hiko, Abdallahi Abdureman and Mohammedkemal M. Ame
doi.
Employee Retention Model for the IT/ITES Sector: Embed your Employees through C.A.R.E and Retain them
Tanvi Chaturvedi*
doi.
Hypertriglyceridemia-Induced Pancreatitis: A Case Report and Literature Review
Maarten Bulterys, Melvin Willems* and Agnes Meersman
doi.
From Neck Pain to a Life-Threatening Condition: A Case Report
Floris Vandewoude* and Sören Verstraete
doi.
Facial Rejuvenation and Patients Satisfaction with the Fourth Generation of Aptos P(LA/CL)–Hyaluronic Acid Threads: A 12-Month Study
Albina Kajaia*
doi.
Effective Management of Refractory Folliculitis Decalvans Using Secukinumab
Adel Al-Santali and Wasan Al-Qurashi*
doi.
LATEST ARTICLES
Cross Sectional Study
2024 Jul
Study on Major Health and Constraints of Backyard and Commercial Poultry Production in Hawassa and Yirgalem Town, Southern Ethiopia
Case Report
2024 Jul
Unraveling the Mysteries of Type-A Aortic Dissection Using POCUS/Echocardiography
Original Research
2024 Jul
Do they Play or Flirt? ‘Pawsitive’ Correlations of Castration Status and Social Behaviour of Male Dogs (Canis lupus familiaris): Video Analyses and Questionnaires